1. Context
Nowadays, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is one of the most globally significant infections (1, 2). The spread of communicable and infectious diseases such as Middle East respiratory syndrome (MERS), SARS, and coronavirus disease 2019 (COVID-19), which are airborne diseases, underscores the importance of air quality (3, 4). This infectious disease poses a significant threat to population growth worldwide. Since its first discovery in humans on December 8, 2019, the SARS-CoV-2 virus and the resulting disease, known as COVID-19, have rapidly spread across the globe (5). Considering that countries on all five continents reported cases of SARS-CoV-2, the World Health Organization (WHO) declared COVID-19 a global pandemic based on these reports (6). At the onset of this pandemic, due to the virus's impact on the upper respiratory system, including the nose and throat, most patients seeking medical attention exhibited clinical symptoms related to the respiratory system, as well as ear, nose, and throat issues (7, 8). The sudden and widespread outbreak of suspected cases of a new flu-like disease in Chinese citizens, and subsequently around the world, remains poorly understood (9, 10).
Different results from various studies on COVID-19 have shown that the virus primarily affects the alveoli, which are responsible for the exchange of respiratory gases with blood gases. This can ultimately lead to shortness of breath, lung dysfunction, respiratory system defects, and vital organ failure, which can result in death (11-17). Medical research has also established a relationship between COVID-19 exacerbation and conditions such as cardiac arrhythmia, diabetes, hypertension, ischemic heart disease, and asthma (18).
Population growth, air pollution, and noise pollution are the primary agents that pose threats and can be harmful to organisms, especially humans (19-23). According to multiple studies, the major organs most affected by air pollutants are the lungs (leading to respiratory diseases) and the heart (resulting in cardiovascular diseases) (24-28). Toxic air pollutants can significantly impact organs such as the eyes, lungs, heart, and brain, disrupting their normal function (29-36). Conditions like asthma, chronic obstructive pulmonary disease (COPD), and COVID-19 are among the most important noncommunicable diseases whose prevalence increases in metropolitan areas due to air pollution (37-41).
Environmental factors and physiological characteristics of the body have various negative effects, including an increase in the prevalence, hospitalization rates, and mortality due to COVID-19 (42). Air pollution, which significantly reduces the oxygen content in human respiratory air and includes various pollutants—solid, liquid, gas, or radioactive/nonradioactive radiation—affects the quality of life for humans and other living organisms (43, 44). Long-term exposure to air pollutants increases the risk of heart attacks, strokes, asthma, impaired brain development in children, Alzheimer's disease, Parkinson's disease, schizophrenia, chronic lung diseases, and various cancers (blood, lung, liver, and brain), ultimately leading to death (45-49). Decreasing air pollution emissions, reducing human activities, significantly decreasing transportation, staying at home, practicing hand hygiene, and maintaining physical distancing are among the most critical interventions to slow the spread of the disease (18, 50).
The purpose of this narrative review report is to understand the impact of COVID-19 and air pollution on the risk factors associated with COPD, cardiovascular diseases (CDs), and respiratory diseases (RDs).
2. Methods
2.1. Eligibility Criteria and Search Strategy
A review of the epidemiological literature was conducted using references available in various databases, including ScienceDirect, Springer, Google Scholar, Web of Science, and PubMed (Table 1). The search criteria included publications in English from 1993 to 2022 and studies involving human participants.
