1. Background
Maternal near miss (MNM) is defined as experiencing very severe complications immediately before or up to 42 days after delivery (1). The prevalence of MNM is estimated to be 18.67 per 1000 live births, most of which occur in low- and middle-income countries (2). In a study on 19,908 live births, Naderi et al. found that the prevalence of MNM was 25.2 per 1000 live births in Iranian women, with governmental hospitals accounting for higher rates (3). Pre-eclampsia/eclampsia, hemorrhage, sepsis, and ruptured uterus have been reported as the main causes of MNM (4). A study in Iran showed that the lower number of antenatal care visits, longer length of labor, and place of residence (rural vs. urban) were important factors contributing to MNM (5).
There is some evidence showing that MNM negatively affects women’s quality of life, causing post-traumatic stress disorders and impaired physical quality of life (6). Although Von Rosen et al. confirmed that MNM can decrease the quality of life and impair the mental and social health of women, they reported no negative effect on sexual function from the viewpoint of women (7).
There is also evidence that MNM may adversely affect sexual function later in life. Andreucci et al. found that women with severe complications during childbirth experience more dyspareunia and restart their sexual relationships after a longer delay compared to women without MNM (8). In their study of 110 women in the postpartum period, Alves et al. found that women suffering from severe maternal complications were more likely to have dyspareunia compared with women who did not have these complications (9).
The effect of different methods of counseling on sexual function has been evaluated in other studies (10, 11). One of these methods is cognitive-behavioral therapy (CBT), which is a type of psychotherapeutic treatment that helps people deal with negative and disturbing thoughts that negatively affect their quality of life (12). Cognitive-behavioral therapy focuses on changing both behavioral and cognitive domains (13). Several studies have evaluated the effect of CBT on the sexual function of women in different stages of life. For instance, Babakhani et al. studied 198 women with sexual dysfunction and found that women who received 4 sessions (each 2 hours) of CBT had a significant improvement in all sexual domains compared to the control group (14). In another study on 60 pregnant women, Nezamnia et al. reported that eight sessions of counseling based on CBT could significantly improve sexual function as well as self-efficacy in pregnant women (15). However, to the best of our knowledge, few, if any, studies have addressed the effect of CBT on the sexual function of women with MNM.
2. Objectives
This study aimed to evaluate the effect of an eight-week CBT counseling on the sexual function of women with near-miss. We hypothesized that CBT can improve the sexual function of these women.
3. Methods
This was a randomized controlled trial conducted on 60 women with MNM. Women with the following characteristics were recruited for this study: Total score of sexual function < 26, parity ≥ 1, basic literacy, experiencing near-miss during recent delivery, and being at 8 - 12 weeks after delivery. The diagnosis of near miss was done according to the World Health Organization and by having one or more of the following criteria: Cardiovascular dysfunction, including shock, cardiac arrest, use of continuous vasoactive medications, cardiopulmonary resuscitation, and severe hypoperfusion. Respiratory dysfunction includes acute cyanosis, gasping, severe tachypnea, severe bradypnea, intubation, and ventilation not related to anesthesia, and severe hypoxemia. Renal dysfunction, coagulation/hematological dysfunction, hepatic dysfunction, neurological dysfunction, and uterine dysfunction (16). The diagnosis of MNM was confirmed by a gynecologist. Furthermore, the names and characteristics of participants with MNM are recorded on a national site. Women with known psychological disorders (self-report) and those who were under psychiatric medication were excluded from the study.
