1. Background
Stroke is among the five leading causes of death in most countries (1). Moreover, since this condition causes cognitive, emotional, and physical disabilities and it is responsible for 3.6% of the total disability-adjusted life years (DALYs), it is considered one of the 10 causes of disability in all countries (2). Among all the neurologic diseases of adult life, stroke ranks first in frequency and importance (3). The common mode of expression of stroke is a relatively sudden occurrence of a focal neurologic deficit (4). Strokes are broadly categorized as ischemic or hemorrhagic. Ischemic stroke is due to occlusion of a cerebral blood vessel causing cerebral infarction (5). Based on the underlying causes, ischemic stroke is divided into 5 major categories of large artery atherosclerosis (15% - 40%), cardioembolic stroke (15% - 30%), small artery occlusion or lacunar stroke (15% - 30%), cryptogenic stroke (up to 40%), and other causes (5%) (6). The treatment of stroke may be divided into three parts: management in the acute phase by measures to restore the circulation and arrest the pathologic process, physical therapy and rehabilitation, and measures to prevent further strokes and progression of vascular disease (7). It is now a major goal of general medicine to reduce the incidence of stroke in the general population by the control of modifiable risk factors (“primary prevention”) (8). In addition to reduction of known risk factors such as hypertension, smoking, and glucose control in diabetics (9), the widespread use of cholesterol-lowering statin medications and antiplatelet drugs has shown in some studies to reduce the primary incidence of and recurrence of stroke (10). Atherosclerotic risk factors are the most common, and yet the most modifiable, risk factors for stroke. Atherosclerotic risk factors include high blood pressure, diabetes mellitus, smoking, and dyslipidemia (11). The discernable difference in recurrent stroke in different studies (ranging from 3% to 23.2%) (12, 13), despite the use of the same medical treatments for this disease in various communities, suggests the hypothesis that this difference can be attributed to the lack of appropriate control of modifiable risk factors for this condition in communities where the incidence of stroke is higher.
2. Objectives
The present study aimed at finding out whether strict control of atherosclerotic risk factors after the first stroke could reduce the chance of recurrent stroke.
3. Methods
3.1. Patients
In this randomized clinical trial study, 86 patients, diagnosed with ischemic stroke by neurologists and hospitalized in the neurology ward of Golestan hospital in Ahwaz, entered the study. The sample size according to previous studies (14) was calculated for each group as 36 patients. However, to compensate for sample loss, 43 patients were allocated to each group. The inclusion criteria were no history of heart valve problems, cardiac arrhythmia, congestive heart failure (ejection fraction < 35%), stenosis of more than 70% in the doppler ultrasound of the cervical vessels, and a national institutes of health stroke scale (NIHSS) of below 22 (15). Moreover, the exclusion criteria included inability of patients to participate in clinical assessments due to a medical condition.
3.2. Design
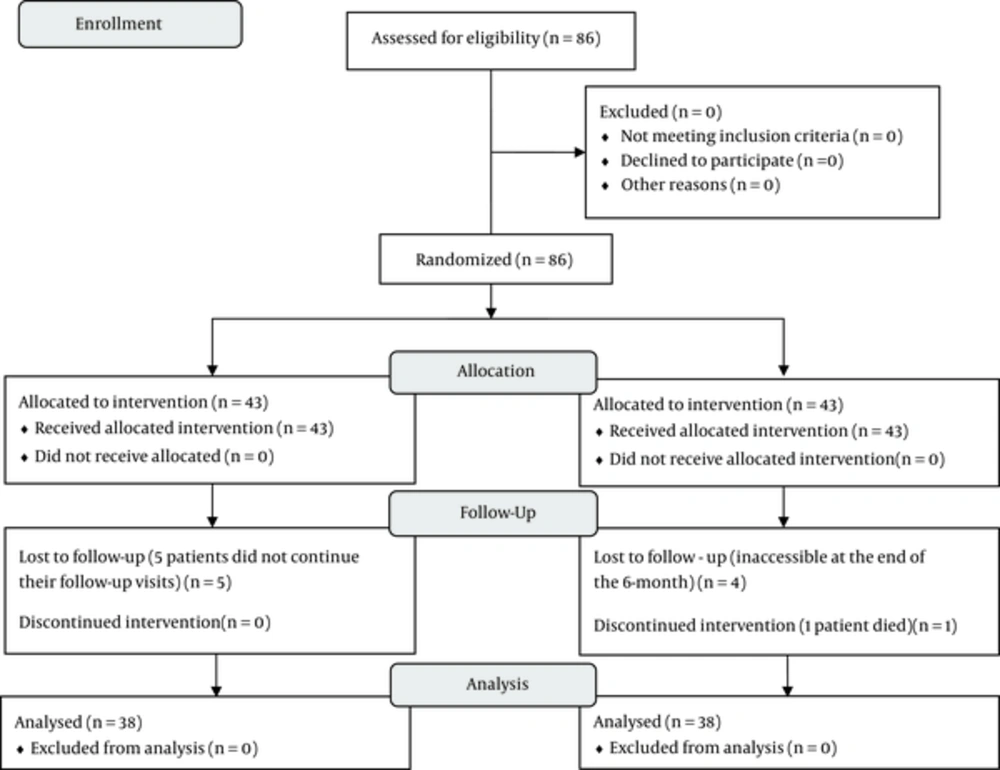