| Terms | Google Scholar | Web of Science | ScienceDirect | PubMed | Springer | Unique Results |
|---|---|---|---|---|---|---|
| SARS-CoV-2 | 141 | 51 | 24 | 28 | 8 | 252 |
| COVID-19 | 87 | 28 | 32 | 23 | 10 | 180 |
| Air pollution | 66 | 34 | 16 | 16 | 6 | 138 |
| Air pollution and COVID-19 | 52 | 21 | 19 | 21 | 8 | 121 |
| COVID-19 and COPD and respiratory diseases | 34 | 23 | 12 | 13 | 3 | 85 |
| COVID-19 and cardiovascular diseases | 25 | 19 | 8 | 10 | 4 | 66 |
| Air pollution and cardiovascular diseases | 21 | 76 | 6 | 5 | 2 | 110 |
| Air pollution and COPD and respiratory diseases | 13 | 13 | 14 | 9 | 4 | 53 |
| Total | 439 | 265 | 131 | 125 | 45 | 1005 |
2.2. Eligibility Criteria
Data gathering was performed using medical subject headings (MeSH) terms, including ‘SARS-CoV-2,’ ‘COVID-19,’ ‘Air Pollution,’ ‘COVID-19 and COPD and respiratory diseases,’ ‘COVID-19 and cardiovascular diseases,’ ‘Air Pollution and cardiovascular diseases,’ and ‘Air Pollution and COPD and respiratory diseases.’ To ensure the inclusion of all relevant research, the following terms were combined with air pollution and SARS-CoV-2 to assess their impact on the risk factors associated with cardiovascular and RDs.
2.3. Study Selection
The literature search was conducted in 2 stages, with the time frame limited to studies published between 1993 and 2022. The search encompassed research examining the effects of COVID-19 and air pollution on risk factors associated with COPD, CDs, and RDs. This included articles from English-language journals and searches in various databases, resulting in 125 articles from PubMed, 131 articles from ScienceDirect (Scopus), 45 articles from Springer, 264 articles from Web of Science, and 439 articles from Google Scholar.
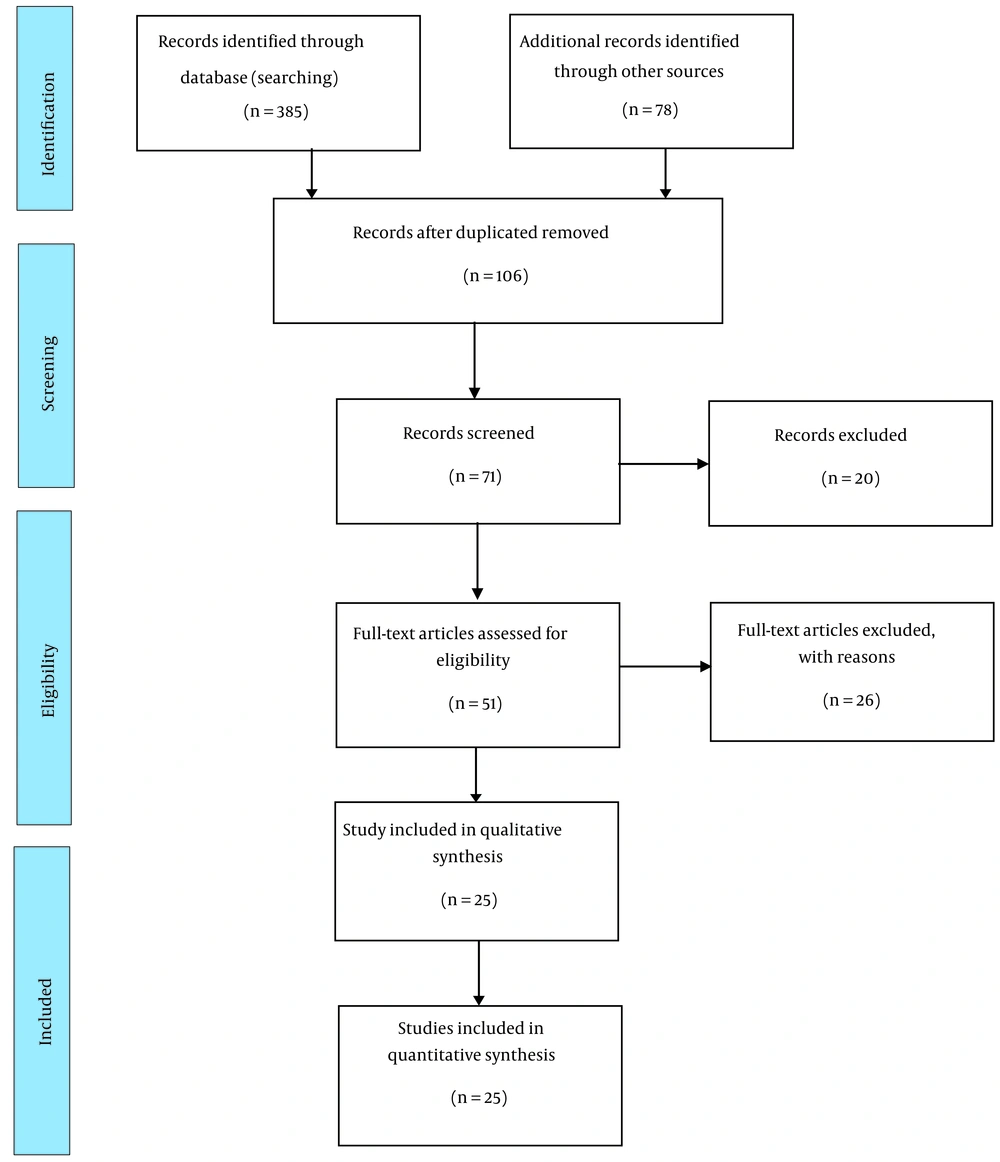
