1. Introduction
Inborn errors of metabolism (IEMs) are a diverse group of more than 1 000 genetic disorders resulting in reduced activity of an enzyme, structural protein, or transporter molecule in a metabolic pathway (1). Although the incidence of each specific disease is rare, collectively IEMs are common and affect 1 in 800 live births (1, 2). The signs and symptoms of these disorders are due to the defect in a metabolic pathway and the aggregation of the defective pathway's metabolites, which are poisonous or can cause cell destruction. Additionally, the lower-path metabolite deficiency is effective in disease pathogenesis. This pathogenesis can affect one or more systems (2-4). Inborn errors of metabolism have a substantial contribution to intellectual disability, seizure, metabolic acidosis, hyperammonemia, ataxia, coma, liver damage, cataract, kidney failure, kidney cyst, cardiomyopathy, pericarditis, sudden infant death syndrome (SIDS), neurologic disorders in children (5).
Children with chronic diseases have complex care needs (6, 7). Inborn errors of metabolism are categorized as rare and chronic conditions that need lifelong support, protection, care, and treatment (4, 8). Caring for a child with IEMs requires specific and lifelong dietary management, which requires constant planning, monitoring, and measurement of the child's daily nutritional intake (1). Moreover, there might be additional management requirements, such as medical appointments, frequent blood tests, occupational therapy, and speech therapy (1, 9). Additionally, these children have psychological problems, such as anxiety, depression, social isolation, and low self-confidence (10). Their quality of life is lower than that of their peers (11, 12), and they frequently experience a sense of loss that results in chronic sorrow (12). Their parents and caregivers’ physical, psychological, and social health is also affected (13, 14). These diseases increase parenteral and familial stress, and the more parenteral stress, the less psychological parent-child psychological adjustment (13). Parents experience depression, sleep disorders, and low quality of life and have more struggles than other families (14).
Despite the above-mentioned challenges that children and families face, there are few and scattered studies about different aspects of caring for children with IEMs, and most are focused on the diagnosis, screening, and treatment methods of IEMs. There is no study examining the unmet needs of parents and children with IEMs; only there are few studies assessing the experience of caring for children with a specific type of IEM. For example, Somanadhan and Larkin assessed the parents' experience of caring for a child with mucopolysaccharidosis (MPS) and observed that parents tend to be active in caring. They felt that they were living in an ambiguous space due to the prognosis of their child's disease (13). In another study, Shirdelzade et al. showed that parents forgot themselves in the shadow of satisfying the needs of their children (15). Therefore, it is decided to conduct an integrative review to assess the care needs of children with IEMs and their parents to provide more information for planning care in healthcare systems.
2. Materials and Methods
This is an integrative review of scientific published literature. This integrative review summarizes past literature to achieve a comprehensive understanding of an issue. Therefore, it is able to build the science, research, practice, and policies of nursing (16). The development of this study is based on Whittemore and Knafl's (2005) method to increase the rigor of the review. This is a modified version of Cooper's (1998) framework, which consists of five stages: Problem identification, literature search, data evaluation (quality appraisal), data analysis, and findings presentation (17). The two later stages were presented as results and discussion.
2.1. Problem Identification
The purpose of this integrative review is to identify the care needs of children with IEMs and their parents. Clarifying these needs can be helpful in programming care plans and implementing patient-centered and multidisciplinary approaches. Therefore, all published documents in English and Persian were searched to answer this question: "What are the care needs of children with IEMs and their parents?"