3.1. Sampling
Following a previous study (17) and using the following formula, the sample size was calculated to be 24 in each group:
µ1=22, α1=0.05, β=0.1, SD1=1.08, SD2=0.99, z-
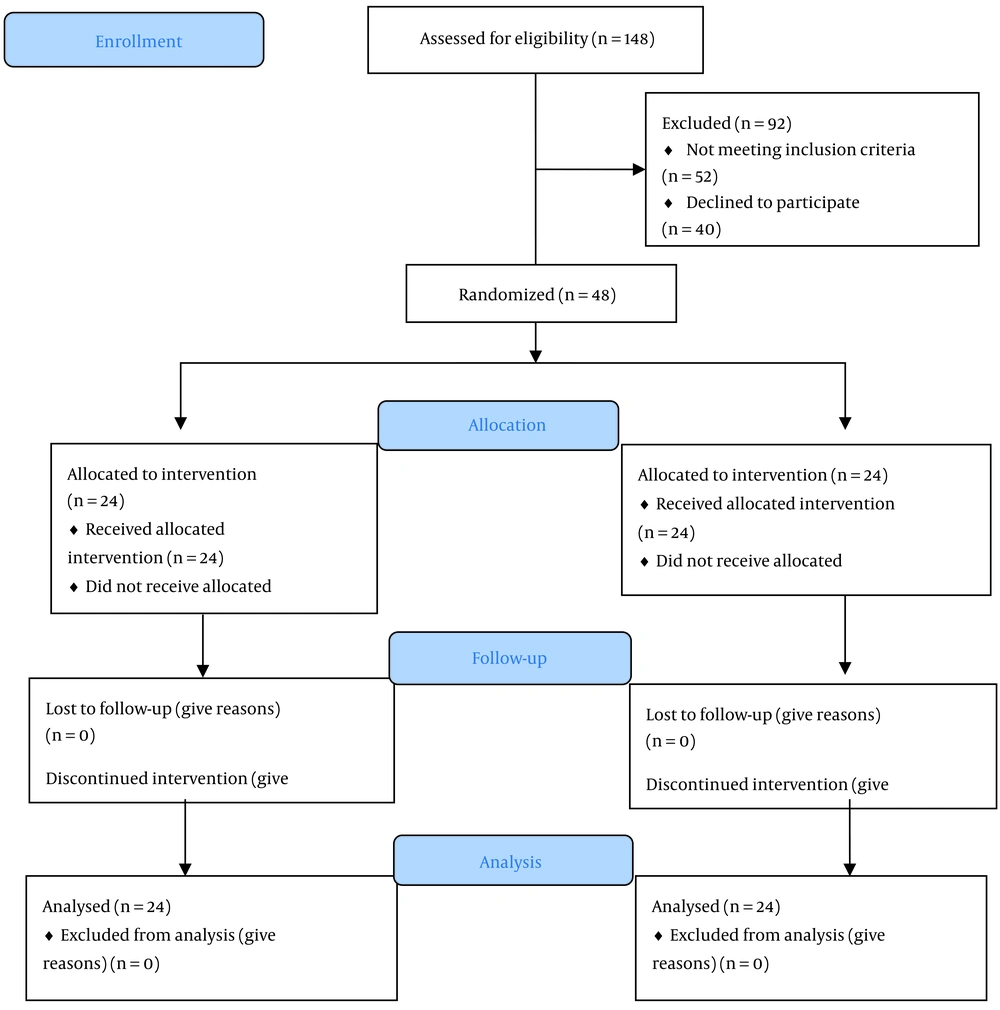
In each group, there were 24 participants, and a total of 48 participants were considered across the 2 groups. The anticipated effect size for this research was 0.8.
3.2. Randomization
In this study, we employed block randomization with a block size of 4 and an allocation ratio of 1:1. For allocation concealment, the codes designated for participants were held by the hospital clerk until the commencement of the study. Therefore, neither the researchers nor the participants were aware of group allocation before the start of the study. Due to the nature of the study, blinding of the researcher and participants was not possible.
3.3. Setting
Health records of women with MNM were screened on the national website, and those who were residents of Ahvaz and eligible to participate were invited to attend 2 public health centers in Ahvaz, Iran. The intervention started in June 2021 and was completed in October 2021.
