1. Background
Autism is a neurological disorder that appears in the early years of childhood. This disorder causes the brain to fail to function well in social behaviors and communication skills. Therefore, this disorder significantly hinders the child's ability to learn and develop skills related to socializing and interacting with others. Children with autism have problems with verbal and non-verbal communication, social behaviors, and playing games and have stereotyped and repetitive behaviors (1). According to the Centers for Disease Control and Prevention (CDC), 1 in every 150 children is currently diagnosed with autism (2). In Iran, the prevalence of autism in Iranian 5-year-old children was reported to be 6.26 per 10 000, and in this study, the disorder was reported to be 3 - 5 times higher in boys than in girls (3).
Sleep is a natural period of rest for the brain and body, in which consciousness is usually partially or totally lost. Therefore, body movements and responses to environmental stimuli are reduced. During this process, the brains of humans and other mammals go through a cycle of brain waves (4). About a third of human life is spent in sleep (5). Adequate sleep plays a crucial role in the mental and cognitive-motor development of adults and children (6). Lack of sleep can have adverse effects on endocrine function, cognitive function, metabolism, and inflammatory response (7). Sleep disturbance is very common in children diagnosed with autism spectrum disorder (ASD), with evidence supporting overlapping neurobiological underpinnings (8). Sleep disturbances and daytime sleepiness may aggravate the symptoms and behaviors of children with autism (9).
On the other hand, people follow unique sleeping habits. But surely, sleep habits have a significant effect on the sleep process (10). Following inappropriate habits and behaviors reduces the quality and quantity of good sleep (11). Thus, sleep disorders in a child (such as resistance to fall asleep, waking up during sleep, difficulty waking up in the morning, and parasomnia) can lead to reactions such as aggression, low concentration, and eating disorders (12). The results of a study showed that sleep behavioral problems are more common in children with autism than in normal children. Children with autism experience more resistance to falling asleep and refusing to stay in bed. Children with autism also experience more night waking. Studies have also shown that sleep behavioral habits in children with autism are significantly different from normal children (1).
Sleep problems are much more common in children with ASDs than in those with other developmental disorders and normal children. According to the literature, the reported prevalence of sleep problems in children with ASD ranges from 40% to 80% (13). Another study showed that sleep problems were recognized as one of the most common concomitant clinical disorders in children with ASDs (14). Another study reported that 53% of children with ASD between the ages of 2 and 5 years had at least 1 common sleep problem. One of the most common sleep problems in children with ASD is poor sleep. Parents often report that these children experience challenges when it comes to initiating or maintaining sleep (15). Another characteristic of children with autism spectrum is that they resist going to bed (16). Also, one of the major challenges in this group of children is that they often wake up during the night or wake up early in the morning (17). Due to the high prevalence of sleep problems in children with ASD, effective treatment in these children is necessary because sleep disorders may aggravate the symptoms of autism (18).
In this regard, pharmacological therapy is the first treatment line for these disorders (19). However, using sleeping pills to prevent sleep problems has many side effects. Therefore, in recent years, non-pharmacological and complementary methods to solve this problem have been studied (20). On the other hand, today, many parents who have a sick child attempt to use supplementary medicine and complementary therapies (21). The use of complementary therapies in nursing care is developing in many medical and care centers as a low-risk, cost-effective, and easily applicable approach with limited side effects (22). Foot reflexology massage is recognized as one of the existing therapies in complementary medicine (23) and holds a significant place among complementary therapies in nursing (24). It can be effectively used alongside medical treatments (25). Foot reflexology massage involves applying pressure to specific reflex points on the feet, including the solar plexus, pineal gland, and others. The basis of reflexology massage is the stimulation of these points and the use of nerve pathways that are related to various organs, glands, and systems of the body (26). According to the Chinese people, massage improves life energy by releasing neurotransmitters and nerve hormones (serotonin and melatonin), leading to less fatigue and improved sleep (27).
2. Objectives
Given the negative impact of sleep disorders on the physical, mental, and overall quality of life of children with ASD, as well as the limited research on the effects of complementary therapies in this population, and considering the ease of use, safety, and acceptance of complementary interventions by families and patients, the aim of the present study was to investigate the effects of foot reflexology massage on the sleep habits of children with ASD aged between 6 and 12 years.
3. Methods
3.1. Study Design
This study is a randomized controlled clinical trial that was performed in 2018-2019. It was approved by the Ethics Committee of Mashhad University of Medical Sciences (code: IR.MUMS.NURSE.REC.1398.020). Also, it was registered in the Iranian Registry of Clinical Trials (code: IRCT20190624043999N1).
