1. Background
Chronic kidney disease involves the bilateral, progressive, chronic deterioration of nephrons and becomes apparent when 50 - 75% of approximately two million nephrons have ceased their physiological function. In such cases, death is inevitable unless renal replacement therapies are undertaken (1, 2). This disease poses a significant health problem due to its substantial financial burden, and the absence of early and appropriate management can lead to end-stage renal disease (3).
The World Health Organization (WHO) identifies chronic kidney disease as a global health issue, estimating that around 850 million people worldwide suffer from various degrees of renal failure. This condition, with an 11% prevalence rate, accounts for approximately 4.5 million deaths annually (4). In Iran, the prevalence and incidence rates of end-stage renal disease (ESRD) are 435.8 and 63.8 per million people, respectively (5). The United States reports the highest prevalence of renal failure, though there has been a decreasing trend, with the number of patients reducing from 125,408 in 2016 to 124,500 in 2017 (6). Conversely, Western Europe, developed countries, and developing nations like Iran have seen an increasing trend in recent decades (7).
In addition to metabolic disorders and an elevated mortality risk from cardiovascular diseases, chronic kidney disease significantly affects patients' physical and mental health, diminishes their quality of life, and places a considerable financial strain on the healthcare system (8).
Patients undergoing hemodialysis face not only the physical and mental challenges associated with the disease but also significant economic pressures (9). The costs of managing this disease were estimated at $4.1 billion in Australia in 2012, $55 billion in the U.S. in 2010, and $1.45 billion in England in 2010 (10).
Early diagnosis and the timely, effective management of chronic kidney disease can significantly reduce its physical and mental impact and markedly decrease its mortality rate (11). Dialysis and kidney transplantation are two renal replacement methods that prevent the accumulation of waste materials in the body. Peritoneal dialysis and hemodialysis represent two forms of dialysis (12), with hemodialysis being the most common method (70%) worldwide for several reasons (13). The annual growth rate of hemodialysis patients is between 10 - 12% globally (14).
Opting for hemodialysis comes with a range of complications during and after the procedure, such as hypotension (20 - 30%), muscle cramps (5 - 20%), nausea and vomiting (5 - 15%), headaches (5%), pruritus (5%), chest and back pain (2 - 5%), and fever and chills (1%) (15). Approximately four million people globally must connect to a dialysis machine 2 - 3 times a week for several hours, significantly impacting their daily lives (16). Despite considerable advancements in medical and nursing care, the mortality rate among hemodialysis patients remains alarmingly high (17, 18). Research indicates that the average life expectancy of patients on dialysis is under three years (19). Survival analysis, a statistical model widely endorsed by many experts, employs a retrospective methodology to monitor a group of subjects over a specific period until an event of interest (e.g., death) occurs. This study concludes by evaluating subjects who did not experience the event as censored data (20). Numerous global studies utilizing this approach have informed various aspects of patient management and treatment. For example, Park et al. reported that the mortality rate for hemodialysis patients after one year of treatment was 20 - 25%, with a five-year survival rate of 35% in the United States (21). In Iran, Habibi et al. estimated the survival rates at 1, 2, 3, 4, and 5 years for these patients to be 84%, 60%, 49%, 25%, and 10%, respectively (15).
Therefore, this study specifically focuses on hemodialysis, a prevalent renal replacement therapy for ESRD. Hemodialysis is vital for managing chronic kidney disease (CKD), especially in light of its increasing prevalence and the high mortality rates associated with it. The therapy necessitates significant lifestyle adjustments and is fraught with various complications, highlighting the need to comprehend its long-term outcomes. Despite advances in healthcare, the survival rates of patients undergoing hemodialysis present a significant concern, with many patients experiencing a shortened life expectancy.
2. Objectives
Given these challenges, this research seeks to offer detailed insights into the survival rates and determinants of mortality among hemodialysis patients in Qazvin Province, Iran. This is crucial for enhancing patient management and treatment strategies, tailoring them to meet the specific needs of the Iranian populace, and enriching the global understanding of CKD and ESRD management.
