1. Background
Diabetes is one of the most common chronic diseases and a leading cause of death and disability worldwide. Today, diabetes is considered one of the most important health-related and socioeconomic problems globally (1). It is estimated that one person dies because of diabetes or its resulting complications every second; 50% of these mortalities (a total of 4 million people per year) occur in individuals younger than 60 years (2). The global prevalence of diabetes in adults was 6.4% in 2010, which equaled 285 million people, and in 2012, it was estimated to be around 371 million people. By 2030, it is estimated that 552 million people will be affected globally (3). Geographically, this disease has a different distribution worldwide, with the largest prevalence reported in India, China, and the USA (4). According to a global study, the prevalence of diabetes in Iran in 2023 was estimated at around 17.9%. It is estimated that by 2030, nearly 9 million Iranian people will likely have diabetes (5, 6). Managing diabetes to prevent complications is essential (7).
Diabetes can be controlled and managed through various methods, including planning meals and following a proper diet, regular exercise, adhering to the instructions for medications, controlling blood pressure and blood glucose at home, and undergoing tests prescribed by a physician (8). In addition to pharmacotherapy, various non-pharmacological methods have been presented for controlling blood glucose. Many studies have shown the positive effects of various non-pharmacological interventions in controlling diabetes (9, 10). These interventions include adhering to a proper diet, regular exercise, cessation of smoking, taking medications, controlling stress, and adhering to the treatment regimen (11, 12). Some studies have reported the degree of failure to adhere to treatment regimens among diabetics as 23-93%, while other studies have reported it in up to one-third of patients (13, 14). Additionally, the results obtained by Demoz et al. indicated poor treatment adherence in T2DM patients (15).
Reality therapy is a counseling method developed by William Glasser in 1965 based on "choice theory" and is widely established as a therapeutic approach (16). Various studies worldwide suggest the effectiveness of reality therapy in addressing psychological components, issues, and disorders, including adult depression, treatment adherence, and reducing stress and anxiety (17, 18). For instance, the study by Farshchi et al. indicated that reality therapy can reduce anxiety and depression and increase treatment adherence among patients with type I diabetes (19). However, limited studies have examined the effectiveness of reality therapy interventions on health indicators and treatment adherence in patients with T2DM.
2. Objectives
The present study aimed to determine the effect of group reality therapy on treatment adherence and health indicators in patients with T2DM.
3. Methods
3.1. Study Design
This research was a Randomized Controlled Trial (RCT) conducted in a diabetes clinic in Ahvaz, southwest Iran, in 2020. The research population consisted of diabetic patients referred to this center, and the research sample was randomly assigned to intervention and control groups. This study was approved by the Iranian Register of Clinical Trials (IRCT) with the number IRCT20181210041915N2.
3.2. Sampling
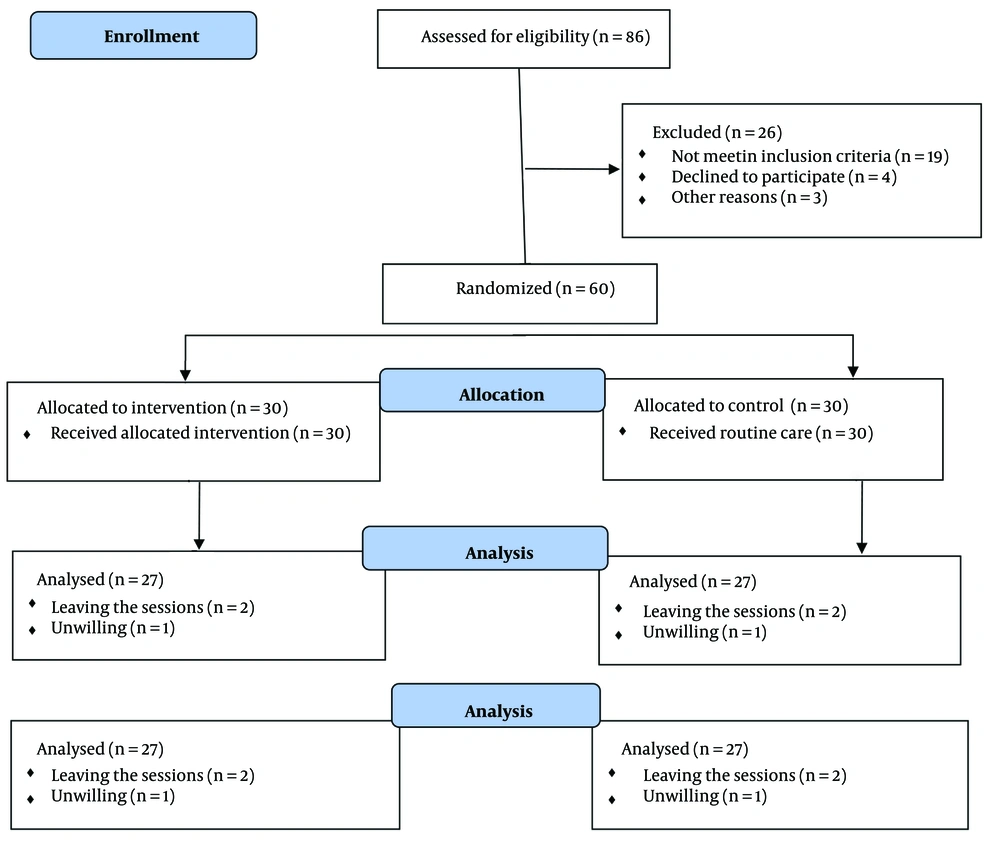