Following the specified criteria, a preliminary screening of 1 005 publications yielded 385 articles that were selected based on database search results. Additionally, a citation review for the terms mentioned above added another 78 articles. In the subsequent stage, 71 studies were reviewed to establish the possible connection between COVID-19 and air pollution regarding the risk factors associated with CDs and RDs. After the review, 51 full-text articles were included in the analysis. Ultimately, 25 articles were selected for inclusion. The process of study preparation and article selection based on the preferred reporting items for systematic reviews and meta-analyses (PRISMA) flow diagram is presented in Figure 1.
The studies that were included in this review met the criteria mentioned below:
- It was written in English and published from 1993 to 2022.
- It was conducted to study the impact of COVID-19 and air pollution on the risk factors attributed to COPD, CDs, and RDs.
The following studies were excluded:
- Studies that were unrelated to COVID-19 and air pollution
- Studies that did not consider the risk factors attributed to COPD, CDs, and RDs
- Those that did not include original data
- Review articles (the reference list was still searched to find other potentially relevant studies)
- Not available in English
- Without a full text available
2.4. Extracting the Data
The information collected from all the studies included study objectives, study setting, statistical analysis, main findings, and limitations. In studies that contained health data, we also extracted study design, study population, health criteria, and outcome evaluation.
3. Results and Discussion
3.1. Sources and Ways of Transition for COVID-19
SARS-CoV-2 was relatively unknown and inconspicuous until it underwent a mutation in 2003, leading to the emergence of a new virus called SARS. This introduced a novel form of the disease to the world, resulting in approximately 8 000 infections and 800 deaths (51). In 2012, another mutation in the virus led to the emergence of MERS, which caused 105 fatalities and infected 573 individuals (52). What distinguishes COVID-19 from SARS and MERS, despite their higher lethality rates, is its rapid spread and high prevalence.