2.2. Literature Search
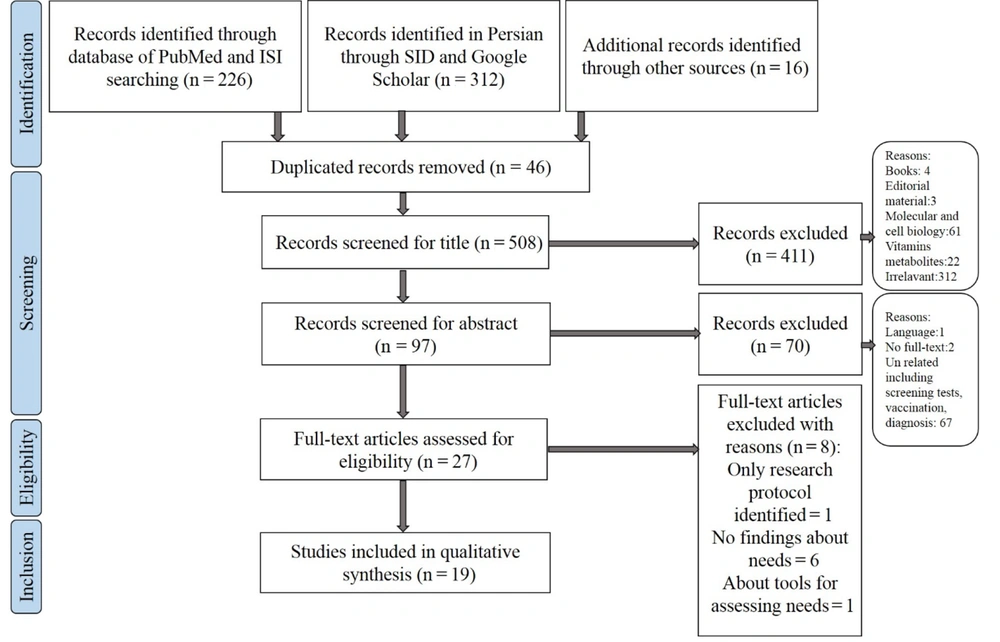
To find the relative articles, databases of PubMed, Web of Science (ISI), SID, and Google Scholar were searched in October and November 2022 with three keywords, including "inborn errors of metabolism, need, and care", that were combined with the Boolean term "AND" (Table 1). For identifying additional records, the related references and the cited articles of found studies were also assessed. All published manuscripts in English or Persian without limitation of the type of them and time were included. The articles in languages other than English or Persian, book chapters, editorial material, no full text available, or only abstracts presented in seminars and conferences were excluded. Then, the full texts of the articles were read carefully to perform an interpretive analysis based on the study's question and objective. None of the Persian documents from both Google Scholar and SID databases was related to the question of this review. The flow chart for selecting articles was designed based on the PRISMA statement (17) (Figure 1).
| Database | Date | Keywords | Article Retrieved |
|---|---|---|---|
| PubMed | 2022, Oct & Nov. | Inborn errors of metabolism AND need AND care | 50 |
| Web of Science (ISI) | 2022, Oct & Nov. | 176 | |
| Google Scholar (English) | 2022, Oct & Nov. | 52600 | |
| Google Scholar (Persian) | 2022, Oct & Nov. | 28 | |
| SID (Persian) | 2022, Oct & Nov. | 284 |
2.3. Data Evaluation and Quality Appraisal
Two independent reviewers screened all titles and abstracts for inclusion and assessed each selected reference independently. Additionally, these reviewers extracted and abstracted the data of each article independently, and disagreements were resolved by discussion and consensus with the third author. Then, all articles included in this study were evaluated using the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) checklist and Joanna Briggs Institute (JBI) checklists based on their methods. The PRISMA checklist was used for appraising reviews, and it has 7 sections and a total of 27 items for evaluating title, abstract, introduction, methods, results, discussion, and other information. If the item was reported in the study, it would get a score of 1, and if not, it would get a score of 0 (18). The JBI checklists were used for appraising quantitative and qualitative studies, which include independent checklists for case series, cross-sectional, and qualitative studies. They consisted of 10, 11, and 10 questions, respectively. The questions can be answered with yes, no, unclear, and not applicable. Those articles that had the most criteria (≥ 50%) were entered into the study (19, 20). After the quality appraisal, no study was excluded.
3. Results
In this section, the 4th and 5th stages of Whittemore and Knafl's (2005) method, including data analysis and findings, are presented.
Studies included in this integrative review were 19 articles that had different methodologies, consisting of 9 quantitative, 7 qualitative, and 3 review studies. Their published data were within 2003 to 2022, and most of them belonged to the UK [5], Canada [3], and the USA [3]. Other articles belonged to Germany [2], Turkey [2], Australia [1], Netherlands [1], Argentina [1], Japan [1], and Switzerland [1]. Table 2 shows the summary of the studies and their findings.