The subjects were assigned to two groups of active follow-up and non-active follow-up of risk factors using the block randomization method. The same medical procedures were conducted for both the groups during their hospitalization. The only difference between the two groups was in terms of the day of discharge; subjects in the non-active follow-up group only received oral recommendations for periodic visits to the specialized clinic of Golestan hospital (every two weeks for one month and then once every month for 6 months after discharge), while in the active follow-up group, in addition to oral recommendations, regular visits of patients to a physician at specified dates were reminded and followed up. At each visit to the physician, blood pressure, blood glucose, and low-density lipoprotein (LDL) of patients were measured and appropriate drugs were prescribed. Subjects in the active follow-up group at each visit and those in the non-active follow-up group at the end of the 6-month period were again questioned and examined in relation to recurrent stroke. Of the 86 patients who initially entered the study, 5 were excluded from the active follow-up group because they did not continue their follow-up visits. In the non-active follow-up group, 4 subjects were also eliminated because they were inaccessible at the end of the 6-month period. In addition, one patient in this group died of heart attack during the study and therefore, excluded from the research. As a result, a total of 76 patients completed the study. The study CONSORT flow diagram is shown in Figure 1.
3.3. Data Analysis
Statistical analysis was conducted using SPSS software (version 20). The percentage for the nominal variables was calculated. Mean ± standard deviation was calculated for each continuous variable. Odds ratio (OR) and exact poisson confidence intervals (CI) were calculated. For each group, prevalence of risk factors and recurrence of stroke were compared by paired-sample t - test. P value of less than 0.05 was considered statistically significant.
3.4. Ethical Considerations
This study was approved by the ethics committee of Ahvaz Jundishapur University of Medical Sciences (code: IR.AJUMS.REC.1394.22), and consent forms were obtained from all patients who participated in the research. The trial was registered at the Iranian registry of clinical trials (http://www.irct.ir) with the Irct ID: IRCT2015051212781N3.
4. Results
Of the patients in the present study, 64.8% were male and 35.2% were female. The mean age of the subjects was 65.9 ± 11.53 with a minimum and maximum of 41 and 90, respectively. At the start of study, there was no significant difference between subjects of the two groups in terms of gender, age, stroke site, diabetes mellitus, smoking history, dyslipidemia, blood pressure, and NIHSS (Table 1). At the end of the study, recurrent stroke was observed in 5 subjects of the non-active follow-up group (13.8%) and only in one subject of the active follow-up group (2.8%) (Table 2). The P value resulting from the comparison of recurrent stroke rate between the two groups was not significant at the level of 0.05. However, due to the closeness of the P value to the significance level (P = 0.089) and since the odds ratio of recurrent stroke in the non-active follow-up group was 5 times more than that in the active follow-up group (OR = 5, CI = 95%), it can be concluded that active follow-up of patients is effective in reducing the risk of recurrent ischemic stroke.