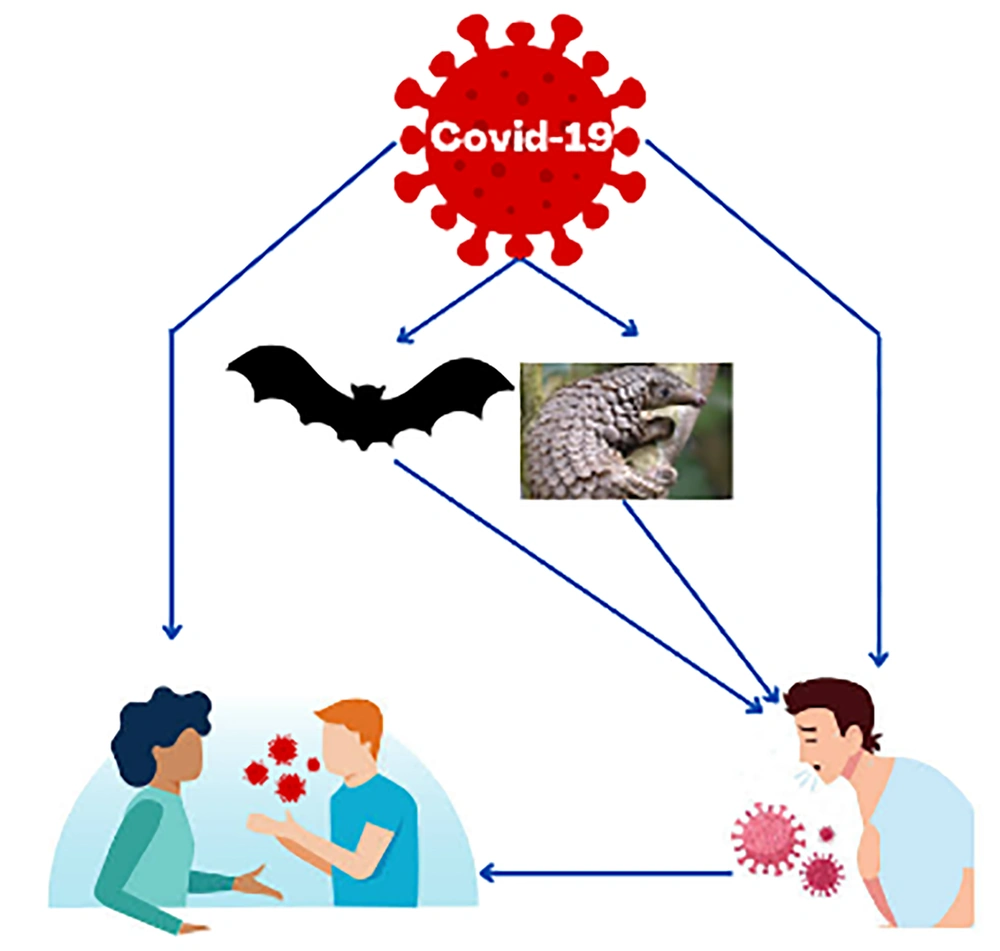
Experiments have indicated that the disease was initially observed in bats, making them the primary reservoirs, although the intermediate source remains unknown (Figure 1). Both SARS and MERS viruses have been transmitted from bats to humans. Laboratory studies have revealed that the SARS-CoV-2 virus shares approximately 90% similarity with the coronavirus found in horseshoe bats and about 70% similarity with the SARS-CoV in terms of RNA genome sequencing.
Common symptoms of COVID-19 include cough, fever exceeding 38°C, chills, headache, runny nose, and body aches. Less common symptoms encompass vomiting, diarrhea, gastrointestinal problems, loss of smell and taste, skin rash, hair loss, and red eyes (53). Figure 2 illustrates the sources and transmission methods of COVID-19.
3.2. Clinical Characteristics of COVID-19 Patients
Headache, sore throat, confusion, dry cough, fever, chills, muscle pain, loss of taste and smell, dyspnea, chest pain, rhinorrhea, rigors, acute respiratory distress syndrome (ARDS), respiratory tract infections, pneumonia, and death are among the most common clinical characteristics of COVID-19 in patients (54-57).
Mortality resulting from COVID-19 involves complex scenarios. In addition to pulmonary complications, deaths caused by this virus may also result from its detrimental effects on the heart and brain, even in individuals who were previously healthy (58). It is evident that COVID-19 tends to cause more severe symptoms in individuals with pre-existing cardiovascular conditions. Consequently, cardiovascular associations have advised such individuals to rigorously follow health protocols (59). What remains mysterious is the development of heart-related complications in individuals who had never experienced heart conditions prior to contracting COVID-19 (57, 60). One of the most perilous complications of this disease is an increased tendency for blood coagulation, elevating the risk of stroke (61). COVID-19 exhibits more adverse effects on the cardiovascular and nervous systems of individuals with neurological conditions such as multiple sclerosis (MS), Alzheimer's disease, stroke, and Parkinson's disease (62, 63).
