1. Background
Multiple Sclerosis (MS) is an inflammatory disease of the central nervous system that affects and damages the myelin sheath in the brain and spinal cord. First recorded in 1822, this disease is the most prevalent neurological disorder in young adulthood (1). Although it can develop at any age, MS typically affects individuals aged 15 to 50, with a threefold higher incidence in women than in men (2). It appears that the incidence of MS has been steadily increasing over the past century, particularly among women (3). According to the latest statistics from the International Multiple Sclerosis Federation, over 2.5 million people worldwide suffer from this disease (4). Additionally, recent statistics from the Iranian Multiple Sclerosis Society have recorded approximately 70 000 cases of MS patients. However, the actual incidence of the disease is likely higher, as not all patients are registered with this society (5). The prevalence of MS has been reported to range from 2.20 to 16.28 per 100 000 people (4).
Multiple Sclerosis primarily occurs during the reproductive stages of human life and poses a threat to individuals’ independence and their ability to participate in family and society, leading to feelings of incompetence and lack of confidence (6, 7). As a chronic condition, MS requires a therapeutic, personalized, and organized program to alleviate its symptoms, delay disease progression, and empower individuals to engage in self-care and address associated challenges (8)).
Self-care is a multidimensional concept that encompasses various behaviors influenced by factors such as health beliefs, economic conditions, and life events (9). Today, self-care plays a significant role in primary care, with approximately 65% to 85% of patients' self-care activities being managed by themselves or their family members. Self-care agency is essential, representing an individual's ability to perform self-care actions (10). Self-care ability, on the other hand, involves a combination of knowledge, self-care tendencies and skills, and awareness of relevant activities (11-13). This ability is influenced by factors including age, gender, developmental stage, health status, life experiences, sociocultural context, healthcare system-related factors such as medical diagnoses and treatment modalities, lifestyle, family dynamics, environment, and available resources.
Orem posits that in addition to the factors mentioned, new parameters are being identified in various societies and conditions that can influence self-care agency (10). Given the restrictive living conditions of MS patients and the disabling nature of the disease, health-related behaviors that promote well-being and mitigate disabilities encounter challenges (14). One well-known model of health-promoting behaviors, introduced by Walker et al. in 1987, suggests that a health-promoting lifestyle is a multidimensional concept that begins with perceptions and actions, fosters personal motivation to enhance health, and ultimately leads to well-being, personal growth, and a fulfilling life. This model encompasses six dimensions: Interpersonal relationships, responsibility for health, self-actualization, stress management, nutrition, and physical activity (15). Theorists argue that engaging in health-promoting behaviors positively influences quality of life, resulting in improved health and reduced disease burden and disability (12).
As individuals with MS typically manage their care at home without direct supervision from healthcare professionals, they are primarily responsible for their own well-being. Self-care for these patients involves the methods they employ in managing their condition and monitoring symptoms (16). Studies investigating health-promoting behaviors in MS patients have revealed challenges such as damaged interpersonal relationships, loss of support networks, increased risk of depression, disease relapse (17), adoption of unhealthy dietary habits (18), and reduced physical activity due to disease-related limitations and fatigue (19). For instance, Chenary et al. reported undesirable health-promoting behaviors in their study (20). Recently, there has been a growing emphasis on the importance of taking responsibility for health in MS patients' self-management (21), as health-responsible behaviors significantly impact individuals’ well-being by encouraging healthy lifestyles and reducing the need for hospitalization (22). In this regard, patient education programs are designed practices aimed at helping patients modify their behavior to enhance their health (23).
Importantly, training chronic patients, such as those suffering from MS, is particularly significant since these patients need to be familiar with sources of information to manage their care at home (24). This is because one of the main components of programs aimed at controlling chronic diseases, which focus on adaptive management, is paying attention to patients’ abilities to correctly perform self-care behaviors (25). In this regard, nurses, serving as mediators between the patient, family, and treatment team, play a crucial role in teaching self-care and improving patients’ life expectancy (26). Familiarity with and awareness of self-care abilities are determining factors in disease control (27). Additionally, by examining health-promoting behaviors, we can identify the lifestyle of these patients and design appropriate empowerment interventions.