3. Methods
3.1. Study Design and Participants
This historical cohort study involved 378 hemodialysis patients from seven hospitals in Qazvin province, including Bu Ali Sina, Velayat, Razi, Alvand, Valiasr, Bueen Zahra, and Avaj. The sample size was estimated using the formula related to the Cox proportional hazards regression model, with considerations for α = 0.05 and 1 - β = 0.80:
This calculation was based on the variable of serum albumin, identified as an important and significant variable in previous studies (15, 22), with a standard deviation of 0.82 and an HR = 0.55 for the 173 samples that resulted in death. Accounting for approximately 45% death during the follow-up period, at least 375 samples of hemodialysis patients were needed.
The study spanned from March 21, 2015, to March 20, 2020, and analyzed data extracted from the medical records of these patients, offering a detailed overview of their medical history and treatment during this timeframe. All patients who met the inclusion and exclusion criteria during the specified period were included in the study through the census method. The eligibility criteria were as follows:
- Willingness to participate: Participants must voluntarily agree to take part in the study, emphasizing the significance of consent given the study's focus on survival rates among hemodialysis patients.
- Minimum dialysis duration: Only individuals who had undergone dialysis for at least three months were considered to ensure the sample represented those actively managing end-stage renal disease.
- Age requirement: Participants needed to be 18 years or older, which corresponds with the study's aim to assess adult hemodialysis outcomes within the Iranian setting.
The exclusion criteria were as follows:
- Refusal to continue participation: Participants unwilling to continue in the study were excluded to maintain accurate survival rate analysis through consistent participation.
- Loss to follow-up: Participants who were untraceable or whose data could not be reliably followed through the study duration were excluded, safeguarding data integrity.
- Incomplete hospital records: Due to the reliance on medical history to understand dialysis and health outcomes, participants with incomplete medical records were excluded.
- History of kidney transplantation: To keep the study focused on hemodialysis survival rates, those with a history of kidney transplantation were not included, considering their distinct health profiles.
These criteria were critical for assembling a focused and relevant group of participants to study hemodialysis survival rates within the Iranian population, particularly in Qazvin Province. The objective was to deliver comprehensive insights into the factors that influence survival rates among this specific patient demographic. Data collection involves using a checklist to gather information from patient's medical records or through telephone or face-to-face meetings. The variables evaluated in this study included age, sex, educational level, occupation, marital status, frequency of dialysis per week, type of vascular access, blood urea nitrogen (BUN) level, hemoglobin level, serum albumin, serum calcium, and the adequacy of dialysis.
The follow-up period in this study commenced three months after the initiation of the first dialysis session, with the endpoint being the time of death. Censored subjects at the study's conclusion included those still alive, those who died from causes unrelated to their condition, and participants lost to follow-up.
Bias was minimized through stringent inclusion and exclusion criteria, the use of the census method for thorough patient inclusion, and standardized data collection from medical records. Conducted over five years, the study aimed to ensure a representative sample and reliable data collection across multiple hospital settings, thus enhancing the validity of the findings.
3.2. Statistical Analysis
Qualitative variables were presented as numbers and percentages, while quantitative variables were reported using means and standard deviations. The Kaplan-Meier curve was utilized to assess the survival rate of hemodialysis patients, and Cox regression analysis was employed to estimate the hazard ratios of factors affecting survival. To adjust for confounders, variables with P-values ≤ 0.2 in univariable Cox regression analyses were included in the multivariable Cox regression model. The proportional hazards assumption was tested and confirmed using the estate test method. Data analysis was performed using SPSS software version 25 and STATA version 12, with a significance level set at 0.05.
3.3. Ethical Considerations
This study received approval from the ethics committee of Qazvin University of Medical Sciences (Ethical Code: IR.QUMS.REC.1400.017. Before providing informed consent, all participants were thoroughly informed about the study's objectives and methods. It was clearly communicated that they had the option to withdraw from the study at any time.