3.2. Study Sample
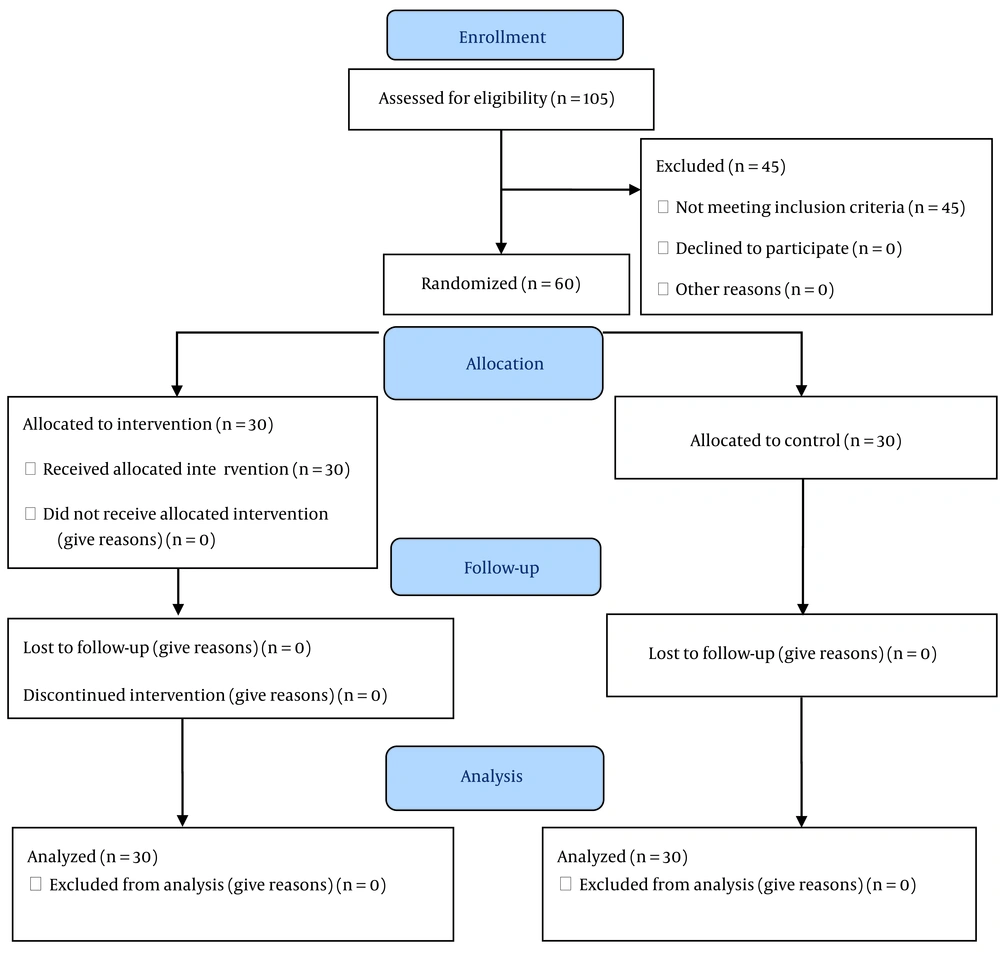
There are 10 autism centers for children, including Ruyesh, Navid Zendegi, Armaghan Noor, Takapoo, Ava, Kavosh, Noor Hedayat, Raha, Tabassom, and Mehr Kazem in Mashhad. Of these 10 centers, 3 centers of Ruyesh, Takapoo, and Kavosh were selected for the research setting by the simple random method. Considering that the dependent variable in this study (the score of sleep habit dimensions of children with ASD) was quantitative, the researcher used a formula to estimate the sample size based on the comparison of the mean and SD of the dependent variable in the 2 populations. Based on the findings of Rezaei and Alijani Ranani et al., the sample size for this study was determined to be 3 individuals (28, 29). Also, based on the findings of a pilot study on 10 children, a sample size of 28 people was determined. In calculating the minimum sample size, 95% CI, 80% test power, and 10% drop-out rate were considered. Finally, to increase the confidence in the research findings, the researcher performed a study and analyzed the data on 60 children (30 people in each group) (Figure 1).