| HTN | Dyslipidemia | Smoking | Diabetes Mellitus | NIHSSa Mean | |||||
|---|---|---|---|---|---|---|---|---|---|
| - | + | - | + | - | + | - | + | ||
| Active follow-up | 14 (36.8%) | 24 (63.2%) | 29 (76.3%) | 9 (23.7%) | 27 (71.1%) | 11 (28.9%) | 23 (60.5%) | 15 (39.5%) | 14.81 |
| Non-active follow-up | 12 (31.6%) | 26 (68.4%) | 27 (71.1%) | 11 (28.9%) | 28 (73.7%) | 10 (26.3%) | 23 (60.5%) | 15 (39.5%) | 14.13 |
| P value | 0.629 | 0.602 | 0.798 | 1.000 | 0.405 | ||||
Comparison of the Prevalence of Risk Factors Between Two Groups at the Start of the Study
| Group | ||||
|---|---|---|---|---|
| Non-Active | Active | P Value | Odds Ratio | |
| With recurrent stroke | 5 (13.2%) | 1 (2.7%) | ||
| Without recurrent stroke | 33 (86.8%) | 37 (97.3%) | 0.089 | 5 (CI = 95%) |
Comparison of Recurrent Stroke Rate Between Two Groups at the End of the Study
5. Discussion
Stroke is one of the leading causes of mortality and morbidity in different communities. Therefore, stroke prevention is one of the main goals of health systems. Recurrent stroke increases the risk of mortality and morbidity caused by stroke. It seems the control of modifiable risk factors for stroke can reduce the odds of recurrent stroke in patients previously experiencing a stroke. Shamsaei et al., in a study on 590 patients, showed that high blood pressure was a risk factor for recurrent stroke (16). Mazdeh et al. also conducted a study on 5413 subjects and concluded that the major risk factors for stroke recurrence included high blood pressure, diabetes mellitus, smoking, and dyslipidemia (17). Therefore, in the present study, high blood pressure, diabetes mellitus, dyslipidemia, and smoking were identified as the most important risk factors for recurrent ischemic stroke. In this study, the rate of recurrent stroke within 6 months from the beginning of the study was 2.7% in the active follow-up group and 13.8% in the non- active follow-up group. In addition, the odds ratio in the non-active follow-up group was 5 times more than the active follow-up group.
The rate of recurrent stroke in the active follow-up group was close to the findings of Achterberg et al. (2013) in the Netherlands who reported that the risk of recurrent stroke after the first stroke of small artery and large artery was 3.3% and 2.9% per year, respectively (12). These figures were also similar to the results of a meta-analysis carried out by Mohan et al. (2014) on 9115 patients in Europe and north American countries, finding that the cumulative risk of recurrent stroke (ischemic and embolic) was 3.1% within the first month and 11.1% within the first year (18). By contrast, the rate of recurrent stroke in the non- active follow-up group was consistent with the findings of Mazdeh in Hamedan, I.R.Iran, who reported that the risk of recurrent stroke in patients was 17.35% (17). This was also similar to the rate of recurrent stroke (23.2%) reported by Ghandehari (2013) in Mashhad, I.R.Iran (13). All in all, considering the difference between the active and non-active follow-up groups in terms of recurrent stroke rate (that was five times higher in the non-active group than in the active group), the similarity of recurrent stroke rate obtained in non-active follow-up group on this research with the findings in previous studies in Iran, and also the similarity of this rate in the active follow-up group with that in more advanced societies where the risk factors are controlled accurately and actively, it can be concluded that active follow-up of patients with stroke and strict control of risk factors can lead to reduced rate of recurrent stroke and consequently, the attributed rates of mortality and morbidity.
5.1. Limitations
Because of the small number of patients with recurrent stroke in this study, the relationship between risk factors and recurrent stroke was not specified. It is recommended to conduct a similar study with a larger sample size to find the relationship between risk factors and the incidence of recurrent stroke.
5.2. Conclusion
According to the results of the present study, active follow-up of patients after the first stroke and strict control of ischemic stroke risk factors can reduce the rate of recurrent stroke.