4. Results
The average age of the participants was 61.65 years. The majority of the patients were male (58.2%), married (86%), and illiterate (39.9%), with all of them having underlying diseases. Most participants (90.21%) underwent hemodialysis three times a week and utilized dialysis fistulas (66.9%) for vascular access. Other qualitative and clinical characteristics are detailed in Table 1.
| Variables and categories | Total | Censored | Deceased | P-Value b |
|---|---|---|---|---|
| Sex | 0.258 | |||
| Male | 220 (58.2) | 138 (62.7) | 82 (37.3) | |
| Female | 158 (41.8) | 90 (57.0) | 68 (43.0) | |
| Marital status | 0.256 | |||
| Single | 36 (9.5) | 22 (61.1) | 14 (38.9) | |
| Married | 325 (86.0) | 199 (61.2) | 126 (38.8) | |
| Divorced/ Widowed | 17 (4.5) | 7 (41.2) | 10 (58.8) | |
| Education level | < 0.001 | |||
| Illiterate | 151 (39.9) | 84 (55.6) | 67 (44.4) | |
| Primary education | 76 (20.1) | 31 (40.8) | 45 (59.2) | |
| High school education | 87 (23.0) | 63 (72.4) | 24 (27.6) | |
| Academic education | 64 (16.9) | 50 (78.1) | 14 (21.9) | |
| Occupation | 0.165 | |||
| Jobless | 190 (50.3) | 82 (43.2) | 0.165 | |
| Employed | 188 (49.7) | 120 (63.8) | 68 (36.2) | |
| Frequency of dialysis per week | 0.687 | |||
| Once a or Twice | 35 (9.3) | 20 (57.1) | 15 (42.9) | |
| Three or Four times | 343 (90.7) | 208 (60.6) | 135 (39.4) | |
| Vascular access | < 0.001 | |||
| Shaldon | 73 (19.3) | 13 (17.8) | 60 (82.2) | |
| Fistula | 253 (66.9) | 171 (67.6) | 82 (32.4) | |
| Permcath | 48 (12.7) | 41 (85.4) | 7 (14.6) | |
| Graft | 4 (1.1) | 3 (75.0) | 1 (25.0) | |
| Hb, g/dL | < 0.001 | |||
| < 10 | 138 (36.5) | 61 (42.2) | 77 (55.8) | |
| 10 - 12 | 144 (38.1) | 98 (68.1) | 46 (31.9) | |
| > 12 | 96 (25.4) | 69 (71.9) | 27 (28.1) | |
| Calcium, mg/dL | 0.002 | |||
| < 8.4 | 154 (40.7) | 97 (63.0) | 57 (37.0) | |
| 8.4 - 9.5 | 188 (49.7) | 119 (63.3) | 69 (36.7) | |
| > 9.5 | 36 (9.5) | 12 (33.3) | 24 (66.7) | - |
| Total | 378 (100) | 228 (60.3) | 150 (39.7) | |
| Age, y | 61.65 ± 14.94 | 59.57 ± 14.11 | 64.81 ± 15.63 | 0.001 |
| Adequacy of dialysis | 1.22 ± 0.30 | 1.25 ± 0.34 | 1.16 ± 0.23 | 0.002 |
| Albumin, g/dL | 4.09 ± 0.73 | 4.09 ± 0.57 | 4.08 ± 0.92 | 0.895 |
| BUN, mg/dL | 26.54 ± 16.54 | 22.81 ± 12.69 | 32.20 ± 19.83 | < 0.001 |
a Values are expressed as mean ± SD or No. (%).
b Chi-square test for qualitative variables and independent t-test for quantitative variables.