3.3. Sampling
After approving the research design and obtaining a referral letter from Mashhad University of Medical Sciences, the researcher referred to the Welfare Organization and, after obtaining an agreement, referred to the autism centers that were affiliated with the Welfare Organization. To determine the sample size from each center, the researcher divided the sample size (n = 60) by the total population of children with ASD (n = 105). This calculation resulted in a fixed number of 0.57, known as the "sample size ratio." To obtain the sample size from each center, the researcher multiplied this ratio by the population of children with ASD in each respective center. Then, by having access to the list of children with ASD separately in each center, the initial sampling was done using the random number table. Finally, the children selected using a simple random method were divided into intervention and control groups.
3.4. Inclusion and Exclusion Criteria
Inclusion criteria were obtaining informed consent from parents, the child between the ages of 6 and 12 years, diagnosis of moderate autism by a psychiatrist, no stressful events (e.g., parents' divorce, death of a first-degree family member, parental dispute, and step-parents) during the last 3 months for the child, the absence of other physical and mental diseases in the child (such as hyperthyroidism, hyperactivity, arthritis, getting a sleep habit score higher than 41 according to Children's Sleep Habits Questionnaire [CSHQ]) (29), no specific problems (such as wound, burns, skin and fungal problems, paralysis, sensory disorders, local inflammation, lymphatic, venous, and vascular disease in the child's feet), not using sleeping pills, and lack of parental addiction. Exclusion criteria were not performing massage for more than 3 sessions by parents, self-medication of sedatives and drugs affecting sleep, and the occurrence of a stressful event during the study.
3.5. Instruments
The data collection instrument included a demographic information questionnaire (27 questions) and standard CSHQ. The Children's Sleep Habits Questionnaire is a standard sleep questionnaire for school-age children that reminds them of how they slept the previous week and is completed with the help of the child and his parents during the interview (30, 31). The questionnaire includes 8 main dimensions. These dimensions include bedtime resistance, sleep onset delay, sleep duration, sleep anxiety night waking, parasomnia, sleep-disordered breathing, and daytime sleepiness.
Of the 45 CSHQ questions, 33 are designed to identify these disorders. Also, some questions have inverse choices. The remaining 12 questions are used for diagnostic and therapeutic purposes and have no research value. Parents have 3 options to choose for each question, including usually (5 - 7 nights per week), sometimes (2 - 4 nights per week), and rarely (0 - 1 nights per week). The score of the questionnaire ranges from 33 to 99, in which a score above 41 indicates a disorder in sleep habits, and the higher the score, the more severe the sleep disorder (29). Also, a higher score indicates a lower quality of sleep (30, 32). Given that this instrument is quantitative, has 8 dimensions, and also has stratified choices, the reliability of this instrument is evaluated using internal consistency. Sleep habits scores were measured with this instrument among 15 children with ASD, and then Cronbach's alpha coefficient was obtained for each dimension and the total score. The alpha coefficients for the dimensions were between 0.63 and 0.87, and for the total score of sleep habits, it was 0.82.
3.6. Intervention
Before sampling, the researcher learned how to massage the foot reflexology massage in the presence of a traditional medicine specialist during sessions. In the intervention group, after providing a complete explanation of the research, the informed consent form was completed by the parents. Then, the demographic questionnaire form was completed by the parents. In the first period, to evaluate the sleep habits, standard CSHQ was completed by the researcher before the intervention and during the interview with the parents. Then, the parents in the intervention group were taught individually during the training session how to perform foot reflexology massage. To do the reflexology massage, the child was first asked to lie down in a comfortable position. Then, the child's feet were placed above the body by placing a pillow under them so that the baby's feet were facing the parent. After washing the hands and drying them to reduce friction, the parent rubs them using a neutral lubricant (Vaseline) (27). Initially, the parent performed a relaxing massage on both feet for 5 min (28). Relaxation here means the preliminary movements to prepare the feet. Preparing the feet included warming the feet with the hands by performing specific movements, including holding all parts of the feet with both hands and massaging the feet (27). Then, massaging continued for 10 min on the given areas on the soles of the toes of both feet, which are related to the head and pituitary glands. In this way, the parent supported the child's foot with one hand and, with the other hand, applied several rotational and circular pressures on the sole of the child's right and left toes. The given intervention (i.e., pressure on the mentioned area) was performed for 5 min (10 s of pressure and 2 s of rest). After 5 min, the same was done on the opposite side of the body (28). Massage therapy was performed by parents before going to bed for 15 min every night for a month (33). To ensure that the massage was done by the parents, they were given a notebook to honestly take notes if massaging was not performed. In addition, a text message was sent every night reminding them to massage their children. On the 15th day, the researcher completed the CSHQ to evaluate the child's sleep habits by interviewing the parents. Then, the massage was continued by the parent, and on the 30th day, which was the last session of the massage intervention, CSHQ was completed again during the interview with the parents to evaluate the child's sleeping habits.