3.4. Intervention
Participants in the CBT group attended eight CBT counseling sessions, each lasting 60 - 90 min. The content of the sessions was as follows:
- Session One: After greetings and getting introduced to the researcher, the participants received some information about near-miss and how this disorder can negatively affect the quality of life and sexual function. They were also trained on ways to improve thinking and feeling, the criteria for effective communication, the main elements of communication, verbal and non-verbal communication, active listening, barriers to effective communication, and healthy and non-healthy communication. The outline of the next sessions was presented.
- Session Two: The first session was reviewed. The following issues were presented: The anatomy and physiology of the male and female reproductive system, classification of beliefs, anxiety, recognition of spontaneous thoughts, how to identify possible resistance and methods to prevent it, methods of relationship management, and relaxation.
- Third session: In this session, the following issues were presented: Thought review, vertical arrow method, sexual function physiology in men and women, techniques of spontaneity, tension, and related factors, characteristics of stressful situations, signs and symptoms of stress, and stress management.
- Session Four: In this session, the following topics were presented: Vertical arrow review (Vertical Arrow/Downward Arrow/Vertical Descent is a form of Socratic questioning in which the therapist asks a succession of questions to uncover intermediate-level and core beliefs. Automatic thoughts often reflect moment-by-moment concerns, worries, or fears), advanced vertical arrow, types of beliefs, problem-solving-oriented and emotion-oriented confrontations, adaptation, and fantasy techniques.
- Session Five: The contents of this session were as follows: Preparing a list of beliefs, teaching the techniques of focused attention, cognitive mapping, time management, goal setting, daily and non-daily to-do-list and administrative tasks, prioritization based on importance and urgency, self-improvement and behavioral activation, and weekly planning of time management barriers.
- Session Six: The following issues were presented in this session: Ways of changing beliefs, teaching the techniques of sexual concentration, reality analysis, objective analysis, standard analysis, coping with negative emotions, cognitive reconstructions, identifying the relationship between thoughts and emotions, identifying cognitive errors, and challenging errors with negative thoughts.
- Session Seven: In this session, the following topics were presented: Teaching sexual concentration techniques, self-reliance, and a discussion of inconsistent and irrational thoughts.
- Session Eight: Summary of previous sessions, review of assignments, self-examination sheets, and discussion of inconsistent and irrational thoughts, teaching different positions, and discussing attitude and practices.
In each session, participants were requested to complete assignments at home based on what they had learned in that session. All counseling sessions were conducted by one of the researchers' Standard deviation (SD) under the supervision of a psychiatrist. Standard deviation participated in the CBT workshop and received a certificate. The content of the sessions was designed by one of the researchers (SN, a psychiatrist) using scientific literature and his experience in treating different patients based on Iranian culture.
Due to the COVID-19 pandemic in Iran, participants were classified into 3 groups of eight, social distancing was observed, and facial masks were provided for participants free of charge. To ensure compliance with the treatment, the researcher made phone calls to women at least once a week. Some small gifts, such as a telephone charge card, were given to the women in the intervention group. All sessions were conducted in the meeting hall of 2 public health centers.
The control group received routine care, and after the completion of the study, one educational session was offered to them. In this session, they were briefly informed about important issues that could improve their sexual performance.
3.5. Measurements
A demographic questionnaire and the Female Sexual Function Index (FSFI) were used to collect data. The former contained questions about age, occupation, age of the husband, educational attainment, and economic status. The validity of this questionnaire was approved through content validity.
The Female Sexual Function Index (FSFI) was developed by Rosen et al.. It consists of 19 questions in 6 domains, including sexual desire (2 questions), sexual arousal (4 questions), lubrication (4 questions), orgasm (3 questions), satisfaction (3 questions), and pain (3 questions). Each question is scored from 0 to 5, with 0 indicating no sexual relationship in the past month and 5 indicating optimal sexual function. Questions in the pain dimension were reversely scored. The sum score of each domain was multiplied by a certain factor (0.6 for desire, 0.3 for arousal and lubrication, and 0.4 for other domains). The total score of the FSFI questionnaire ranged from 0 to 36, and scores less than 26 indicated sexual dysfunction (18). The validity and reliability of this questionnaire were approved by Fakhri et al. in Iran (19). Women were requested to complete the demographic and FSFI questionnaires, and one of the researchers SD was available in case they had any questions. Data collection started in May and was completed in August 2021.