The sample size was calculated as 60 people using a mean comparison formula and based on a similar study (19). Initially, 60 patients referred to Amir Almomenin Hospital in Ahvaz were selected based on inclusion criteria. They were then randomly allocated into two groups of 30 people each (the intervention and the control groups) by a coin toss. In the intervention group, three subjects, and in the control group, three subjects dropped out due to unwillingness to continue with the study. Accordingly, 54 subjects completed the study in the intervention group (n = 27) and in the control group (n = 27) (Figure 1).
The inclusion criteria were literacy in reading and writing, no history of uncontrolled underlying diseases such as epilepsy, no history of receiving any reality therapy training, and non-smoking status. Exclusion criteria included hospitalization during the study, absence from more than one training session, severe psychiatric disorders, or the use of psychotropic drugs or substance abuse.
3.3. Data Collection and Instruments
In this study, data collection instruments included questionnaires and checklists, specifically the questionnaire of demographic-clinical characteristics, compliance to treatment, the checklist of health indicators, and Cohen's stress questionnaire. The demographic questionnaire captured personal characteristics and clinical status of subjects, including age, gender, level of education, marital status, household income, HbA1C, cholesterol, triglyceride levels, and participation in training classes. The compliance to treatment questionnaire included 56 items covering three areas: Diet, exercise, and medications. The total sum of the scores was calculated based on 100 and classified into three groups: Desired (75% - 100%), semi-desired (50% - 75%), and undesired (less than 50%) (19). The reliability and validity of this questionnaire were previously measured by Sanaei et al.; the reliability was estimated at (r = 0.83) using the test-retest method, and content validity was employed for validity (20). Cohen's perceived stress questionnaire consists of 14 items, each responded to on a 5-point Likert scale (none, low, moderate, high, and very high) (21). Reliability was obtained through the Cronbach alpha coefficient, with a score of 0.71 for positive perception of tension and 0.75 for negative perception of tension (22). The checklist of health indicators captured metabolic control indicators (HbA1C, fasting blood glucose, cholesterol, triglyceride). To ensure consistency, the study used laboratory kits from the laboratory at Amiralmomenin Hospital in Ahvaz City for all participants.
3.4. Intervention
After providing a written informed consent form and explaining the research objectives to the participants, they were assured that their information would remain confidential. A sufficient explanation was given to all participants about completing the questionnaires. Before any intervention, laboratory tests were taken for both groups to measure health indicators (blood glucose, cholesterol, triglyceride, HbA1c, etc.). Thereafter, the therapeutic protocol was implemented over ten 45-minute sessions (once per week) for 2 months as lecture and face-to-face training for the intervention group (Table 1). The control group patients received only routine hospital interventions. Educational materials were provided to both groups as pamphlets and CDs after completing the study. After completing the training course, tests were performed and questionnaires were completed by both groups; the final test was conducted one month after the last training session (test and re-completion of questionnaires) by both groups.
