1. Background
Degenerative joint diseases are prevalent chronic conditions worldwide, with osteoarthritis (OA) being a prominent example (1). Osteoarthritis is a leading cause of disability both in the United States and globally (2). Its prevalence in Iran is reported as 15.1% (3). This disease causes various anatomical and physiological changes in joint tissues, such as cartilage degradation, bone regeneration, and the development of osteophytes (4). Given its high prevalence, OA is recognized as the most common joint disorder, and from 1990 to 2019, the global prevalence of KOA increased by 48%.3 (1).
Osteoarthritis affects various joints, including the hip, knee, spine, and finger joints. Among these, knee osteoarthritis (KOA) is a prevalent condition among older people, resulting from specific diseases or the natural aging process. Numerous studies conducted on the correlation between KOA and age suggest that degenerative changes, including those in the knee joint, occur as individuals grow older (5). Pain is the most common symptom experienced by individuals with KOA (6), and its alleviation is a primary focus of treatment (7). Additional symptoms of this condition include joint swelling, audible crepitus, joint effusion and soft tissue inflammation, joint deformity, limited range of motion, tenderness, and muscle weakness (8). Joint pain often leads to activity avoidance in these patients, which in turn contributes to muscle weakness (9).
There are various treatment methods available for managing knee osteoarthritis, including pharmaceutical, non-pharmaceutical, and surgical interventions (10). However, these treatments are primarily conducted in hospitals, specialized clinics, and physiotherapy centers, often incurring significant costs. Therefore, complementary treatment programs administered by non-specialists or even the patients’ families hold great potential in accelerating the recovery process and providing significant benefits for individuals with knee osteoarthritis (9).
Stretching exercises are commonly used as complementary treatments to improve muscle and joint flexibility in patients. Proprioceptive neuromuscular facilitation exercises (PNF) are a specific type of stretching exercise known for their effectiveness in enhancing flexibility through neurophysiological mechanisms (11). Maicki et al. compared the effects of PNF and manual therapy on patients with cervical spondylosis. They found that the PNF group outperformed their daily activities compared to the manual therapy group (12).
Given the high prevalence of knee osteoarthritis and the significant economic burden it imposes on both society and patients due to its chronic nature, it is crucial to explore alternative treatment options that can minimize unnecessary interventions and potential side effects associated with invasive procedures. Additionally, strengthening knee muscles plays a vital role in managing this condition. However, there is a limited number of studies demonstrating the effectiveness of treatments like PNF in improving muscle strength in patients with knee osteoarthritis. Therefore, the present study aimed to investigate the impact of PNF on muscle strength in patients with knee osteoarthritis.