4.1. Survival Rate
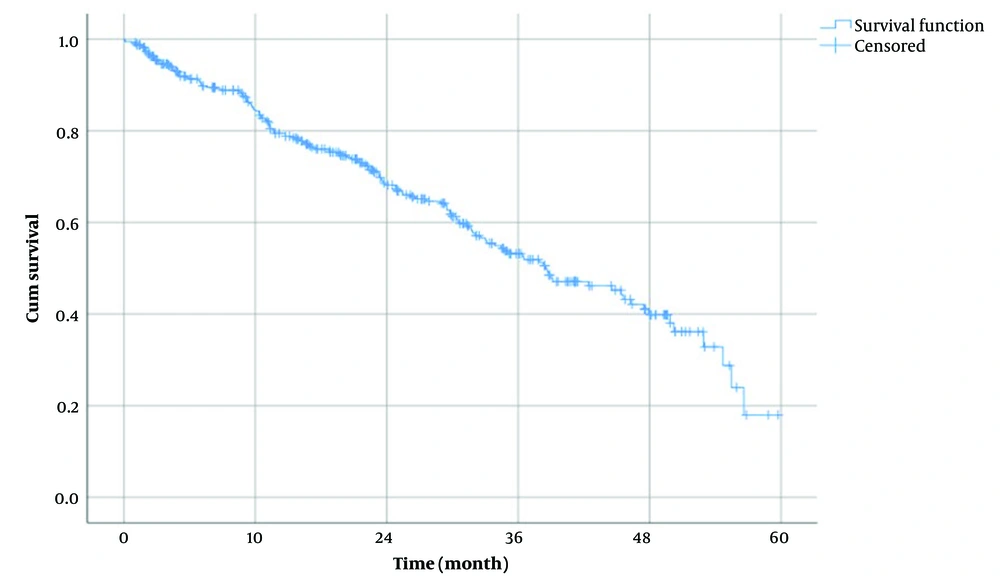
The average follow-up duration was 22.82 ± 16.65 months. Out of 378 patients, 150 patients (39.7%) experienced the event (death). The median survival time for the patients was 38.5 months (95% CI: 31.35 - 45.65 months), indicating that half of the patients survived for at least 38.5 months. According to the Kaplan-Meier method, the 1, 2, 3, 4, and 5-year cumulative survival probabilities for the hemodialysis patients, along with their standard errors, were 84.3 ± 2.0%, 68.1 ± 2.7%, 53.2 ± 3.2%, 39.8 ± 3.9%, and 18.0 ± 7.1%, respectively (Figure 1).
4.2. Univariable Cox Regression Analysis
Cox regression analysis was utilized to explore the association between various variables and the mortality of hemodialysis patients (Table 2). The analysis revealed that for each one-year increase in age and each one-mg/dL increase in BUN, there was a significant 2% increase in mortality risk. Conversely, mortality significantly decreased with higher levels of education, an increased number of dialysis sessions per week, and greater adequacy of dialysis. Regarding vascular access, mortality was significantly lower in patients with fistulas and Permicath compared to those with Shaldon catheters. A decrease in hemoglobin levels and an increase in calcium levels, compared to their normal ranges, were also significantly associated with increased mortality (P < 0.05).
| Variables | Median of Survival, mo | Hazard Ratio (HR) | 95% Confidence Interval for HR | P-Value | |
|---|---|---|---|---|---|
| Lower Bound | Upper Bound | ||||
| Gender | 0.350 | ||||
| Male | 38.77 | Ref | - | - | |
| Female | 38.50 | 1.17 | 0.85 | 1.61 | |
| Marital status | |||||
| Single | 44.53 | Ref | - | - | |
| Married | 38.50 | 1.21 | 0.70 | 2.11 | 0.49 |
| Widow or divorced | 21.50 | 2.08 | 0.92 | 4.69 | 0.08 |
| Educational status | |||||
| Illiterate | 29.50 | Ref | - | - | |
| Elementary | 29.97 | 1.15 | 0.79 | 1.68 | 0.476 |
| High school education | 52.93 | 0.38 | .23 | 0.60 | < 0.001 |
| High school diploma or academic education | 55.47 | 0.33 | 0.19 | 0.59 | < 0.001 |
| Occupational status | 0.283 | ||||
| Unemployed | 37.97 | Ref | - | - | |
| Employed | 39.03 | 0.84 | 0.61 | 1.16 | |
| Dialysis per week | 0.002 | ||||