| No. | Content | Assignments |
|---|---|---|
| 1 | The initial session introduces members, sets expectations, outlines group rules, ensures regular meetings, performs weekly tasks and presents them in subsequent sessions. | Members are asked to list their three most important health wishes, focusing on how they differ, how they share similar needs, and how they meet them. |
| 2 | The session's assignments were reviewed, and explanations were given on selecting ineffective behaviors like non-compliance with treatment regimens, and the reasons and methods behind such tendencies. | The assignment of this session aims to determine the level of health members desire and their current level of health, based on a continuum from 1 to 100. |
| 3 | Review the assignments of the previous session. Explanation about general behavior and its four components (thought, action, physiology, and feeling), machine learning of behavior in humans, and explanation of aggression as a general behavior | Members should explain the components of non-compliant behaviors. |
| 4 | The session focuses on understanding behavior, self-control, and positive aspects while teaching members about behavior, feelings, and internal and external control. It also emphasizes non-compliance as an internal choice. | The tasks of this session focus on the control of human behavior, examining both external and internal factors, and the actions taken to achieve desired outcomes. |
| 5 | The fifth session emphasized the importance of contrasting qualitative and real-world behavior, emphasizing responsibility, familiarizing members with responsibilities, and promoting responsible behavior choices. | Participants were asked if their goals would lead them to their desired destination and if they had a roadmap to guide them. |
| 6 | The session provided feedback, reviewed assignments, and taught seven destructive and seven effective behaviors to achieve goals, emphasizing the importance of avoiding excuses. | Past failures and excuses highlight unrealistic behaviors and the need for alternative ways to achieve desired outcomes. |
| 7 | Review the assignments of the last session. Determining the ways to achieve the demands from the members' language. Explanation of effective and ineffective solutions considering the two characteristics of being realistic and responsible | Checking whether the specified ways have been effective? |