2. Objectives
This study aimed to investigate the impact of proprioceptive neuromuscular facilitation techniques on the muscle strength of patients with knee osteoarthritis.
3. Methods
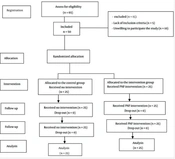
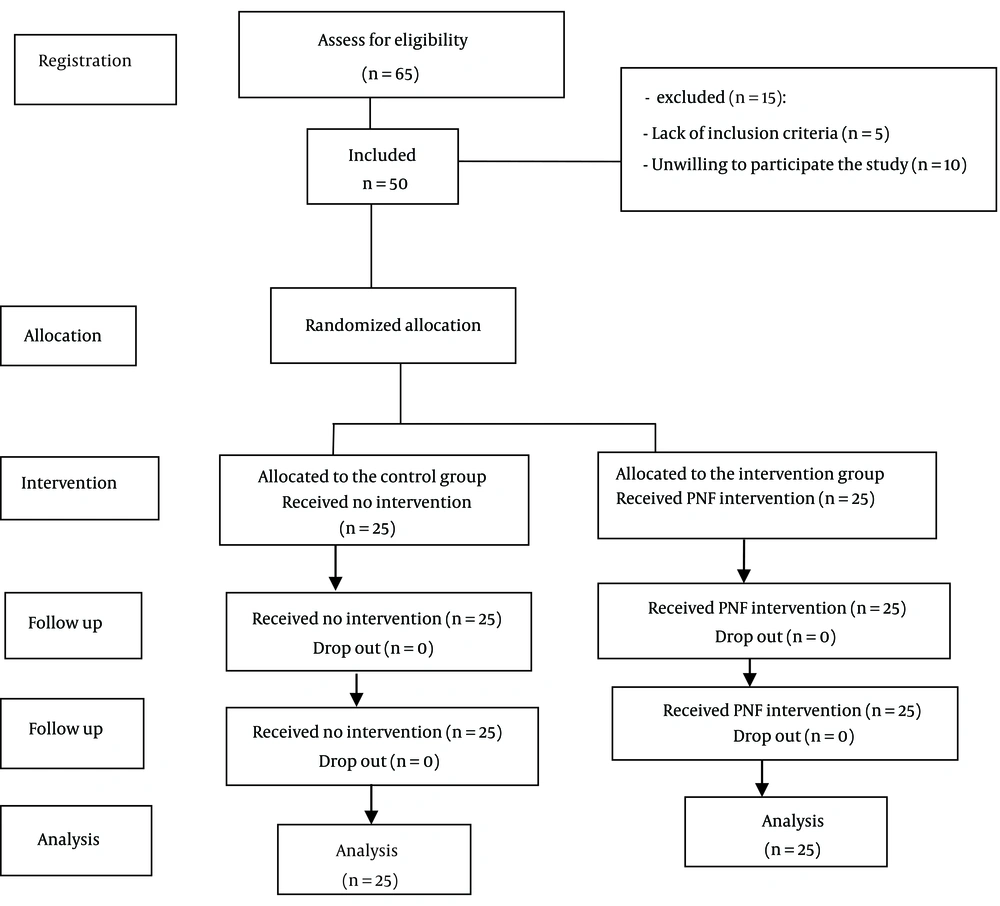
This quasi-experimental study consisted of fifty patients with knee osteoarthritis who were referred to orthopedic offices in Darab City in 2021. The sample size for each group was determined to be 25, based on the statistical formula and similar studies (13, 14), resulting in a total sample size of 50 patients. Non-probability sampling was used to select the patients, who were then divided into 2 groups: An experimental group and a control group. The allocation of participants into these groups was done by a block randomization method. This block randomization process used permuted blocks of size 2 to assign patients at a ratio of 1:10 to each of the two groups (Figure 1).
The inclusion criteria were as follows: Patient’s willingness to participate, age 40 to 65 years, presence of joint osteoarthritis in one or both knees confirmed by radiographic evidence and an orthopedic doctor, muscle strength of 3 or less, no history of surgery on the target joint (such as joint replacement or repair), and no previous participation in similar over the past 6 months. Exclusion criteria included disease exacerbation leading to hospitalization and non-participation in exercises for more than two sessions.
3.1. Measure
In this study, the muscle strength of patients with knee osteoarthritis was measured using a five-point scale. A score of 5 indicated complete muscle contraction against gravity, representing normal muscle strength. A score of 4 indicated good but not complete muscle strength against gravity, with moderate resistance or slight weakness. The score of 3 indicated moderate weakness, with sufficient strength only against gravity. A score of 2 indicated extreme weakness, where the person could move but not overcome gravity. A score of 1 indicated very severe weakness, where weak muscle contraction could be palpable, but no movement was observed. A score of 0 indicated no movement. Patients with a muscle strength score of 3 or less were included in the study. The validity and reliability of this manual muscle strength measurement scale have been confirmed in various medical reference books (11).
3.2. Intervention
The interventions were made in accordance with standard research practices, which involved explaining the research objectives, obtaining informed consent from participants, and obtaining a code of ethics from the Ethics Committee of Yasuj University of Medical Sciences. The experimental group received proprioceptive neuromuscular facilitation (PNF) techniques twice a week, with each session lasting between 30 to 45 minutes. In total, there were 16 sessions conducted over 8 weeks based on a specific protocol and instructions that were deemed relevant to the research.