2. Objectives
Therefore, the present study aims to investigate the relationship between self-care ability and health-promoting behaviors in patients with Multiple Sclerosis.
3. Methods
3.1. Study Design and Setting
This research adopts a cross-sectional descriptive-analytical design. The statistical population comprises all MS patients under the coverage of the Multiple Sclerosis Society of Khuzestan Province. Sampling was conducted from November 2020 to January 2021.
3.2. Participants
The sample size for this study was calculated based on a study by Morowati et al. (27), where the self-care ability was reported as 51.47%. Thus, the sample size was determined to be 101 using the following formula with a confidence level of 95% and a margin of error of 0.05. The sample size was calculated using statistical software. Finally, considering a 10% attrition rate, the sample size was adjusted to 112 individuals.
The inclusion criteria comprised MS patients whose diagnosis was confirmed by a neurologist within the past year according to McDonald’s criteria, willingness to participate in the study, age over 18, ability to establish relationships, literacy, absence of mental disorders and history of drug consumption, and capability to complete online questionnaires. The exclusion criterion was incomplete questionnaire submission.
3.3. Measurements
The data collection tools included:
3.3.1. Demographic Information Questionnaire
This questionnaire collected general information such as the patient's age, marital status, occupation, level of education, history of chronic diseases, specific chronic diseases if present, duration of MS disease, history of participation in psychological training classes, and income level.
3.3.2. Self-care Inventory (SCI)
Developed by Weaver (1985), adapted by Geden and Taylor (1991), and revised by Lukkarinen and Hentinen (1997) and Tokam (2007), this 40-item scale assesses patients' cognitive function and attitude toward self-care agency in physical diseases. The inventory uses a 6-point Likert scale: (1) strongly agree (2) slightly agree, (3) agree, (4) disagree, (5) slightly disagree, and (6) strongly disagree. Scores range from 40 to 240, with higher scores indicating better self-care ability. The total score is obtained by summing scores of all questions. Self-care ability is interpreted as good (40 - 58), moderate (59 - 89), poor (90 - 160), and highly poor (> 160). Ebrahimi et al. validated the Persian version of SCI with a Content Validity Ratio (CVR) and Content Validity Index (CVI) of 98% and 95%, respectively (28). Additionally, Saadat et al. determined the reliability of the inventory using the test-retest method, reporting Pearson correlation and Cronbach alpha coefficients of 0.95 and 0.97, respectively (29).
3.3.3. Health-Promoting Lifestyle Profile (HPLP)
Walker et al. (1987) developed the Health-Promoting Lifestyle Profile based on its second version. This 52-item scale assesses health-promoting behaviors across six dimensions: Nutrition, physical activity, responsibility for health, stress management, interpersonal relationships, and self-actualization. Responses are scored on a Likert scale ranging from never (1) to most of the time (4). Each dimension is measured by specific sets of questions: Self-actualization (questions 1-9), responsibility for health (questions 10 - 18), interpersonal relationships (questions 19 - 27), stress management (questions 28 - 35), physical activity (questions 36 - 43), and nutrition (questions 44 - 52). Scores for each dimension are obtained by summing the scores of the corresponding items, with the total HPLP score ranging from 52 to 208. Higher scores indicate better health-related behaviors within each dimension. Scores between 202 and 208 are considered good, while scores from 150 to 201 are deemed acceptable, and scores below 150 are classified as poor health-promoting lifestyle profiles (28).
The Persian version of HPLP was validated in Iran by Mohammadi Zeidi et al., who conducted construct validity and confirmatory factor analysis, demonstrating an acceptable fit for the six-factor model (30). Walker assessed the reliability of the entire scale and its six dimensions using Cronbach’s alpha, reporting values of 94% for the overall scale and 79% - 94% for the individual dimensions (29). In the present study, the questionnaire exhibited high reliability, with a Cronbach's alpha coefficient of 0.93 for the overall scale. The reliability of the six dimensions of HPLP was also assessed, yielding Cronbach's alpha values of 0.73 for nutrition, 0.80 for physical activity, 0.71 for interpersonal relationships, 0.76 for responsibility, 0.74 for stress management, and 0.72 for self-actualization.