| 8 | Explanation regarding the components of the therapeutic diet (exercise, medicine, nutrition) and the effect of each one on diabetes control | Members can briefly explain the effects of each component in diabetes control for the next meetings. |
| 9 | The session discussed the importance of a SMART plan to achieve goals, identify member solutions, and introduce program features. | Writing the program in writing with the SMART feature of the program |
| 10 | The tenth session emphasized the importance of commitment, requiring written commitment from members, and personal goals, emphasizing responsibility and goal achievement. |
Contents and Assignments of Reality Therapy Sessions Provided to Participants
3.5. Data Analysis
Data analysis was performed using SPSS 22 and included descriptive statistics such as mean, standard deviation, number, and percentage. The following tests were utilized: Repeated measures tests, independent t-test, Mann-Whitney test, paired t-test, correlation coefficient test, analysis of variance, and Kruskal-Wallis. The significance level was set at P < 0.05.
4. Results
The results showed that both groups were homogeneous in demographic variables, with no significant difference between them in this regard (P > 0.05). To compare the variables of gender, marital status, occupation, household income, and smoking status, the chi-square test was used (Table 2).
| Variables | Intervention (n = 27) | Control (n = 27) | Total (N = 54) | Test Statistic | P-Value |
|---|---|---|---|---|---|
| Age | 51.96 ± 10.56 | 55.30 ± 7.9 | 53.63 ± 9.41 | -1.31 | 0.196 |
| BMI | 27.17 ± 5.63 | 29.16 ± 5.16 | 28.12 ± 5.45 | -1.35 | 0.182 |
| Gender | 1.94 | 0.264 | |||
| Female | 14 (51.9) | 19 (70.4) | 21 (38.9) | ||
| Male | 13 (48.1) | 8 (29.6) | 33 (68.1) | ||
| Marital status | 0.750 | 0.386 | |||
| Single | 4 (14.8) | 2 (7.4) | 6 (11.1) | ||
| Married | 23 (85.2) | 25 (92.8) | 48 (88.9) | ||
| Education | 2.03 | 0.362 | |||
| Primary school | 6 (22.2) | 10 (37.0) | 16 (29.6) | ||
| Middle and high school | 15 (55.6) | 14 (51.9) | 29 (53.7) | ||
| University education | 6 (22.2) | 3 (11.1) | 9 (16.7) | ||
| Source of information | 1.24 | 0.538 | |||
| Treatment staff | 17 (85.5) | 20 (87.0) | 37 (86.0) | ||
| Self-learning | 3 (15.0) | 2 (8.7) | 5 (11.6) | ||
| Media | 0 (0.0) | 1 (4.3) | 1 (2.3) | ||