In this study, stretching exercises were performed specifically targeting the quadriceps and hamstring muscles. To stretch the hamstring muscles, participants were asked to lie in a supine position with their knees open and then raise their dominant leg to flex the hip joint. To stretch the quadriceps muscles, participants were asked to lie in a prone position with bent knees, slightly lifting the thigh from the table to hyperextend the hip joint.
During the stretching exercises, a therapist applied pressure to the leg of the participants in a position where mild pain was felt. The participants were then instructed to hold the leg in that position for 30 seconds. Following this phase, an isometric contraction of the stretched muscle was performed for 10 seconds, followed by a 30-second resting period before returning to a new mild pain state. This procedure was repeated three times in each session, with 10 seconds of rest between stretches.
To ensure the safety of participants during the COVID-19 pandemic, interventions were conducted in a sports club while adhering to all health protocols. For male participants, a male researcher who was also a nurse assisted in carrying out the interventions. Prior to the intervention, patients were contacted to set the intervention time, which took place in the morning from 8 to 12 AM. It is important to note that no interventions were carried out for the control group, who solely received routine care.
3.3. Ethical Approval
The study protocol was approved by the Ethics Committee at Yasuj University of Medical Sciences (IR.YUMS.REC.1399.156).
3.4. Data Analysis
Data related to muscle strength were collected before, immediately after, and four weeks after the intervention. The collected data were analyzed using SPSS 21, descriptive statistics (such as central tendency and dispersion indices), and inferential statistics, considering a 95% confidence interval and a significance level of less than 0.05.
4. Results
Fifty patients with a mean age of 53.6 ± 10 completed this study, among whom 38 (76%) patients were female and 12(24%) were male. There were no statistically significant differences in demographic variables between the two groups (P > 0.05). The patients’ characteristics are shown in Table 1.
| Variables | Intervention | Control |
|---|---|---|
| Age | 7.9 ± 52.1 | 12.6 ± 55.2 |
| Sex | ||
| Male | 8 (32) | 4 (16) |
| Female | 17 (68) | 21 (84) |
| Marital Status | ||
| Single | 0 (0) | 1 (4) |
| Married | 25 (100) | 24 (96) |
| Residence place | ||
| Urban | 6 (24) | 6 (24) |
| Rural | 19 (76) | 19 (76) |
| Education | ||
| Less than Diploma | 19 (76) | 21 (84) |
| Higher than Diploma | 6 (24) | 4 (16) |
| Employment status | ||
| Employee | 2 (8) | 2 (4) |
| Housewife | 15 (60) | 20 (80) |
| Others | 8 (32) | 4 (16) |
| Family history of KOA | ||
| Yes | 15 (60) | 14 (56) |
| No | 10 (40) | 11 (44) |
Patients’ Characteristic a
The findings of the study indicated that mean scores of muscle strength for the patients in the interventional group significantly improved following PNF compared with those in the control group. In other words, the result of the repeated measure ANOVA for between-group comparison showed a statistically significant difference, i.e., by time and group, for mean scores of muscular strength parameters including degree (P = 0.001), percentage of normality (P = 0.001) and scale (P = 0.001). More statistical analysis indicated these differences were related to the time of the end of the intervention. However, there were no significant differences for times of pre-intervention and fourth week of intervention (Table 2).