3.3. Major Airborne Pollutants Harmful for the Human Body
Air pollution is defined as substances in the atmosphere that are harmful to the health of humans and other living beings and materials. The main types of air pollutants include particulates (both organic and inorganic), gases (such as carbon monoxide, nitrous oxides, and sulfur dioxide), and biological molecules (64). According to a report by the WHO, air pollution is responsible for approximately 7 million deaths worldwide each year. It poses risks to various living organisms, including humans, animals, and food crops (65, 66).
Figure 3 illustrates the various health effects of exposure to air pollution, including RDs, CDs, neurological disorders, chronic illnesses, skin conditions, and eye irritation (27, 67, 68). The primary sources of toxic air pollutant emissions, which can have detrimental effects on public health, are both artificial and natural activities. These emissions raise significant concerns among citizens in megacities (69, 70).
Health reports highlight air pollution as one of the primary carcinogenic agents threatening public health. Inhaled volatile organic compounds, heavy metals, sulfur dioxide, carbon monoxide, ozone, nitrogen oxides, and particulate matter can have both acute and chronic effects on various organs in the body (67, 71).
3.4. The Role of Air Pollution in the Transmission of SARS-CoV-2
The impact of air pollution on the COVID-19 pandemic has not been sufficiently investigated. The primary entry points for the virus into the body are the mouth, nose, eyes, and ears. Aerosols and droplets containing SARS-CoV-2 have the potential to enter the human body (72). The relationship between air pollution and the transmission of SARS-CoV-2 is depicted in Figure 4. Both the environment and humans suffer from numerous environmental and health problems due to exposure to both short-term and long-term air pollution. The severity of health consequences depends largely on the concentration of pollutants in the ambient air and the duration of exposure to polluted air (72).
Prolonged exposure to air pollution and daily inhalation can reduce lung function, making individuals more susceptible to viral infections. This is due to the negative impact on the cilia in the airways, a reduction in lung respiratory capacity, and the exacerbation of disease symptoms (73). Air pollutants, including PAH, Pb, heavy metals, volatile organic compounds (VOCs), PM2.5, NO2, SO2, and O3, often exceed acceptable limits in many cities, particularly in industrial areas (74). Breathing clean air is as vital as maintaining a proper diet for a healthy life.
Various studies have shown an increased risk of respiratory disorders and abnormalities associated with exposure to toxic air pollutants. Moreover, RDs, especially COVID-19, can be severely affected by the harmful effects of air pollutants (23, 75).
According to studies conducted by the WHO, the European Union, the United States, and China, the original source of SARS-CoV-2 has not yet been determined. Results from these studies suggest that SARS-CoV-2 may have been transmitted to humans through various animals, including bats, birds, pigs, foxes, cows, dogs, and wild animals. Figure 4 presents a transmission hypothesis for the SARS-CoV-2 outbreak.
Scientists believe that animals, birds, and reptiles such as frogs, camels, rabbits, snakes, deer, peacocks, roosters, crocodiles, kangaroos, snails, cats, and goats could have been present at the virus's site of origin, Wuhan (China), and may have acted as intermediate hosts for the virus (76).
3.5. Air Pollution and Cardiovascular and Respiratory Diseases
There is a significant relationship between air pollutants and various diseases, including cancer, asthma, allergies, RDs, and CDs. This relationship has been well-documented in scientific literature (77-83). The effects of air pollution exposure on the heart and lungs are illustrated in Figure 5.
Several measures can be taken to enhance indoor air quality and mitigate the complications caused by pollutants. These include improving efficiency by repairing air conditioners and central ventilation systems, adopting clean fuels, replacing gas-burning vehicles, reducing heavy vehicle traffic on urban roads, transitioning industrial fuels to natural gas, mandating technical vehicle inspections, and replacing stoves to reduce cooking-related pollutants (84-86).