The researcher met with the chancellor of the Khuzestan Province Multiple Sclerosis Society to explain the research objectives and obtain permission to collaborate. Due to the ongoing Covid-19 pandemic and the associated risks for MS patients, as well as their limited ability to visit the society except for emergencies, the instruments were developed as online forms (via WhatsApp) after coordinating with the center's authorities. Subsequently, an expert from the society created a virtual group and added all patients covered by the society who met the inclusion criteria. The patients were provided with links to access the online questionnaires, which were shared in the virtual group. Alongside explaining the study and addressing any potential questions, the researchers emphasized that only patients between the ages of 18 and 60 should complete the questionnaires. Before proceeding, respondents were asked to review and confirm their agreement to the consent form. It's important to note that the questionnaires were completely confidential and anonymous to ensure ethical standards. Patients were encouraged to reach out to the researcher with any questions regarding questionnaire completion. Given that the completed questionnaires met the required sample size, there were no dropouts in the sample.
3.4. Statistical Analysis
All collected data were analyzed using SPSS version 26 software, with significance levels set at P ≤ 0.01 and P ≤ 0.05. Descriptive statistics, including mean and standard deviation for quantitative data and frequency percentages for qualitative data, were employed. The normality of variables was assessed using the Kolmogorov-Smirnov test, which confirmed their normal distribution. Statistical analyses included Pearson correlation, independent t-tests, and Analysis of Variance (ANOVA) tests.
3.5. Ethical Considerations
The Ethics Committee of Ahvaz Jondishapur University of Medical Sciences approved the present study (IR.AJUM.REC.1400.374). All necessary permissions for conducting the research were obtained from the relevant administrators, and all methods were performed in accordance with the relevant guidelines and regulations. Patients were informed about the voluntary nature of participation in the study and the option to withdraw their cooperation at any time. They were assured of the confidentiality of their information.
4. Results
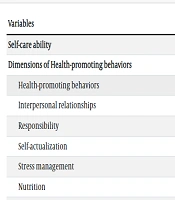
This study examined 112 MS patients, 83 of whom were women, aged between 41 and 50, married, employed, with diploma degrees, monthly incomes ranging from 4 to 8 million, disease histories of less than 10 years, and suffering from other chronic diseases (Table 1). The mean SCI score of the patients was 104.49 ± 12.72 (ranging from 40 to 240), indicating generally poor self-care ability according to the standard classification based on the questionnaire. Furthermore, the mean and standard deviation of health-promoting behaviors were generally 132.52 ± 12.72 (ranging from 50 to 208), suggesting a weak health-promoting lifestyle profile among the patients. Among the HPLP dimensions, the highest mean scores were observed in the responsibility for health dimension (33.65, ranging from 9 to 36), while the lowest mean scores were in the nutrition dimension (15.62, ranging from 8 to 34) (Table 2).
| Demographic Variables | Values a |
|---|---|
| Gender | |
| Male | 29 (25.89) |
| Female | 83 (74.11) |
| Job | |
| Unemployed | 23 (20.53) |
| Housewife | 33 (29.46) |
| Manual worker | 6 (5.35) |
| Employee | 34 (30.35) |
| Retired | 3 (2.67) |
| Non-governmental | 13 (11.60) |
| Marital status | |
| Married | 73 (65.17) |
| Single | 33 (29.36) |
| Divorced | 2 (1.78) |
| Widow | 4 (3.60) |
| Level of Education | |
| Diploma and below | 45 (40.17) |
| Associate degree | 18 (16.07) |
| Masters’ degree | 36 (32.14) |
| Masters’ degree and above | 13 (11.60) |
| Work department level and less | 43 (38.39) |
| Income level, million tomans | |
| Between 4 and 8 | 60 (53.58) |
| More than 8 | 9 (8.03) |
| History of chronic disease | |
| No | 30 (26.78) |
| Yes | 82 (73.22) |
| Kind of chronic diseases | |
| Multiple sclerosis disease (alone) | 30 (26.78) |
| Endocrine diseases | 14 (12.5) |
| Respiratory diseases | 7 (6.25) |
| Cardiovascular diseases | 38 (33.92) |
| Skeletal diseases | 6 (5.35) |
| Gastrointestinal diseases | 5 (4.46) |
| Neurological diseases | 10 (8.92) |
| Skin diseases | 2 (1.8) |
| Duration of MS disease, year | |
| Less than 10 | 68 (60.71) |
| More than 10 | 44 (39.29) |
| History of participation in psychological training classes | |
| No | 100 (89.28) |
| Yes | 12 (10.72) |
| Age, y | |
| 18 - 30 | 25 (22.32) |
| 31 - 40 | 30 (26.78) |
| 41 - 50 | 42 (37.50) |
| 51 - 60 | 15 (13.39) |
a Values are expressed as No. (%) except for age (No. (mean)).