3.6. Ethical Considerations
The protocol of the study was approved by the Ethics Committee of Ahvaz Jundishapur University of Medical Sciences (Ref. ID: IR.AJUMS.REC.1399.255). Also, the protocol of the study was registered in the Iranian Registry of Randomized Controlled Trials (Ref. ID: IRCT20200612047744N1, All participants provided written informed consent before data collection.
3.7. Statistics
Data were analyzed using SPSS v. 22. The Shapiro-Wilk test was employed to test the normality of continuous data. The independent t-test was used to examine the differences between the 2 groups for numerical data, while the Chi-square test was used to examine the differences between the 2 groups for categorical data. In this study, 2 variables (i.e., orgasm and total score of sexual function) were significant before intervention. Since the data were not normal, it was not possible to perform an ANCOVA test to adjust the effect of these 2 variables. Therefore, we subtracted the mean scores of post-intervention from pre-intervention and then applied the Mann-Whitney test. P < 0.05 was considered statistically significant.
4. Results
In this study, 48 women with MNM were recruited and randomized into 2 groups, and no one dropped out of the study (Figure 1). Demographic characteristics of the participants are presented in Table 1. The mean age of women was 30.5 and 29.1 years in the CBT and control groups, respectively. Most of the participants had high school diplomas and one child. The dominant mode of delivery in the CBT group was cesarean (54.2%), while most women in the control group had a normal vaginal delivery (62.5%). The most prevalent cause of near miss was preeclampsia/eclampsia (50% and 41.7% in the intervention and control groups, respectively). The second cause of near miss was placenta accreta and increta (20.8% and 25% in the intervention and control groups, respectively).
| Variables | Mean ± SD or n (%) | P-Value | |
|---|---|---|---|
| CBT, N = 24 | Control, N = 24 | ||
| Age (y) | 28.21 ± 6.9 | 29.42 ± 6.53 | 0.53 a |
| 20 - 30 | 15 (62.5) | 16 (66.7) | 0.940 b |
| 31 - 40 | 6 (25) | 5 (20.8) | |
| > 40 | 3 (12.5) | 3 (12.5) | |
| Age of husband (y) | 33.58 ± 6.9 | 32.96 ± 7.5 | 0.76 a |
| Education | 0.82 b | ||
| High school | 5 (20.8) | 6 (25) | |
| Diploma | 10 (41.7) | 11 (45.8) | |
| University education | 9 (37.5) | 7 (29.2) | |
| Mode of delivery | 0.24 b | ||
| Normal vaginal delivery | 11 (45.8) | 15 (62.5) | |
| Cesarean | 13 (54.2) | 9 (37.5) | |
| Number of children | 0.66 b | ||
| No children | 7 (29.2) | 6 (25) | |
| 1 | 11 (45.8) | 8 (33.3) | |
| 2 | 2 (8.3) | 3 (12.5) | |
| ≥ 3 | 4 (16.7) | 7 (29.2) | |
| Causes of near-miss | 0.85 b | ||
| Hypertension and diabetes | 4 (16.7) | 4 (16.7) | |
| Heart disease | 1 (4.2) | 2 (8.3) | |
| placenta accreta, increta | 5 (20.8) | 6 (25) | |
| Preeclampsia/eclampsia | 12 (50) | 10 (41.7) | |
| Uterine atony, rupture, postpartum hemorrhage | 2 (8.3) | 1 (4.2) | |
| Perforation of ectopic pregnancy | 0 | 1 (4.2) | |
Socio-Demographic Characteristics of Participants in Two Groups of CBT and Control
Table 2 shows the mean score of sexual function in different domains in the 2 groups before intervention. As this table shows, the score of all domains of sexual function was low in the 2 groups. The score of orgasm (0.86 ± 0.38 vs. 2.10 ± 0.61, P = 0.001) and the total score of sexual function (15.32 ± 1.50 vs. 16.32 ± 2.58, P = 0.001) were significantly lower in the control group compared to the CBT group.