After data synthesis based on Whittmore and Knafl (2005), three main categories, including children, parents/family, and health system needs, were identified. Table 3 shows each category and its subcategories.
| No. | Title | Authors/Year | Study Design | Findings |
|---|---|---|---|---|
| 1 | Long-term needs of adult patients with organic acidemia: Outcome and prognostic factors | Martin-Hernandez et al./2009/UK (21) | Quantitative/reviewing medical records of 15 patients with organic acidemia | The multidisciplinary approach to care; need for support for the transition from adolescence to adulthood; most of them were dependent on their parents; appropriate counseling for women of childbearing age about pregnancy, childbirth, and its potential risks; nutritional needs such as tube feeding, nocturnal feeding for maintaining energy, supplements, diet restriction; different systems assessment based on the signs and symptoms of patients such as neurological problems, renal failure, cardiomyopathy, osteoporosis, optic problems. |
| 2 | Perspectives on dietary adherence among women with inborn errors of metabolism | Kemper et al./2010/USA (22) | Qualitative/focus groups | Dietary needs; need to educate about medical diet and sources of medical foods, preparation of medical foods; need insurance coverage for medical foods; need to assist with the transition from pediatric to adult healthcare providers; need to develop symptom-based dietary monitoring |
| 3 | Inborn errors of metabolism: Psychosocial challenges and proposed family systems model of intervention | Weber et al./2012/USA (23) | Review | Need support as they focus on immediate practical demands, grieve over illness; related losses and reorient future expectations |
| 4 | Living with an inborn error of metabolism detected by newborn screening: Parents’ perspectives on child development and impact on family life | Gramer et al./2014/Germany (24) | Quantitative/descriptive | Need for comprehensive multidisciplinary care, including psychological, financial, and social support |
| 5 | A national survey of providers treating patients with metabolic disorders identified by newborn screening demonstrates challenges faced by clinical care systems | McClain et al./2015/USA (25) | Survey on 114 healthcare providers working with IEM patients and families | Lack of insurance coverage; lack of reimbursement for the services; system-level interventions are needed to support the development of and access to interventions and for coordination of healthcare delivery; need for more communication between healthcare professionals; to restructure the fragmented healthcare delivery system to favor patient-centered, coordinated care while slowing an unsustainable trend in rising healthcare costs |
| 6 | Experiences of caregivers of children with inherited metabolic diseases: A qualitative study | Siddig et al./2016/Canada (26) | Qualitative | Specialized diet needs; children's social needs; social support for parents; fitting in with peers; need for coordinated care across the healthcare team |
| 7 | Child and family experiences with inborn errors of metabolism: A qualitative interview study with representatives of patient groups | Khangura/2016/Canada (27) | Qualitative | Need for specific improvements in health services, such as better care coordination; need for achieving a diagnosis; need to receive appropriate support |
| 8 | Parent coping and the behavioral and social outcomes of children diagnosed with inherited metabolic disorders | Brown et al./2017/Australia (28) | Quantitative/cohort (multiple questionnaires accomplished by 22 parents) | Need for a multidisciplinary team for supporting families and considering biopsychosocial factors; parents need psychological assessment and support after the diagnosis of IEM |
| 9 | Difficulties in daily life and associated factors and quality of life of children with inherited metabolic disease and their parents in Japan: A literature review | Yamaguchi et al./2017/Japan (29) | Review | Need to expand education for primary care physicians about IEM patients; psychological support for families; social support for parents; assessment of children and families' health status, burden, and stress at regular clinic visits; support groups for associate families who have similar experiences to peer support; need for attentive hearing, empathy, and recipiency in daily clinical practice by medical professionals; patient education about diet therapy; education about self-care with consideration for the child's growth and development, intelligibility, and sense of values, and with praise for the child's efforts |
| 10 | Parenting a Child with Phenylketonuria (PKU): An Interpretative Phenomenological Analysis (IPA) of the Experience of Parents | Carpenter et al./2018/UK (30) | Qualitative: Interpretive phenomenology | Need for acceptance of diagnosis and management; educational need; support from others |
| 11 | What are the information needs of parents caring for a child with Glutaric aciduria type 1? | Piercy et al./2019/UK (31) | Qualitative focus group | The need to be active partners in medical management to feel in control of the situation through understanding the condition and managing the condition by ensuring the restricted regimen |