Numerous studies have shown that the most effective ways to reduce health risks associated with air pollutant exposure involve changing fuel sources, such as replacing solid fuels such as wood and dung with cleaner alternatives such as city gas with alkaline energy, increasing indoor fresh air circulation, and optimizing ventilation systems (86-88).
The CDs and RDs resulting from air pollutants and COVID-19 uptake with their damage mechanisms are presented in Table 2.
| Pollutant | Major Sources | Adverse Health Effects | References |
|---|---|---|---|
| COVID-19 | Respiratory droplets, human-to-human, direct contact, aerosol, snakes, pangolins, avians, civet cats, swine, phocine, bovine, canine, centipedes, goats, frogs, camels, wild rabbits, reptiles, cicadas, crocodiles, and kangaroos | Headache, sore throat, confusion, dry cough, fever, chills, anxiety, stress, anxiety, fear, muscle pain, loss of taste and smell, dyspnea, chest pain, rhinorrhea, rigors, acute respiratory tract infection, pneumonia, and molecular mechanisms of virus function in pathogenesis | (4, 18, 56, 57, 76, 89-96) |
| Particle matter | Dust storms, road dust, grassland fires, industrial processes, fuel/tobacco combustion, power plants, diesel engines, cleaning, operations, cooking, and biomass burning | Cardiovascular and respiratory diseases, coughing, inflammation, decreased lung function, difficulty breathing, aggravated asthma, heart attacks, irritation of the airways, tissue damage, hypertension, diabetes mellitus, and cancer | (67, 68, 97-103) |
| Nitrogen dioxide | Fuel combustion, wood burning, motor vehicles, stoves, waste burning, cigarette smoke, and power generation | Irritate airways, respiratory infections, asthma, inflammation, difficulty breathing, coughing, wheezing, tissue damage, throat irritations, headache, dyspnea, chest pain, diaphoresis, fever, bronchospasm, skin dryness, and atopic eczema | (21-23, 67, 104-109) |
| Sulfur dioxide | Natural volcanic activities, coal combustion, vehicle emissions, fuel incineration, crude oil and coal, industrial boilers, and metal processing | Respiratory irritation, cardiovascular diseases, asthma, irritation, wheezing, inflammation, bronchitis, changes in pigmentation, and respiratory dysfunction | (39, 67, 110-114) |
| Ozone (O3) | Interaction of VOCs and NOx with UV-photoactivation and combustion of fossil fuels | Breathing problems, asthma, emphysema, chronic obstructive pulmonary disease, coughing, irritation, inflammation, asthma, bronchitis, heart attack, tissue damage, skin dryness, acne, and atopic dermatitis | (22, 109, 115-120) |
Abbreviations: UV, ultraviolet; VOC, volatile organic compound.
4. Conclusions
The findings of this study demonstrate that air pollutants and COVID-19 infection have a synergistic effect on CDs and RDs. The study aimed to estimate the consequences of toxic air pollutants on COVID-19-related mortality.
The COVID-19 pandemic has caused a significant loss of life, infecting millions of people and delivering a severe blow to the global economy. The crisis stemming from the coronavirus epidemic and the resulting worldwide lockdowns have profoundly impacted various countries' economies. Air pollution also places individuals at risk for COVID-19 by triggering allergies. The cilia in the airways, which play a vital role in the respiratory system by clearing viruses, can be severely damaged when exposed to polluted air. Some economic effects of this deadly virus include increased unemployment rates, the closure of industries and large manufacturing companies, a decline in oil prices, and more.
According to daily reports from international organizations and the ministries of health of different countries involved in addressing COVID-19, one of the most significant factors influencing the disease's prevalence and severity is age. Older individuals are at higher risk of death and illness due to COVID-19. Some of the most crucial preventive measures to reduce the speed of disease transmission and break the chain of virus transmission include practicing social distancing, avoiding gatherings in densely populated areas, frequent handwashing, maintaining personal hygiene, refraining from touching one's eyes, mouth, and nose with contaminated hands, using standard medical masks, employing protective shields and gloves, minimizing unnecessary travel, and receiving vaccinations approved by the WHO.