In the control group, after giving a complete explanation of the research, the informed consent form was completed by the parents. The demographic questionnaire form was then completed by the parents. Also, in the first period, CSHQ was completed by the researcher during the interview with the parents to evaluate sleep habits. Then, on the 15th and 30th day after entering the study, CSHQ was completed again by the researcher to evaluate the child's sleeping habits during the interview with the parents.
3.7. Data Analysis
Finally, the data were statistically analyzed using SPSS version 16 with chi-square, independent t-test, and Mann-Whitney tests.
4. Results
Statistical tests showed that the demographic variables of the samples were homogeneous. The mean and SD of age of children with ASD was 8.8 ± 2.4 years in the intervention group and 8.3 ± 2.4 years in the control group. In each group, the minimum age was 6 years, and the maximum age was 12 years. The result of the independent t-test did not show a significant difference between the 2 groups (P = 0.46). Therefore, the 2 groups were homogeneous in terms of age. The children studied were 47 (78.34%) boys and 13 (21.66%) girls. The result of the independent t-test showed no statistically significant difference between the 2 groups in terms of sex frequency (P = 0.46). Therefore, the 2 groups were homogeneous in terms of gender. The mean and SD of weight of children with ASD was 28.2 ± 11.7 kg in the intervention group and 31.2 ± 11.7 kg in the control group. In the present study, the lowest weight of the children was 13 kg, and the maximum weight was 60 kg. The result of the independent t-test did not show a significant difference between the 2 groups (P = 0.33). Hence, the 2 groups were homogeneous in terms of weight variables. Regarding other demographic variables in this study, the results of statistical tests showed that the 2 groups were homogeneous in terms of these variables, and there was no statistically significant difference between the 2 groups (Table 1).
| Variables | Groups | Test Results | |
|---|---|---|---|
| Intervention | Control | ||
| Age (y) | 8.8 ± 2.4 | 8.3 ± 2.4 | P = 0.46, t = 0.46 |
| Height (cm) | 124 ± 18.2 | 128 ± 16.02 | P = 0.37, t = -0.91 |
| Weight (kg) | 28.2 ± 11.7 | 31.2 ± 11.7 | P = 0.46, t = 0.46 |
| Birth rank | 1.36 ± 0.61 | 1.56 ± 0.85 | P = 0.46, t = 0.46 |
| Gender | df = 1, chi-square = 0.88, P = 0.35 | ||
| Boy | 22 (73.3) | 25 (83.3) | |
| Girl | 8 (26.7) | 5 (16.7) | |
Frequency Distribution of Descriptive Variables of the Studied Samples a
Regarding the comparison of the total score of children's sleep habits in the control and intervention groups, the total score of children's sleep habits before the intervention was 45.30 in the intervention group and 45.90 in the control group. The mean total score of children's sleep habits before the intervention was not significantly different between the control and intervention groups (P = 0.71). Also, the total score of children's sleep habits after the intervention was 37.17 in the intervention group and 45.72 in the control group. The mean total score of children's sleep habits after the intervention was significantly different between the control and intervention groups (P = 0.001). The mean total score of children's sleep habits in the control group had no significant difference before and after the intervention (P = 0.47). However, the mean total score of children's sleep habits in the intervention group had a significant difference before and after the intervention (feet reflexology massage; P = 0.002). The results showed that foot reflexology massage had a significant impact on the score of sleep habits in the intervention group, with a score reduction of 8.13 ± 3.95 points (P = 0.002; Table 2).