| 12 | The need for additional care in patients with classical galactosemia | Welling et al./2019/Netherland (9) | Quantitative/cross-sectional | Dietary needs; need for additional care in the domains of mental function, speech, and voice; need to monitor the appearance of the potential impairments associated with the disease |
| 13 | The impact of disease severity on the psychological well-being of youth affected by an inborn error of metabolism and their families: A one-year longitudinal study | Dimitrova et al./2021/Switzerland (32) | Quantitative/Longitudinal | A child psychologist specializing in IEMs; receiving highly specialized interdisciplinary care at a tertiary center |
| 14 | New recommendations for the care of patients with mucopolysaccharidosis type I | Bay et al./2021/Argentina (33) | Review | Need for early diagnosis and treatment and an interdisciplinary follow-up |
| 15 | Inborn Errors of Metabolism in Pediatric Palliative Care | Harputluoglu et al./2021/Turkey (34) | Quantitative/cross-sectional | Need for social, physical, psychological, and physiotherapy |
| 16 | Exploring the experiences of family caregivers with low income accessing healthcare services for children with inborn errors of metabolism | Chimney/2022/Canada (1) | Qualitative/Grounded Theory/Thesis | Unmet needs: Psychological support; financial resources; providing education; local community events; flexibility in care |
| 17 | “Why them, why me, why us?” The experiences of parents of children with lysosomal acid lipase deficiency: An interpretative phenomenological analysis study | Hassall et al./2022/UK (35) | Qualitative/Phenomenology | Need for psychological support of family |
| 18 | Unmet Needs of Parents of Children with Urea Cycle Disorders | Scharping et al./2022/Germany (36) | Quantitative/prospective single-center pilot study | Need for information on the growth and development of children; information on current or future services available for children; additional supporting services; support in finding a suitable caretaker; talk to other affected families; support for insomnia, fatigue, loss of appetite, finding meaning in the situation, physical exhaustion; support for the feeling of being useless, powerless, and helpless; additional support groups; psychological support |
| 19 | Unmet Needs of Children with Inherited Metabolic Disorders in the COVID-19 Pandemic | Ozalp Akin et al./2022/Turkey (37) | Quantitative/cross-sectional | Need for special services and rehabilitation; need for financial support; Domains of services: Healthcare needs: Access to healthcare for follow-up; receiving medicine; support for specific diet; Educational needs: Preschool education; schooling; Special services and rehabilitation: Special education for cognitive difficulties; physiotherapy; speech and language therapy; vision/hearing rehabilitation; occupational therapy. |
Abbreviation: IEM, inborn errors of metabolism
a Articles are sorted ascending by the date of publication.
| Children with IEM | Parents or Caregivers | Healthcare System |
|---|---|---|
| Dietary and nutritional needs (5): Tube feeding, nocturnal feeding, supplements, diet restriction; education about medical diet and sources of medical foods, preparation of medical foods; development of a symptom-based dietary monitoring; specialized diet Social needs (3): Fitting with peers; education about preschool and schooling Psychological support (4): A child psychologist specialized in IEMs; improvement of the quality of life; regular health status, burden, and stress check at regular clinic visits Different systems’ assessments and additional needs (4): Mental function; cognitive difficulties; speech and voice; vision and hearing; monitoring potential impairments; musculoskeletal and physical function; growth and developmental monitoring; physiotherapy; occupational therapy; special services and rehabilitation Self-care education with consideration for the child's growth and development, intelligibility, and sense of values, and with praise for the child's efforts (1) | Psychological support (9): Support as they focus on immediate practical demands, grieve over illness-related losses and reorient future expectations; psychological assessment and support after the diagnosis of IEMs; attentive hearing, empathy, and recipiency in daily clinical practice by medical professionals; support for achieving acceptance; social worker in the team; support for the feeling of being useless, powerless, and helpless; support for insomnia, fatigue, loss of appetite, finding meaning in the situation, physical exhaustion; regular health status, burden, and stress at regular clinic visits Social support (5): Associate families who have similar experiences to peer support; local community events; finding a suitable caretaker; additional support groups; involving others to care for the child as he/she is growing Educational need (2): Management of disease; information on the growth and development of children; information on current or future services available for children; additional supporting services Financial support (2) Managing the condition (4): Achieving a diagnosis; flexibility in care; being an active partner in medical management to feel in control of the situation | Multidisciplinary approach for care, including psychological, financial, and social support in which clinician and dietician be the core (5): Patient-centered and coordinated care between patients, families, and healthcare providers (3); support for the transition from adolescence to adulthood (2); appropriate counseling for women of childbearing age about pregnancy, childbirth, and its potential risks Healthcare systems-level interventions (3): Access to healthcare for interventions and follow up; receiving medicine; support for specific diet; insurance coverage of medical foods, and medical services; expanding education about IEMs for primary care physicians (1) |