| Variables | Mean ± SD | P-Value | |
|---|---|---|---|
| CBT, N = 24 | Control, N = 24 | ||
| Sexual desire | 2.32 ± 0.48 | 2.32 ± 0.51 | 0.75 |
| Sexual arousal | 2.31 ± 0.64 | 2.42 ± 0.49 | 0.83 |
| Lubrication | 2.72 ± 0.68 | 2.68 ± 0.43 | 0.24 |
| Orgasm | 2.10 ± 0.61 | 0.86 ± 0.38 | 0.001 |
| Sexual satisfaction | 2.76 ± 0.79 | 2.83 ± 0.81 | 0.71 |
| Pain | 4.11 ± 0.93 | 4.18 ± 0.52 | 0.87 |
| Total score of sexual function | 16.32 ± 2.58 | 15.32 ± 1.50 | 0.002 |
Sexual Function and its Components in Two Groups of CBT and Control Before Intervention a
The scores of sexual functions and their domains in the 2 groups are presented in Table 3. As evident from this table, the mean scores of all sexual domains improved significantly in the CBT group compared to the control group (P < 0.001).
| Variables | Mean ± SD | P-Value | |
|---|---|---|---|
| CBTN = 24 | ControlN = 24 | ||
| Sexual desire | 3.77 ± .64 | 2.25 ± .53 | < 0.001 |
| Sexual arousal | 3.72 ± .45 | 2.40 ± .48 | < 0.001 |
| Lubrication | 3.13 ± .35 | 2.60 ± .36 | < 0.001 |
| Orgasm | 3.11 ± .45 | 1.0 ± .42 | < 0.001 |
| Sexual satisfaction | 4.25 ± .52 | 2.83 ± .81 | < 0.001 |
| Pain | 2.36 ± .80 | 4.21 ± .54 | < 0.001 |
| Total score of sexual function | 20.37 ± 1.44 | 15.3 ± 1.40 | < 0.001 |
Sexual Function and its Components in Two Groups of CBT and Control After Intervention a
Because orgasm and the total score of sexual function were significantly different before the intervention, we used change analysis and the Mann-Whitney U test to eliminate the effect of these 2 factors. The results of the change analysis are presented in Table 4. As can be observed in this table, the change in the mean score was dominant in the CBT group in comparison to the control group (P < 0.001).
| Variables | Change Analysis | Mann-Whitney U test | P-Value |
|---|---|---|---|
| Mean ± SD | |||
| Sexual desire | 0.000 | < 0.001 | |
| Control, n = 24 | -0.0750 ± 0.202 | ||
| CBT, n = 24 | 1.47 ± 0.66 | ||
| Sexual arousal | 23.00 | < 0.001 | |
| Control, n = 24 | -0.025 ± 0.151 | ||
| CBT, n = 24 | 1.41 ± .817 | ||
| Lubrication | 134.05 | < 0.001 | |
| Control, n = 24 | -0.087 ± 0.348 | ||
| CBT, n = 24 | 41 ± .77 | ||
| Orgasm | 36.00 | < 0.001 | |
| Control, n = 24 | 0.133 ± 0.326 | ||
| CBT, n = 24 | 1.01 ± .56 | ||
| Sexual satisfaction | 12.00 | < 0.001 | |
| Control, n = 24 | 0.000 ± 0.000 | ||
| CBT, n = 24 | 1.48 ± .75 | ||
| Pain | 24.00 | < 0.001 | |
| Control, n = 24 | 0.033 ± .163 | ||
| CBT, n = 24 | -1.75 ± 1.35 | ||
| Total score sexual function | 20.500 | < 0.001 | |
| Control, n = 24 | -0.020 ± 0.577 | ||
| CBT, n = 24 | 4.05 ± 3.07 |
Differences between two Groups of CBT and Control Using Change and Mann-Whitney Analyses
5. Discussion
This study aimed to evaluate the effect of CBT on the sexual function of women with near miss. Our results showed that eight sessions of CBT could improve all domains of sexual function. In the present study, we recruited women who experienced life-threatening situations during or after childbirth. A systematic review including 14 studies showed that most morbidities after childbirth were related to perineal lacerations, while near-miss is applied to those situations where women experience severe complications. Overall, dyspareunia and delay in reassuming sexual relationships were the most common sexual complications that these women reported (7).