| Variables | Values a |
|---|---|
| Self-care ability | 104.49 ± 12.72 |
| Dimensions of Health-promoting behaviors | |
| Health-promoting behaviors | 132.52 ± 13.60 |
| Interpersonal relationships | 20.50 ± 5.05 |
| Responsibility | 33.65 ± 4.60 |
| Self-actualization | 25.42 ± 4.46 |
| Stress management | 17.54 ± 2.88 |
| Nutrition | 15.62 ± 2.98 |
| Physical activity | 19.79 ± 3.41 |
| Level of self-care ability | |
| Good (40 - 58) | 0 (0) |
| Average (59 - 89) | 78 (69.6) |
| Poor (90 - 160) | 31 (27.7) |
| Very poor (≥ 160) | 3 (2.7) |
| Level of health-promoting behaviors | |
| Good (202 - 208) | 5 (4.5) |
| Acceptable (150 - 201) | 106 (94.6) |
| Poor (< 150) | 1 (0.9) |
a Values are expressed as mean ± SD or No. (%).
Regarding the relationship between self-care ability and health-promoting behaviors, the Pearson correlation test revealed a significant association of health-promoting behaviors with their dimensions and self-care ability (P < 0.001). All variables were positively correlated, indicating that an increase in one variable led to an increase in the other. Moreover, there was a moderate-to-strong relationship between self-care agency and health-promoting behaviors [r = 0.4 - 0.7 (moderate relationship); r > 0.7 (strong relationship)] (Table 3).
| Variables | Nutrition | Physical Activity | Responsibility | Stress Management | Interpersonal Relationships | Self-actualization | Health-Promoting Behaviors | Self-care Ability | |
|---|---|---|---|---|---|---|---|---|---|
| Nutrition | r | 1 | 0.67 | 0.697 | 0.687 | 0.674 | 0.765 | 0.508 | 0.508 |
| P-value | < 0.001 | < 0.001 | < 0.001 | < 0.001 | < 0.001 | < 0.001 | < 0.001 | ||
| Physical activity | r | 1 | 0.885 | 0.849 | 0.815 | 0.945 | 0.457 | 0.457 | |
| P-value | < 0.001 | < 0.001 | < 0.001 | < 0.001 | < 0.001 | < 0.001 | |||
| Responsibility | r | 1 | 0.925 | 0.910 | 0.978 | 0.516 | 0.516 | ||
| P-value | < 0.001 | < 0.001 | < 0.001 | < 0.001 | < 0.001 | ||||
| Stress management | r | 1 | 0.899 | 0.988 | 0.516 | 0.516 | |||
| P-value | < 0.001 | < 0.001 | < 0.001 | < 0.001 | |||||
| Interpersonal relationships | r | 1 | 0.992 | 0.482 | 0.482 | ||||
| P-value | < 0.001 | < 0.001 | < 0.001 | ||||||
| Self-actualization | r | 1 | 0.537 | 0.537 | |||||
| P-value | < 0.001 | < 0.001 | |||||||
| Health-promoting behaviors | r | 1 | 0.965 | ||||||
| P-value | < 0.001 | ||||||||
| Self-care ability | r | 1 |
Regarding the relationship between demographic variables and self-care ability, the results showed that age (P = 0.001), education (P = 0.002), and job type (P = 0.017) were related to self-care ability in patients. However, the relationship between age and self-care ability was reversed. Regarding the relationship between demographic variables and health-promoting behaviors, the results indicated no significant relationship between all dimensions of health-promoting behaviors and demographic characteristics in multiple sclerosis patients (P < 0.05).