Abbreviation: IEM, inborn errors of metabolism
3.1. Children’s Need
Children's needs are categorized into dietary and nutritional, social, and psychological support, self-care education, different systems assessments, and additional needs. The most reported needs of children with IEMs are their dietary and nutritional needs, including a specialized diet, education about medical diet and sources of medical foods, preparation of them, diet restriction, supplements, need for tube feeding and nocturnal feeding, and developing symptom-based dietary monitoring (9, 21, 22, 26, 29).
Inborn errors of metabolism are a group of rare and chronic diseases that the patients must support psychologically (27, 29, 32, 34) and socially (26, 34, 37). There must be a child psychologist specialized in IEMs (32) to help them improve their quality of life, as well as their health status, stress, and burden check at regular visits (29). Additionally, these children need social support, especially for fitting in with peers (26, 34) and educating about preschool and schooling (37).
These diseases might affect multiple systems and cause impairments in them, such as the nervous system, mental status and cognition, vision, hearing, speech and voice, musculoskeletal and physical functions, growth, and development (9, 21). Therefore, they need different system assessments for monitoring potential impairments (9, 21) and additional services for caring and rehabilitation (37), including physiotherapy, occupational therapy, and speech therapy (34). Importantly, they need to be educated about self-care, especially about the growth and development of the child, intelligibility, and sense of values, and the child's efforts must be considered.
3.2. Parents'/Family's Needs
Parents/families of children with IEMs have numerous needs consisting of psychological support, social support, financial support, education, and managing the condition. The most important need of parents is psychological support and assessment. It should begin as soon as the diagnosis is made because parents must focus on care demands, grief induced by illness-related losses, and future expectations reorientation (23, 28, 35). They need help to achieve acceptance (30) and overcome feelings of uselessness, powerlessness, helplessness, insomnia, fatigue, loss of appetite, finding meaning in the situation, and physical exhaustion. Parents need attentive hearing, empathy, and recipiency in daily clinical practice by medical professionals (29); therefore, a social worker and a psychologist must be involved in the healthcare team to regularly check their health status (1, 21, 32), burden, and stress (29).
Social support is another important need of parents. They need to connect to families who have similar experiences for peer support (26, 29, 30, 36). Additionally, they need additional support groups (36), local community events (1), finding a suitable caretaker, and involving others to care for the child as he/she is growing (36).
Another category that emerged in data synthesis was parenteral needs for managing the condition. Firstly, they need a documented diagnosis that describes the condition (27, 33). Then, to have an active role in caring for the child, they need to understand the condition and manage it through coordinated and controlling intake and involvement (31). There should be flexibility in care to optimize the management (1).
The educational needs of parents are in the domains of disease management, growth and development of the children, and current or future services available for children (30, 36). Additionally, parents need financial support to cover the costs of treatment and care for a child with IEMs (1, 37).
3.3. Healthcare System’s Needs
In addition to children's and parent's needs, some needs should be met in the healthcare system. The essential one is using a multidisciplinary approach to care in which the clinician and dietician are the core and collaborate with nurses and other specialist services, such as social workers, physiotherapists, and psychologists (21, 24, 28, 32, 33). Moreover, it should be patient-centered and coordinated between patients, families, and healthcare providers (25-27). The healthcare system must support the transition from pediatric to adult healthcare providers (21, 22). It should pay special attention to the issue of counseling for women with IEMs in childbirth age about pregnancy, childbirth, and its potential risks (21).