We could not find any similar study to evaluate the effect of CBT on the sexual function of women with near miss. However, some studies have evaluated the effect of CBT on women in other critical situations. For example, Abdollahpour et al. conducted a study on 179 women who experienced a traumatic childbirth and assigned them into 3 groups: Debriefing, brief cognitive behavioral therapy, and a control group. Their results showed that 12 weeks after delivery, women in the 2 intervention groups showed a significant reduction in the score of depression compared to the control group (20). Also, Malakouti et al., in a study on 68 postpartum women, found that using the Ex-PLISSIT model could significantly increase the scores of sexual function and marital satisfaction (21). Our results are in line with those of Abdollahpour et al. and Malakouti et al (20, 21).
Other studies have also evaluated the positive effect of CBT on sexual function and satisfaction. (20, 21) Amini et al., for example, studied 60 women assigned to three groups of CBT: Empathy, intimacy, sexual satisfaction (EIS), and control (22). They found that 8 sessions of intervention could significantly improve all domains of sexual function. However, the effect of EIS was more dominant. In a randomized controlled trial, Nezamnia et al. found that 8 sessions of CBT could improve the scores of self-efficacy and sexual function in pregnant women (15). Our results are in line with those of Amini et al. and Nezamnia et al. (15-22).
Although the number of women with MNM who underwent cesarean section was more than that of women undergoing normal vaginal delivery in the present study, this difference was not significant between the 2 groups. Mohammadi et al. found that women who undergo cesarean section before the onset of labor experience more maternal near-miss than those experiencing normal vaginal delivery (23). Also, our results showed that the most prevalent causes of near miss were preeclampsia/eclampsia, placenta accreta, and increta. The latter could be attributed to the high prevalence of cesarean section in Iran. According to the latest reports, the prevalence of cesarean section in Iran is 47.9% (24). Although limited studies in Iran have shown that the complications of vaginal delivery after cesarean section (VBAC) are less than those of repeated cesarean section, the number of gynecologists who can take responsibility for VBAC is very small (25).
5.1. Strengths and Limitations of the Study
The scarcity of studies on the sexual function of women with MNM, coupled with the higher incidence of MNM due to the increased rate of cesarean section in Iran compared to other countries, underscores the necessity of conducting studies like the present one. However, despite its strengths, this study has some limitations. First, discussing sexual matters may not be convenient for Iranian women, potentially influencing their responses in this study. Second, we did not assess the sexual function of male partners, which could have also impacted our results.
5.2. Implications or Recommendations
Although cognitive-behavioral therapy has significantly improved sexual function in near-miss women, the overall score of sexual function remains lower than normal. This suggests that these women may require more extended counseling sessions or alternative interventions. Further intervention studies with longer follow-up periods and involving husbands can help identify additional aspects of these women's needs.
5.3. Conclusions
The results of this study showed that 8 weeks of counseling based on CBT could significantly improve all components of sexual function. The use of this method is recommended for women who suffer from severe complications after childbirth.