| Income | 3.97 | 0.137 | |||
| Desirable | 3 (11.1) | 2 (7.4) | 5 (9.3) | ||
| Relatively desirable | 18 (66.7) | 12 (44.4) | 30 (55.6) | ||
| Undesirable | 6 (22.2) | 13 (48.1) | 19 (35.2) | ||
| Smoking | 1.41 | 0.493 | |||
| Yes | 3 (11.1) | 1 (33.7) | 4 (7.4) | ||
| No | 24 (88.9) | 26 (96.3) | 50 (92.6) | ||
| Duration of Diabetes | 0.18 | 0.915 | |||
| Less than 5 | 9 (33.3) | 9 (33.3) | 18 (33.3) | ||
| 5 - 10 | 3 (11.1) | 4 (14.8) | 7 (13.0) | ||
| More than 10 | 15 (55.6) | 14 (51.9) | 29 (53.7) | ||
| Family history of Diabetes | 1.54 | 0.352 | |||
| Yes | 18 (66.7) | 22 (81.5) | 40 (74.1) | ||
| No | 9 (33.3) | 5 (18.5) | 14 (25.9) |
Comparison of Demographic Variables of Diabetic Patients in Intervention and Control Groups Before Reality Therapy Intervention (N = 54)
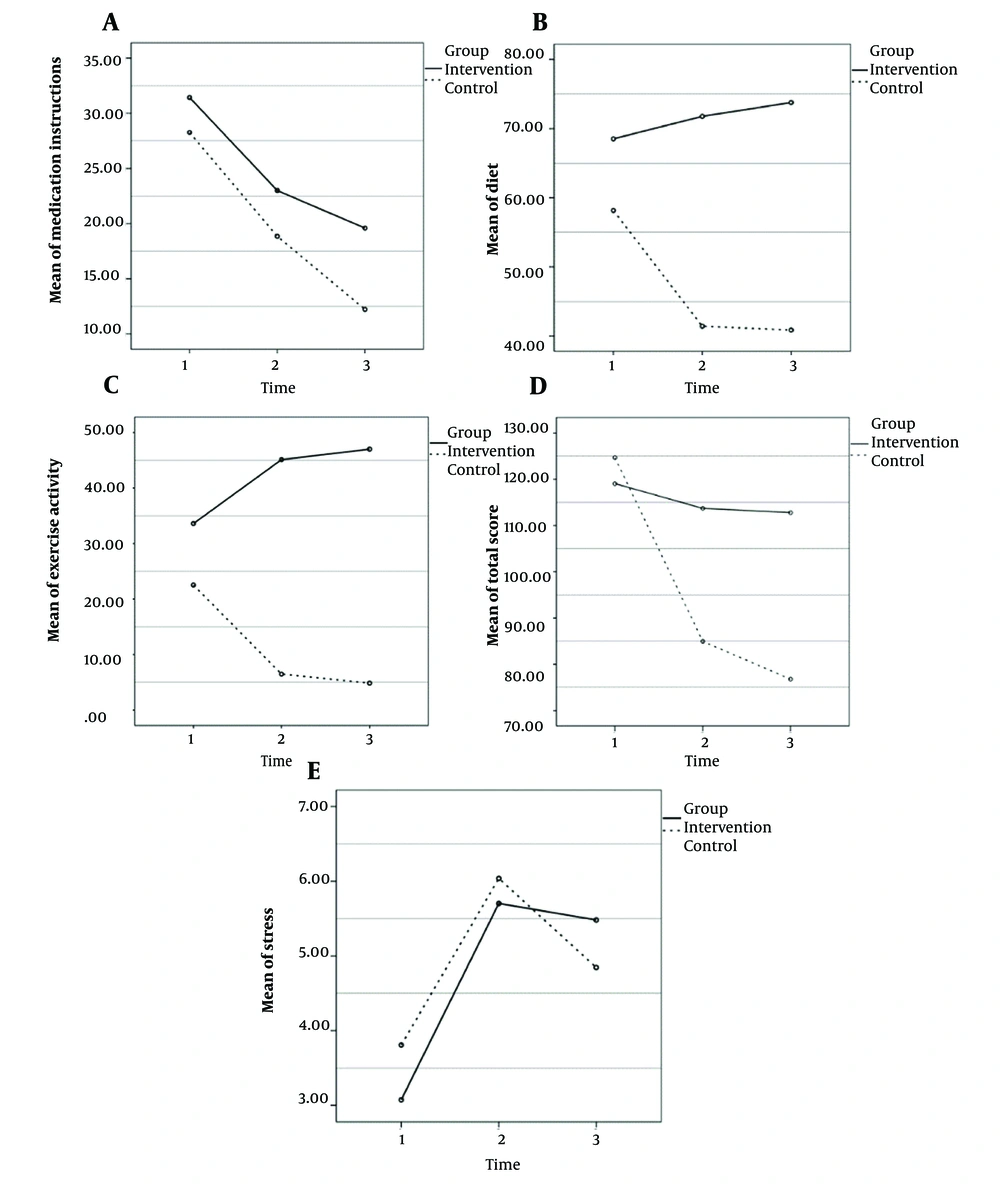
The results also showed that the mean scores for exercises, dietary instructions, and drug instructions had no significant difference between the two groups before the intervention, according to t-test results (P > 0.05). However, immediately after the intervention and one month post-intervention, a significant difference was found between the two groups in terms of exercise and dietary instructions (P < 0.001), while the difference in drug instructions was not significant (P > 0.05) (Table 3).
| Variables | Intervention (n = 27) | Control (n = 27) | Test Statistic | P-Value | Total (N = 54) |
|---|---|---|---|---|---|
| Compliance to treatment regimen | |||||
| Exercise activity | |||||
| Baseline | 33.59 ± 16.74 | 22.52 ± 11.34 | 2.85 | 0.006 | 28.06 ± 15.22 |
| 1.5 months later | 45.11 ± 6.62 | 6.28 ± 8.09 | 19.19 | < 0.001 | 25.79 ± 20.82 |
| 3 months later | 47.00 ± 8.45 | 4.75 ± 7.11 | 19.83 | < 0.001 | 25.92 ± 22.63 |
| Diet | |||||
| Baseline | 68.52 ± 10.34 | 58.15 ± 4.79 | 4.73 | < 0.001 | 63.33 ± 9.54 |
| 1.5 months later | 71.78 ± 4.85 | 41.41 ± 4.02 | 25.03 | < 0.001 | 56.59 ± 15.95 |
| 3 months later | 73.78 ± 6.60 | 40.85 ± 4.69 | 21.13 | < 0.001 | 57.31 ± 17.56 |
| Stress | |||||
| Baseline | 3.07 ± 1.54 | 3.81 ± 1.92 | -1.54 | 0.130 | 3.43 ± 1.76 |
| 1.5 months later | 5.70 ± 3.49 | 6.26 ± 2.84 | -0.64 | 0.524 | 5.98 ± 3.16 |
| 3 months later | 5.48 ± 3.63 | 4.78 ± 2.31 | 0.85 | 0.339 | 5.13 ±3.03 |
| Medication instructions | |||||
| Baseline | 31.43 ± 1354 | 28.26±9.97 | 0.98 | 0.331 | 29.84 ± 11.88 |