Some interventions must have been implemented at the healthcare system level, such as providing access to healthcare for interventions and follow-up (25, 37), receiving medicine (37), support for specific diets (37), and insurance coverage of medical services and medical diets and foods (22, 25). Expanding education about IEMs for primary care physicians should also be noted because they are at the frontline and usually take the immediate responsibility of caring for patients with IEM (29).
4. Discussion
This review synthesized the data on the care needs of children with IEMs and their parents to provide a better understanding of their condition and make healthcare professionals able to implement a more specific and detailed care plan. The results of the present study showed that the care needs of these patients can be categorized into three categories: Children, parents, and healthcare systems' needs.
4.1. Children's Needs
The most important needs that must be included in any care plan for children with IEMs are specialized diet and nutritional supplements. Children with IEMs have to follow a restricted diet therapy lifetime to prevent metabolic crisis (29), which causes multiple difficulties for them. One critical aspect of dietary management in these children is the supplementation of vital nutrients with medical foods (22, 29). Medical foods supply essential nutrients except for the restricted ones in many forms, such as powder, formula, and drinks. Growth failure and metabolite decompensation might be caused by a lack of access to these special foods (1).
Additionally, caregivers, who are generally parents, have to ensure that the child has enough energy intake that needs frequent feeding. Even at night, the fasting length must not exceed 4 hours in some types of IEMs (1); therefore, they need nocturnal feeding in addition to daytime feeding. It might also be essential in children with feeding problems and anorexia (21). As the intake needs of each patient differ from the other, it seems necessary to develop new interventions to monitor their dietary intake based on their needs and symptoms of the disease. To achieve the best result, dietary interventions would need to be individually tailored (22, 26). As the children grow, they take more responsibility for self-care, and education plays a critical role in it. They must be educated about diet intake, restrictions, and medical foods (29). Early education might help improve long-term adherence, especially with their peers and teachers (22). In self-care education, the age of children, their growth and development, intelligibility, and sense of values should be considered, and the efforts of children have to be appraised (29).
Alongside nutrition, children with IEM have multiple system involvement, which necessitates different systems’ assessments and additional care needs. For example, Martin-Hernandez et al. (2009) suggested the regular assessment of musculoskeletal for monitoring osteoporosis, nephrotic for developing renal failure, cardiac for the possibility of cardiomyopathy, or neurological for progressing mental and cognitive functions (21). The importance of identifying such impairments is that we can find them early and prepare help, care, or treatment in time (9). Other mentioned impairments include speech and voice, vision and hearing loss, growth and development, motor function, and intellectual ability (9). Children with IEMs might need additional care, treatment, and rehabilitation for these problems, such as physiotherapy, occupational therapy, and speech therapy (34, 37).
Psychological and social support are the other two important needs of children with IEMs. A child psychologist specializing in IEMs can help these children more efficiently (34). Their health status, burden, and stress must be assessed regularly (29). Moreover, psychological and social support can be provided by rare disease patient groups, social networks, and supportive resources (27). Children with IEMs need support to fit in with their peers and should have received education about preschool and schooling (37).
4.2. Parents' Needs
Children's disease is a crisis for families, and it can affect not only the child but also the parents. The awareness of the fact that the child's life and prognosis are in the parents' hands puts a great burden on them (29). Therefore, they face many problems and have numerous needs. The first one is achieving a diagnosis because a diagnosis of IEMs always accompanies doubts, and it takes time to reach a final diagnosis. Moreover, at last, many unknowns remain about the prognosis and the future of the child (27). The healthcare professional must help parents gain acceptance (30) and psychologically support and assess them as they focus on immediate care demands, grief induced by illness-related losses, and future expectations reorientation (23, 28, 35). Additionally, parents need support for overcoming insomnia, fatigue, loss of appetite, finding meaning in the situation, physical exhaustion, and feeling useless, powerless, and helpless (36). All of them need attentive hearing, empathy, and recipiency by healthcare professionals (29). Therefore, the presence of a social worker and a psychologist in the healthcare team seems essential (1, 21, 32).