| Variable/Time | Intervention | Control | Repeated Measure ANOVA (P-Value) |
|---|---|---|---|
| Degree | 0.001 | ||
| Pre-intervention | 2.8 ± 0.4 | 2.8 ± 0.3 | |
| 4th week of intervention | 2.8 ± 0.4 | 2.8 ± 0.3 | |
| End of intervention | 3.6 ± 0.6 | 2.8 ± 0.3 | |
| Percentage of normality | 0.001 | ||
| Pre-intervention | 45 ± 10 | 44 ± 12 | |
| 4th week of intervention | 45 ± 10 | 46 ± 9 | |
| End of intervention | 65 ± 14 | 45 ± 9 | |
| Scale | 0.001 | ||
| Pre-intervention | 2.8 ± 0.4 | 2.8 ± 0.3 | |
| 4th week of intervention | 2.8 ± 0.4 | 2.8 ± 0.3 | |
| End of intervention | 3.5 ± 0.6 | 2.8 ± 0.3 |
Between-Group Comparison of Mean Scores for Muscle Strength Parameters a
5. Discussion
In the present study, the effect of PNF techniques on the muscle strength of patients with KOA was investigated, as few studies have been conducted to investigate the effect of PNF on the muscle strength of patients suffering from KOA. Therefore, in order to compare the results of the present study with the results of other research, the studies that investigated the effect of PNF in other cases are mostly referred to. The results of the present study indicated that PNF increased the muscle strength of patients with KOA. Rhyu et al. conducted a study entitled “The effect of band exercise using proprioceptive neuromuscular facilitation on lower limb muscle strength”. The results of the study revealed that muscle strength exercises using the PNF model are effective in improving muscle strength, flexibility, and balance (15). The results of the research of Meena et al. also demonstrated that PNF with moist heat improves hamstring flexibility compared to static stretching with moist heat (16).
Moreover, this finding is in agreement with the results of other studies such as improving respiratory muscle strength in the study by Areas et al. (17), improving lung function in the research of Seo and Cho (18), improving the balance and performance of patients with patellofemoral syndrome in a study by Keyhanfar and Hosseini (19), and the improvement of daily life activities in the study by Kusumawati et al. (20), are in the same direction. The results of Masekar et al. (21) research, which compared the effect of PNF and Muscle Energy Technique (MET) on knee osteoarthritis, showed that PNF had a greater effect in improving pain, hamstring flexibility and range of motion in patients compared to MET. Also, the research results of Maia et al. (22) demonstrated that PNF improved the physical performance and quality of life of people with KOA.
On the other hand, the results of the study by Najafi et al. (23), which examined the effect of these interventions on the daily activities of stroke patients, emphasized the lack of effect of these interventions. This diverse result can be justified by the difference in the nature of the diseases since stroke causes a disconnection between the brain and muscles. Consequently, it is possible that performing these exercises did not affect their physical performance. Proprioceptive neuromuscular facilitation exercises consist of several movement patterns to facilitate and correct the motor commands of the brain by receiving messages from proprioceptive receptors in muscles. Modifying the disturbed patterns causes the establishment of order, facilitates the transfer of proprioception, and corrects the condition of joints and muscles (24). Guloglu et al. (25), in a study entitled “Efficacy of proprioceptive neuromuscular facilitation in improving shoulder biomechanical parameters, functionality, and pain after axillary lymph node dissection for breast cancer” concluded that PNF can improve muscle strength of the upper extremity, reduced pain during activity as well as improve functional status in patients with breast cancer.
The mechanism of the therapeutic outcomes of PNF methods in increasing muscle flexibility is neurophysiological and includes muscle stretch reflex. This mechanism increases the endurance of tension and improves muscle strength (11). The findings of the present intervention, which confirmed this issue, can be due to this underlying mechanism.
Therefore, it can be claimed that considering the benefits of these techniques and patients’ willingness to use rehabilitation methods in order to reduce the side effects of using drugs, it is necessary to consider such rehabilitation interventions along with medical care. These techniques should be taught to patients. Notwithstanding its strengths, the present study has limitations that need to be mentioned. One of the limitations of the present study was the small study sample. Therefore, it is suggested that future studies should be designed and conducted with a larger sample size and over an extended period. Moreover, the therapeutic exercises can be practiced at home in future studies under the supervision of a nurse.
5.1. Conclusions
The findings of this study demonstrated that the implementation of the PNF technique can increase muscle strength in patients with KOA. Moreover, as increasing muscle strength in these patients is one of the leading therapeutic goals, these rehabilitation methods should be considered in the treatment plan of these patients and be taught to them to improve their health. As the objective of these exercises is the provision of a better life for these patients, it costs less and is economical. Moreover, the patients’ family members can implement it, and they can benefit from it at any time. They are also effective in better disease control and reduce visits to healthcare facilities.