| Dimension of Sleep Habits and Evaluation Stages | Control, Mean ± SD | Intervention, Mean ± SD | Results of Between-Group Analyses |
|---|---|---|---|
| Sleep time resistance | |||
| Before the intervention | 11.77 ± 2.87 | 11.97 ± 2.40 | t = -0.93 a, P ≤ 0.67 |
| 15th day of the intervention | 11.47 ± 3.01 | 9.97 ± 3.15 | Z = 2.16 b, P ≤ 0.03 |
| 30th day of the intervention | 11.30 ± 2.97 | 9.60 ± 3.28 | t = -2.10 a, P ≤ 0.004 |
| Delayed sleep onset time | |||
| Before the intervention | 1.92 ± 0.83 | 2.13 ± 0.80 | Z = -0.64 b, P ≤ 0.65 |
| 15th day of the intervention | 1.83 ± 0.84 | 1.93 ± 0.83 | Z = -1.44 b, P ≤ 0.42 |
| 30th day of the intervention | 1.70 ± 0.94 | 1.80 ± 0.73 | Z = -0.16 b, P ≤ 0.87 |
| Sleep duration | |||
| Before the intervention | 8.70 ± 2.21 | 8.83 ± 3.63 | t = -0.23 a, P ≤ 0.87 |
| 15th day of the intervention | 8.51 ± 2.40 | 6.70 ± 3.13 | t = -3.53 a, P ≤ 0.02 |
| 30th day of the intervention | 8.29 ± 2.31 | 6.52 ± 2.74 | t = -3.30 a, P ≤ 0.003 |
| Sleep anxiety | |||
| Before the intervention | 5.43 ± 1.97 | 5.13 ± 1.62 | t = 0.32 a, P ≤ 0.52 |
| 15th day of the intervention | 5.40 ± 1.83 | 4.99 ± 2.54 | t = 0.63 a, P ≤ 0.68 |
| 30th day of the intervention | 5.39 ± 1.52 | 4.80 ± 1.93 | t = -1.01 a, P ≤ 0.14 |
| Frequent night awakenings | |||
| Before the intervention | 4.03 ± 1.42 | 4.53 ± 1.63 | t = 1.26 a, P ≤ 0.21 |
| 15th day of the intervention | 4.16 ± 2.01 | 3.20 ± 2.28 | t = 1.74 a, P ≤ 0.09 |
| 30th day of the intervention | 4.13 ± 1.52 | 3.63 ± 1.95 | t = -1.10 a, P ≤ 0.27 |
| Parasomnia | |||
| Before the intervention | 6.10 ± 3.40 | 5.50 ± 3.40 | t = -0.77 a, P ≤ 0.45 |
| 15th day of the intervention | 6.20 ± 3.60 | 4.60 ± 3.01 | t = -2.34 a, P ≤ 0.04 |
| 30th day of the intervention | 6.07 ± 3.30 | 3.90 ± 2.30 | t = -2.90 a, P ≤ 0.005 |
| Respiratory diseases in sleep | |||
| Before the intervention | 2.03 ± 2.01 | 2.20 ± 1.40 | Z = -0.33 b, P ≤ 0.76 |
| 15th day of the intervention | 2.40 ± 2.40 | 1.40 ± 1.60 | Z = 2.33 b, P ≤ 0.03 |
| 30th day of the intervention | 2.40 ± 2.03 | 1.03 ± 1.40 | Z = 3.18 b, P ≤ 0.001 |
| Daily drowsiness | |||
| Before the intervention | 11.20 ± 2.92 | 12.73 ± 4.30 | t = 1.60 a, P ≤ 0.11 |
| 15th day of the intervention | 10.90 ± 3.30 | 10.23 ± 3.54 | t = -0.75 a, P ≤ 0.45 |
| 30th day of the intervention | 11.47 ± 3.34 | 10.13 ± 3.74 | t = 1.45 a, P ≤ 0.15 |
| Total score of sleep habits | |||
| Before the intervention | 45.90 ± 5.89 | 45.3 ± 6.66 | t = -3.4 a, P ≤ 0.001 |
| 15th day of the intervention | 45.33 ± 6.96 | 39.07 ± 9.52 | t = -0.37 a, P ≤ 0.71 |
| 30th day of the intervention | 45.72 ± 6.34 | 37.17 ± 8.13 | t = 5.2 a, P ≤ 0.001 |
| Results of the within-group analyses | F = 1.36 c, P ≤ 0.47 | F = 12.16 c, P ≤ 0.002 | F = 11.36 c, P ≤ 0.01 |
| The difference before the intervention and the 30 days after the intervention | -0.18 ± 3.52 | -8.13 ± 3.95 | t = 7.8 a, P ≤ 0.001 |
Mean Scores of Total Sleep Habits of Children with Autism in the Intervention and Control Groups
5. Discussion
Considering the general purpose of the study “to determine the effect of foot reflexology massage on the total score of sleep habits in children with autism,” the present study showed that foot reflexology massage had a significant impact on the mean total score of sleep habits in children with ASD. According to the results, after performing the feet reflexology massage, the mean total score of sleep habits in children with ASD decreased by 8.13. This score reduction was significant. However, no significant change was observed in the control group. Considering that as the total score of sleep habits decreases, the quality of sleep in children increases, it can be concluded that foot reflexology massage is effective in improving sleep quality in children with ASD.