| 1.5 months later | 23.00 ± 7.57 | 18.85±6.61 | 2.14 | 0.037 | 20.92 ± 7.35 |
| 3 months later | 19.59 ± 8.11 | 12.22 ± 3.63 | 4.31 | < 0.001 | 15.91 ± 7.25 |
| Total score | |||||
| Baseline | 119.05 ± 26.92 | 124.67 ± 15.64 | -0.94 | 0.353 | 121.86 ± 21.98 |
| 1.5 months later | 113.70 ± 10.96 | 84.96 ± 14.66 | 8.16 | < 0.001 | 99.33 ± 19.36 |
| 3 months later | 112.78 ± 13.64 | 76.78 ± 12.64 | 10.06 | < 0.001 | 94.78 ± 22.35 |
| Health Indicators | |||||
| FBS | |||||
| Baseline | 229.63 ± 118.11 | 193.19 ± 77.58 | 1.34 | 0.186 | 211.41 ± 100.6 |
| 1.5 months later | 123.59 ± 42.04 | 203.7 ± 76.14 | -4.79 | < 0.001 | 163.65 ± 73.11 |
| 3 months later | 123.22 ± 44.20 | 238.26 ± 92.49 | -5.83 | < 0.001 | 180.74±92.33 |
| Triglyceride | |||||
| Baseline | 207.81 ± 74.38 | 175.33 ± 78.47 | 1.56 | 0.125 | 191.57 ± 77.48 |
| 1.5 months later | 162.59 ± 51.58 | 199.0 ± 117.1 | -1.48 | 0.145 | 180.8 ± 91.49 |
| 3 months later | 154.96 ± 50.44 | 244.15 ± 152.6 | -2.88 | 0.006 | 199.56 ± 121.3 |
| Cholesterol | |||||
| Baseline | 176.52 ± 51.54 | 161.04 ± 38.44 | 1.25 | 0.216 | 168.78 ± 45.71 |
| 1.5 months later | 162.56 ± 46.29 | 167.44 ± 38.01 | -0.42 | 0.674 | 165.0 ± 42.06 |
| 3 months later | 146.22 ± 34.69 | 189.70 ± 43.62 | -4.05 | < 0.001 | 167.96 ± 44.78 |
| HBA1C | |||||
| Baseline | 8.15 ± 2.07 | 8.12 ± 1.90 | 0.22 | 0.827 | 8.13 ± 1.97 |
| 3 months later | 6.19 ± 1.87 | 9.03 ± 1.85 | -5.77 | < 0.001 | 7.56 ± 2.33 |
Comparison of Trends in Variables Included: Diet, Treatment Regimen, Exercise, Medication, and Stress at Different Times by Groups (N = 54) a
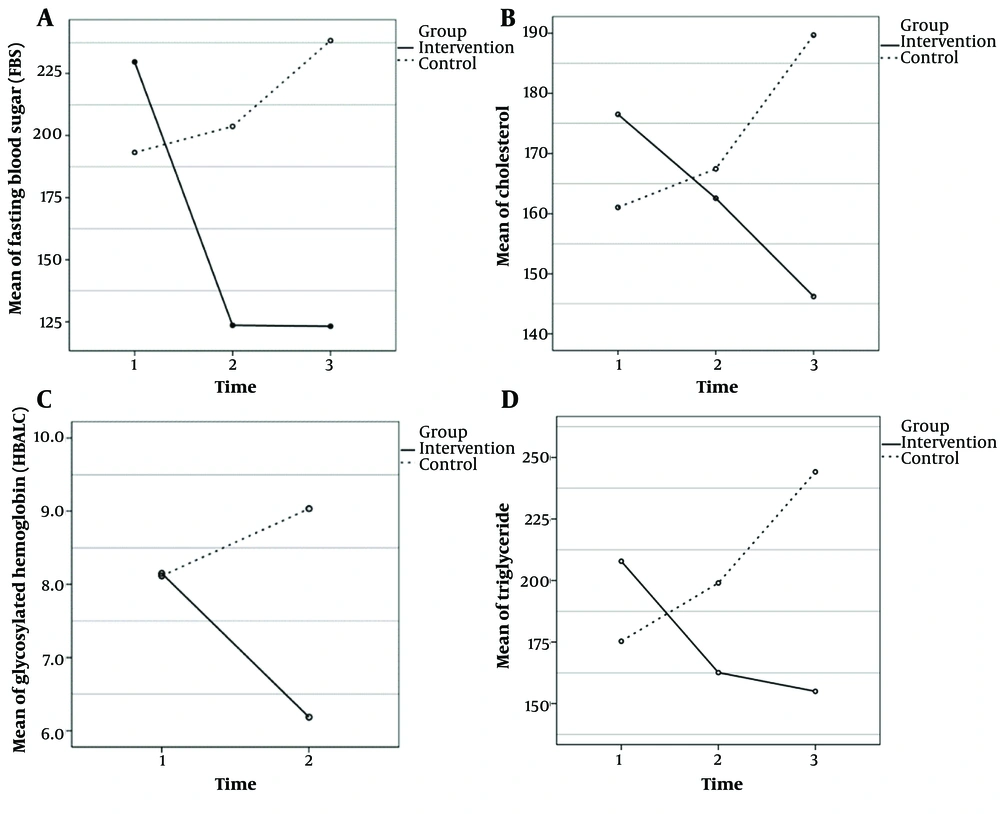
The results also showed that there was no significant difference in the stress scores between the pre-intervention and post-intervention phases, according to repeated measurement tests (P > 0.05). Regarding the analysis of health indicators, the findings indicated that the mean FBS, cholesterol, and triglyceride levels had no significant difference between the two groups before the intervention (P > 0.05). However, immediately after the intervention and one month post-intervention, a significant difference was found between the two groups (P < 0.001). Additionally, the mean HbA1c levels showed no significant difference between the two groups before and after the intervention (P > 0.05) (Table 4, Figures 2 and 3).