| 1 or 2 times | 23.47 | Ref | - | - | |
| 3 or 4 times | 38.77 | 0.42 | 0.24 | 0.72 | |
| Vascular access | |||||
| Shaldon | 10.93 | Ref | - | - | |
| Fistula | 46.27 | 0.17 | 0.12 | 0.23 | < 0.001 |
| Permcath | . | 0.09 | 0.04 | 0.20 | < 0.001 |
| Hb, g/dL | |||||
| < 10 | 29.50 | 2.24 | 1.56 | 3.24 | < 0.001 |
| 10 - 12 | 47.87 | Ref | - | - | |
| > 12 l | 52.93 | 0.85 | 0.53 | 1.37 | 0.501 |
| Calcium, mg/dL | |||||
| < 8.4 | 44.53 | 1.01 | 0.71 | 1.43 | 0.970 |
| 8.4 - 9.5 | 45.60 | Ref | - | - | |
| > 9.5 | 23.67 | 2.25 | 1.41 | 3.59 | 0.001 |
| Age, y | - | 1.02 | 1.01 | 1.03 | 0.001 |
| Adequacy of dialysis | - | 0.50 | 0.27 | 0.91 | 0.023 |
| Albumin, g/dL | - | 0.92 | 0.74 | 1.14 | 0.443 |
| BUN, mg/dL | - | 1.02 | 1.01 | 1.03 | < 0.001 |
4.3. Multivariable Cox Regression Analysis
Multivariable Cox regression analysis was utilized to identify variables associated with the mortality of hemodialysis patients, adjusted for confounding factors. Variables with P-values ≤ 0.2 in univariable Cox regression were included in the multivariable Cox regression model. The analysis revealed that age, BUN levels, education level, frequency of dialysis per week, type of vascular access, average hemoglobin, and average calcium levels were significant predictors of mortality in hemodialysis patients (Table 3). Mortality risk significantly increased by 2% with each one-year increase in age (HR = 1.02, 95% CI: 1.001 to 1.03) and by 1% with each one-mg/dL increase in BUN levels (HR = 1.01, 95% CI: 1.004 to 1.02). Patients undergoing dialysis 3 - 4 times a week experienced a significant 54% reduction in mortality compared to those dialyzing 1 - 2 times a week (HR = 0.46, 95% CI: 0.25 to 0.82). Regarding vascular access, mortality was significantly lower with a fistula compared to a Shaldon catheter (HR = 0.20, 95% CI: 0.13 to 0.28) and a Permcath (HR = 0.13, 95% CI: 0.06 to 0.31). Mortality significantly increased when hemoglobin levels fell below 10 g/dL (HR = 1.77, 95% CI: 1.18 to 2.64) and calcium levels rose above 9.5 mg/dL (HR = 1.86, 95% CI: 1.13 to 3.04) compared to their normal ranges. Additionally, hemodialysis patients with higher education levels experienced significantly lower mortality (HR = 0.58, 95% CI: 0.34 to 0.99).