The results of Rezaei in 2018 (28) are consistent with the present study. One of the reasons for this consistency is that the age of the children studied is the same (6 - 12 years) in both studies. Also, the questionnaire used in both studies (standard CSHQ) is the same. On the other hand, the intervention of both studies (foot reflexology massage) is similar. Also, the results of this study are consistent with the results of Shafiee et al. (34). Braun et al. investigated the effects of massage therapy on pain, anxiety, muscle spasms, postoperative relaxation, and satisfaction in patients undergoing heart surgery. Their findings indicate a reduction in pain, anxiety, and muscle spasms, as well as an increase in feelings of relaxation and satisfaction in patients undergoing massage therapy (35). This study is consistent with the present study in that both studies suggest that massage therapy may promote relaxation and potentially improve the sleeping habits of children.
In another study, Farrokhian et al. examined the “effect of foot reflexology massage on sleep quality of hemodialysis patients referred to Qazvin Bouali Hospital” on 62 hemodialysis patients. The general results of the study showed that the use of foot reflexology massage improved the sleep quality of hemodialysis patients (36). The results of this study are consistent with the present study, and the reason is the similarity of the type of intervention (foot reflexology massage) of both studies. Despite the different types of patients and the tools used, the general results of the 2 studies are consistent.
In Williams' study, conducted on 12 autistic children with learning disabilities, the intervention involved a 3-night massage using lavender oil. The results of the study showed that massage with lavender oil has no positive effect on the sleep patterns of children with autism (37). This result is not consistent with the result of the present study. Perhaps one of the reasons for this dissimilarity is the short duration of the massage (3 nights). Differences in the type of intervention can also be effective. In Williams' study, lavender oil massage was used for 3 nights, while in the present study, children with autism received foot reflexology massage for 1 month, as this difference can be in contradiction with the effective results. Also, considering that the sample size in Williams' study was small (12 people), the effect of this intervention on sleep quality would not be significant. Salimi et al. also conducted a study. The results of their study showed that aromatherapy was not effective in improving the sleep quality of burned patients (38). This result is not consistent with the overall result of the present study. Probably, the short time of the aromatherapy (20 minutes) has resulted in no significant effect on the sleep quality of the patients in this study.
The results of the multivariate analysis of variance of the statistical test showed that among all the variable dimensions of sleep habits, the effect of foot reflexology massage on the dimension of daytime sleepiness was higher than that of other dimensions. The findings of the present study showed that the foot reflexology massage is effective on the mean score of daytime sleepiness in children with autism; thus, after performing the foot reflexology massage, the mean score of daytime sleepiness in children with autism decreased by 2.60. This decrease in score was significant, but no significant change was observed in the control group. Surani et al. investigated “the effect of animated movies in combating child sleep health problems” in a study. The study was conducted on 264 children from 2 primary schools. The results showed that this intervention did not change the daytime sleepiness score (39), which is not consistent with the results of the present study. Perhaps the reason for this result was the increase in brain activity of children watching educational animation. In this regard, Rezaei study conducted on 60 children with leukemia showed that foot reflexology massage reduced daytime sleepiness (28). This result is consistent with the result of the present study. One of the reasons for this consistency is that the type of intervention and the way it is performed (foot reflexology massage) are the same in both studies.
5.1. Implication for Clinical Practice
Nurses can indeed provide training on reflexology foot massage to children, as well as caregivers, parents, and other family caregivers. This training can be facilitated through various educational resources such as pamphlets, software, and educational handbooks.
5.2. Conclusions
The results of the present study showed that foot reflexology massage is effective in improving sleep habits and increasing the quality of sleep in children with autism. Therefore, the research hypothesis “foot reflexology massage is effective in reducing the score of sleep habits in children between the ages 6 - 12 years with autism” was supported. Therefore, due to the high importance of sleep quality in children with autism, it can be said that the use of foot reflexology massage is recommended as a non-pharmacological, safe, easy, low-cost, and cost-effective method in improving sleep disorders in these children. It should be mentioned that the individual differences of the children under study can affect their sleep quality. Thus, it can be a limitation in this study. It is also suggested that future studies investigate the effect of foot reflexology massage on improving sleep quality in children with other types of diseases.