Parents need peer support from families with similar experiences (26, 27, 32), access to other support groups (36), and local community events (1) to benefit from the support of one another, such as finding a suitable caretaker or involving others to care for the child as he/she is growing (36). Social support can affect the satisfaction with the life of these parents (29), and it is important for parents' well-being (26).
When a rare and chronic disease, such as IEMs, is diagnosed, many questions arise in the minds of parents. They need information on the disease, its management, the child's growth and development, current or future services available for children, and additional supporting services (30, 36). The parents' need for information reveals the importance of regular appointments for the whole family to keep them informed of the latest developments, answer their questions, and respond to emerging needs (36). The scientific information must be in a written and practically focused form (31).
In addition to information, parents need to understand the condition to be an active partner in the management of the disease. This involved struggling with science and being aware of the worst scenario. They need to be aware of the worst conditions to manage the condition and prevent irreversible complications (31). Managing the condition comes through ensuring that the restricted regimen is adhered to, which is achieved by coordinating and controlling intake and involvement and developing a shared care plan (31). Additionally, flexibility in care is valuable for parents in managing the condition. For example, the possibility of collecting blood samples allows the family to save time or access different formulas covered by the government, which helps families make changes in their child's diet (1).
The last important and most reported need of parents in the studies is financial support in providing medical supplies, food, and medications and assisting to cover the costs of care (1, 37). However, Scharping et al. (2022) did not report it as an unmet need of parents of children with urea cycle disorders, which might be the result of German policies in supporting these families (36).
4.3. Healthcare System's Needs
Some of the changes must have been made at the healthcare system level to meet the needs of children with IEMs and their families. The most important one is applying a multidisciplinary approach, which is patient-centered and coordinated between patients, families, and healthcare professionals (25-27). Clinicians and dieticians have to be the core, and other healthcare professionals include nurses, social workers, psychologists, occupational therapists, physiotherapists, and speech therapists (21, 28, 32, 33). Care approaches should consider support for the transition from adolescence to adulthood (21, 22) and providing care, such as counseling for women in childbirth age about pregnancy, childbirth, and its potential risks both for the mother and the child (21).
The healthcare system level needs interventions that can provide patients and families with access to services and follow-ups, medicine or enzyme prescriptions, specific diet (25, 37), and insurance coverage of medical foods and medical services (22, 25). Improving health outcomes for these patients without access to healthcare services will not be effective (25). Although there are some policies for improved delivery of healthcare systems in developed countries, such as The Patient Protection and Affordable Care Act of 2010 (ACA), which holds promise in expanding access to healthcare coverage (25) in developing or underdeveloped countries, there is a long way to go (37). It is also necessary to expand primary care physicians' education about IEMs (29). Usually, primary care physicians are the ones who met children with IEMs for the first time, and having enough knowledge about these rare conditions would help them in managing, referring them to appropriate specialists, and subsequently preventing unwanted consequences, such as intellectual disabilities (29).
4.4. Conclusion
This integrative review aimed to categorize and summarize the needs of children with IEMs and their parents. This study highlighted the most important needs in three categories: Children's, parents', and the healthcare system's needs. Generally, children's needs include dietary and nutritional, social, and psychological needs, the need to assess different systems and their additional needs, and the need for self-care education. Parents needed psychological, social, educational, and financial support and help in managing the condition. The healthcare system needs to provide a multidisciplinary approach to caring for these patients and more effective healthcare interventions. To achieve optimum outcomes, a multidisciplinary, family-centered, and coordinated care plan must be applied, and more supportive plans must be used for these patients and families. In this care plan, the patient and the family are at the center of any assessment, planning, and intervention, and this care plan would be able to satisfy the needs of patients and parents. Additionally, a multidisciplinary approach would be able to cover needed healthcare interventions and provide well-designed and patient-centered care. It is suggested that further studies be designed to evaluate the needs of patients with IEMs of different ages and studies for developing a care plan for IEMs, applying it, and evaluating its effect on the patients' and their parents' quality of life.
4.5. Study Limitations
Most of the articles belonged to developed countries; therefore, it was impossible to assess the needs in developing and undeveloped countries, which have different welfare and healthcare policies, IEM prevalence, and family structures.