5. Discussion
The current research is a descriptive-analytical cross-sectional study, and the research population comprised all patients with multiple sclerosis covered by the Multiple Sclerosis Association of Khuzestan province. The sample included 112 patients selected from the research community using the available sampling method. The results of the present study indicated the poor general self-care ability of the patients. However, 69.6% of the patients exhibited moderate self-care ability. Studies have similarly reported moderate self-care ability among patients with Multiple Sclerosis (31-33). Morowati et al. also found moderate self-care ability among MS patients (27), while Soodmand et al. observed desirable self-care ability in hemodialysis patients, attributing it to patients' carefulness about their diseases and conditions, and their efforts to strengthen factors that improve self-care ability (34). However, in the present study, the self-care ability of MS patients was poor. Given the chronic nature and complications of the disease and the necessity of self-care skills, the discussion on self-ability is crucial. It calls for the attention of health-sector authorities, policymakers, and administrators to plan for regular and recurrent self-care training, involving multiple sclerosis societies and nurses.
Regarding health-promoting behaviors, the results revealed the poor health lifestyle profile of patients, although 94.6% of the patients exhibited acceptable health-promoting behaviors. In line with the findings of the present study, Stuifbergen and Roberts (35) reported total HPLP scores of 140.4 in their research on female MS patients in the southwest of the United States. Conversely, Manavifar and Asaei examined patients with hypertension in Mashhad, Iran, and reported their health-promoting behaviors mean score at the undesirable level of 122.87 (ranging from 100 to 186) (36). However, Alizadeh et al. (37) in Iran reported moderate health-promoting behaviors among their examined patients, who were females under the coverage of Tabriz Multiple Sclerosis Society, while the statistical population of the present study comprised both genders.
On the other hand, the poor health-promoting behavior observed in our examined patients was expected, given that 40.17% had educational levels of diploma and below, and only 10.72% participated in educational courses held by the Society. This underscores the need for designing and planning programs to improve healthy behaviors and self-care ability in these patients. The results also revealed a significant relationship between health-promoting behaviors, their dimensions, and self-care ability. In this regard, Wang et al. studied older adults and found a direct and significant relationship between health-promoting behaviors and self-care ability (38). Similarly, in Iran, Abdolkarimy et al. examined health workers in Urmia (39), Farokhzadian et al. investigated university students in Isfahan (40), and Salahshouri et al. studied older adults in Dena (41), all concluding that self-efficacy had a strong positive and significant relationship with health-promoting behaviors.
Considering the findings of the present study, particularly the direct relationship between self-care ability and health-promoting behaviors, health authorities and administrators can facilitate the enhancement of chronic patients' health-promoting behaviors and self-care ability by implementing health-promoting programs. The chronic nature of the disease and its associated conditions influence health-promoting behaviors. Saadat explained that chronic conditions often lead to infrequent health-promoting behaviors in MS patients, emphasizing the need for relevant training through nursing and psychological interventions (29). Furthermore, the perception of the disease is linked to health-promoting behaviors in MS patients (12). Given the diverse cultural and social conditions of patients and their impact on disease perception, further studies on promoting disease perception and health-related behaviors in this patient group are recommended.