| Variables | Mean Square | F | P-Value | ƞ2 |
|---|---|---|---|---|
| Compliance to Treatment Regimen | ||||
| Exercise activity | ||||
| Overall | ||||
| Time | 86.91 | 1.37 | 0.258 | 0.026 |
| Time*group | 3908.89 | 61.69 | < 0.001 | 0.543 |
| Group | 37965.43 | 196.47 | < 0.001 | 0.791 |
| Control | ||||
| Time | 2573.79 | 44.81 | < 0.001 | 0.633 |
| Intervention | ||||
| Time | 1422.01 | 20.53 | < 0.001 | 0.441 |
| Diet | ||||
| Overall | ||||
| Time | 739.64 | 25.72 | < 0.001 | 0.331 |
| Time*group | 2059.39 | 71.62 | < 0.001 | 0.579 |
| Group | 24420.50 | 9415.86 | < 0.001 | 0.887 |
| Control | ||||
| Time | 2608.75 | 160.76 | < 0.001 | 0.861 |
| Intervention | ||||
| Time | 190.27 | 4.61 | < 0.001 | 0.151 |
| Stress | ||||
| Overall | ||||
| Time | 82.78 | 15.74 | < 0.001 | 0.236 |
| Time*group | 6.57 | 1.25 | 0.291 | 0.024 |
| Group | 3700.70 | 0.07 | 0.790 | 0.001 |
| Medication instructions | ||||
| Overall | ||||
| Time | 2691.16 | 53.26 | < 0.001 | 0.506 |
| Time*group | 65.15 | 1.29 | 0.280 | 0.024 |
| Group | 971.23 | 7.45 | 0.009 | 0.125 |
| Total score | ||||
| Overall | ||||
| Time | 11353.04 | 57.91 | < 0.001 | 0.527 |
| Time*group | 6671.67 | 34.03 | < 0.001 | 0.396 |
| Group | 15730.06 | 36.34 | < 0.001 | 0.411 |
| Control | ||||
| Time | 17715.27 | 119.14 | < 0.001 | 0.047 |
| Intervention | ||||
| Time | 309.44 | 1.27 | 0.289 | 0.821 |
| Health Indicators | ||||
| FBS | ||||
| Overall | ||||
| Time | 31621.93 | 21.49 | < 0.001 | 0.292 |
| Time*group | 84941.23 | 57.71 | < 0.001 | 0.526 |
| Group | 113340.89 | 7.05 | 0.010 | 0.119 |
| Control | ||||
| Time | 15013.79 | 32.239 | < 0.001 | 0.554 |
| Intervention | ||||
| Time | 101549.37 | 40.98 | < 0.001 | 0.612 |
| Triglyceride | ||||
| Overall | ||||
| Time | 4785.97 | 2.37 | 0.098 | 0.044 |
| Time*group | 50251.39 | 24.90 | < 0.001 | 0.324 |
| Group | 39013.56 | 1.702 | 0.198 | 0.032 |
| Control | ||||
| Time | 33002.75 | 11.02 | < 0.001 | 0.298 |
| Intervention | ||||
| Time | 22034.61 | 21.18 | < 0.001 | 0.449 |
| Cholesterol | ||||
| Overall | ||||
| Time | 213.43 | 0.621 | 0.539 | 0.012 |
| Time*group | 12107.19 | 35.24 | < 0.001 | 0.404 |
| Group | 4867.56 | 1.03 | 0.315 | 0.019 |
| Control | ||||
| Time | 6112.38 | 22.49 | 0.135 | 0.464 |
| Intervention | ||||
| Time | 6208.24 | 14.95 | < 0.001 | 0.365 |
| HBA1C | ||||
| Overall | ||||
| Time | 8.96 | 20.19 | < 0.001 | 0.280 |
| Time*group | 61.20 | 138.02 | < 0.001 | 0.726 |
| Group | 51.95 | 7.53 | 0.008 | 0.127 |
| Control | ||||
| Time | 11.67 | 82.02 | < 0.001 | 0.759 |
| Intervention | ||||
| Time | 58.49 | 78.55 | < 0.001 | 0.751 |
Comparison of Trends in Health Indicators at Different Times by Groups Using Repeated Measures Test (N = 54)
5. Discussion
This study was conducted to determine the effect of reality therapy on treatment adherence and health indicators in 54 T2DM patients. The results showed that the physical activity dimension score increased significantly in the intervention group compared to the control group after group reality therapy. In other words, participants in the intervention group were more successful in adopting an exercise routine to maintain their health compared to the control group. Confirming these findings, a study by Farshchi et al. indicated that diabetic patients often have an unsuitable lifestyle due to the disease and its complications, with physical activity and proper diet not being common. However, reality therapy, a common psychological treatment, can effectively help in controlling the disease (19).