Regarding the relationship between demographic variables and self-care ability, age (P = 0.001), education (P = 0.002), and type of job (P = 0.017) showed a significant association with self-care ability. However, gender (P = 0.079), marital status (P = 0.411), economic status (P = 0.807), presence of other chronic diseases (P = 0.083), disease duration (P = 0.947), and participation in educational classes (P = 0.947) did not exhibit a significant relationship with self-care ability in multiple sclerosis patients. In this context, the findings of Kasiksi and Diapoglu's (31) and Eru Meloglu's (32) studies indicated that self-care ability increased with higher education levels in multiple sclerosis patients and decreased with advancing age. Soodmand, in a study on self-care ability among hemodialysis patients in Rasht, found that single individuals exhibited greater self-care ability due to their younger age and higher physical capacity. Additionally, men demonstrated greater self-care ability compared to women, potentially influenced by Iranian cultural norms where women often take on caregiving roles within families, possibly leading to less emphasis on self-care (34). In the present study, the age variable may have led to reduced attention to the disease over time due to its normalization and the occurrence of other chronic illnesses. Conversely, higher education levels and literacy among some patients may have resulted in increased awareness and knowledge, prompting greater attention to self-care behaviors.
Regarding the relationship between demographic variables and health-promoting behaviors, the results indicated no significant association between any dimension of health-promoting behaviors and overall health-promoting behavior with demographic characteristics in multiple sclerosis patients (P < 0.05). Dashti-Dehkordi et al. examined multiple sclerosis patients in Isfahan province and found that married patients exhibited higher levels of responsibility, spiritual growth, and nutrition-related behaviors compared to single patients (P < 0.05). Age was also inversely related to the physical activity dimension of health-promoting behaviors (22).
Manavifar and Asaei also noted, through a study on hemodialysis patients, that the responsibility dimension score was higher in women compared to men. Additionally, there was a significant inverse relationship between age and the total score of health-promoting behaviors (P < 0.05) (36). In the current study, unlike similar research, the chronic nature of the disease and its associated conditions likely influenced health-promoting behaviors. Saadat emphasized that chronic conditions correlate with decreased health-promoting behaviors in MS patients, highlighting the need for patient education through appropriate nursing and psychological interventions (29).
Furthermore, several facilitating factors and obstacles have been proposed to impact the understanding of the disease and consequently, behavior change in multiple sclerosis patients, underscoring the variation in disease comprehension across different societies (42). Since self-care behaviors tend to improve as perceived barriers decrease, and lack of awareness serves as a primary barrier to self-care behaviors, stakeholders involved in planning, implementation, and ongoing care, such as nurses who play crucial roles in the self-care of these patients, should concentrate their efforts on purposeful self-care training programs. These programs should be conducted regularly and patients should be followed up regarding their adherence to regular self-care activities (27). Considering the diverse cultural and social conditions among patients and their impact on disease comprehension, conducting further studies to enhance disease understanding and health-related behaviors in this patient group is recommended.
5.1. Limitations
This study encountered several limitations. Firstly, it only examined patients under the coverage of the Khuzestan Province Multiple Sclerosis Society, potentially excluding MS patients not affiliated with this Society. Therefore, caution should be exercised when generalizing the results to other MS patient populations. Additionally, the study's sample consisted solely of individuals above the age of 18, thus limiting the applicability of findings to younger patients. Furthermore, data collection relied on online questionnaires due to the concurrent Covid-19 pandemic, which may have affected the questionnaire completion process. Despite efforts to ensure proper completion conditions, the absence of patients at the Society and the lack of in-person visits may have influenced questionnaire responses, albeit beyond the researcher's control.
5.2. Conclusions
In summary, the findings revealed moderate levels of self-care ability and health-promoting behaviors among the MS patients surveyed. Recognizing the significant role of self-care activities in preventing disease complications and prolonging patient lifespan, it's imperative to enhance self-care ability and health behaviors. This not only alleviates the burden on healthcare facilities but also reduces healthcare system costs and enhances disease control and self-management. To achieve this, the Multiple Sclerosis Society, as the primary provider of health services to these patients, can develop and implement structured training programs tailored to the self-efficacy needs and capabilities of patients. Collaboration with other healthcare professionals such as physicians and nurses is essential in this endeavor. In addition to in-person programs, remote training and follow-ups via telephone or SMS can be effective. Moreover, given the infrequent nature of self-care behaviors, the Society, with support from state organizations and institutions, can facilitate and encourage patients to engage in self-care activities.