Furthermore, the present study found that the score for the dietary instructions dimension increased significantly in the intervention group compared to the control group after implementing the intervention. Similarly, Massah et al. showed that an educational program based on reality therapy could improve dietary behaviors in diabetic patients, aligning with the findings of this study (23).
On the other hand, the score for the drug dimension did not differ significantly in the intervention group compared to the control group after implementing the reality therapy intervention. A study by Naderyanfar et al. found that the scores for the drug behavior subscale did not increase significantly in the intervention group, which aligns with the findings of this study (24). However, Farshchi et al. found that group reality therapy was effective in improving adherence to a proper diet, exercise, drug regimen, and blood glucose control (19). Additionally, studies by Matteson and Russell, and Kreps et al. suggested that cognitive-behavioral intervention was more effective than other interventions for drug regimen adherence in patients with chronic diseases (25, 26). The differing results of these studies compared to the present study could be attributed to varying educational conditions and interpersonal differences among patients in learning, which may explain the differences in the drug behavior dimension.
The results also showed that the reality therapy training method is not effective in reducing stress in diabetic patients. In line with this finding, Fuladvandi et al. showed that reality therapy did not significantly reduce the stress levels of diabetic patients, which is similar to the present study's findings (27). Heenan et al. found that factors such as a friendly and respectful atmosphere, free expression of group sympathetic emotions, and sympathetic understanding during group therapy, with an emphasis on self-related concepts, led to a different attitude in patients compared to the beginning of the treatment course. This positive change was attributed to the therapy method, which, by establishing sympathy and deep relations among patients over sessions, allowed for better expression of their problems and increased acceptance of disease symptoms, thereby enhancing the effectiveness of the educational method in diabetic patients (28). This finding, however, does not align with the present study's results, which could be due to the socio-cultural conditions and average age of the patients.
The results of the present study also showed that FBS, triglyceride, and cholesterol levels decreased significantly in the intervention group compared to the control group after the intervention. These findings are in congruence with the findings of Tachanivate et al., Wilson et al., and Velázquez-López et al. (29-31). However, the present study also showed that HbA1c levels did not change significantly in either group before or after the intervention, indicating that reality therapy did not affect HbA1c levels in T2DM patients. In line with this finding, DiClemente showed that after the educational intervention, there was no significant difference in health indicators such as FBS and HDL, which concurs with the present study's findings (32). On the other hand, Ahmadi et al. found that training self-care behaviors by a nurse effectively reduced HbA1c levels in diabetic patients (33). This difference in findings may be attributed to the different training methods used.
It should be noted that the psychological status, as well as familial, personal, and social problems of the participants, may have affected their responses and thus the research findings. These factors were beyond the researcher’s control and could limit the generalizability of these findings.
5.1. Conclusions
The present study found that reality therapy, by changing thought components and patients’ understanding, could lead to improved adherence to treatment regimens regarding diet and physical activity, and improve the health indicators of T2DM patients. Thus, nurses, counselors, therapists, and clinical psychologists can use educational programs based on reality therapy to promote self-care behavior in diabetic patients. Furthermore, training experts in relevant organizations on reality therapy to hold educational workshops can be beneficial for vulnerable groups.