| Variables | Hazard Ratio (HR) | 95% Confidence Interval for HR | P-Value | |
|---|---|---|---|---|
| Lower Bound | Upper Bound | |||
| Marital status | ||||
| Single | Ref | - | - | |
| Married | 0.55 | 0.30 | 1.03 | 0.060 |
| Widow or divorced | 0.68 | 0.26 | 1.77 | 0.431 |
| Educational status | ||||
| Illiterate | Ref | - | - | |
| Elementary | 1.07 | 0.70 | 1.62 | 0.766 |
| High School | 0.58 | 0.34 | 0.99 | 0.045 |
| High school diploma or academic education | 0.55 | 0.29 | 1.05 | 0.071 |
| Dialysis per week | 0.008 | |||
| 1 or 2 times | Ref | - | - | |
| 3 or 4 times | 0.46 | 0.25 | 0.82 | |
| Vascular access | ||||
| Shaldon | Ref | - | - | |
| Fistula | 0.20 | 0.13 | 0.28 | < 0.001 |
| Permcath | 0.13 | .06 | 0.31 | < 0.001 |
| Hb, g/dL | ||||
| < 10 | 1.77 | 1.18 | 2.64 | 0.006 |
| 10 - 12 | Ref | - | - | |
| > 12 | 1.04 | 0.64 | 1.69 | 0.881 |
| Calcium, mg/dL | ||||
| < 8.4 | 0.96 | 0.66 | 1.38 | 0.819 |
| 8.4 - 9.5 | Ref | - | - | |
| > 9.5 | 1.86 | 1.13 | 3.04 | 0.014 |
| Age, y | 1.02 | 1.001 | 1.03 | 0.031 |
| Adequacy of dialysis | 0.82 | 0.38 | 1.74 | 0.598 |
| BUN, mg/dL | 1.01 | 1.004 | 1.02 | 0.006 |
5. Discussion
This study aimed to determine the 1, 2, 3, 4, and 5-year survival rates of hemodialysis patients and their predictors among 378 patients undergoing hemodialysis in various dialysis departments within Qazvin Province, Iran. Cox regression analysis was utilized to identify mortality predictors in hemodialysis patients. The findings revealed that age, education level, type of vascular access, frequency of dialysis per week, BUN, hemoglobin level, and serum calcium were significant predictors of mortality among patients attending the dialysis wards in Qazvin Province. Previous research has emphasized the importance of estimating the survival rates of hemodialysis patients for decision-making regarding hemodialysis initiation and identifying patients at a high risk of mortality for appropriate management and follow-up (23, 24). The median 5-year survival time for patients was 38.5 months, suggesting that at least 50% of the patients survived for 38.5 months following the commencement of hemodialysis. Habibi et al. reported a median 5-year survival of 34 months, Montaseri et al. reported 37 months, and Ebrahimi et al. reported 20.9 months (15, 22, 25). In contrast, Shabankhani et al. found a median survival rate of 108 months, and Ferreira et al. reported 59 months for Brazilian hemodialysis patients (26, 27). The significant variation in median survival rates across these studies may be attributed to differences in countries' development levels, healthcare access, genetics, lifestyle, and nutrition, as detailed in the study by Kazeminia et al. (28).
In the present historical study, the 1, 2, 3, 4, and 5-year cumulative survival rate of the hemodialysis patients and their standard errors were 84.3 ± 0.020%, 68.1 ± 0.027%, 53.2 ± 0.032%, 39.8 ± 0.039%, and 18.0 ± 0.071%, respectively. The 1, 2, 3, 4, and 5-year survival rates of the patients was 84%, 60%, 49%, 25%, and 10% in a study by Habibi et al (15). These rates were 75%, 63%, 50%, 41%, and 23% in a study by Montaseri et al. respectively, indicating different values with a similar decreasing trend (25). Ferreira et al. reported 1, 5, 10, and 20-year survival rates for Brazilian hemodialysis patients as 82.3%, 49.1%, 22.5%, and 13.3%, respectively (27). Msaad noted 1 and 3-year survival rates of 95% and 87%, and Sun et al. reported 1 and 5-year survival rates of 94% and 59%, respectively (19, 29).
Comparison of the 1, 3, and 5-year survival rates among the aforementioned studies reveals similar 1-year survival rates for patients both within and outside of Iran. However, the 3-year and 5-year survival rates are notably lower for Iranian patients, necessitating further investigation into the influence of various individual and societal factors, as well as the quality of care.
Regarding the relationship between different variables and the mortality of hemodialysis patients, this study found that each one-year increase in age and each one-mg/dL increase in BUN significantly raised mortality by 2%. Msaad et al. identified age as an important predictor of survival for hemodialysis patients, with those above 65 years experiencing a 1.26 times higher risk of mortality compared to those under 65 years (19). Similarly, Montaseri et al. reported that each additional year of age increased the risk of death by 1.88 times in hemodialysis patients (25). In line with this, Bal et al. (30) and Ferreira et al. (27) also highlighted age as a crucial predictor of survival, noting that older patients with higher BUN levels had a lower chance of survival. These findings align with the current study, suggesting that older age and higher BUN levels decrease the survival rate of hemodialysis patients (19, 30), potentially due to the better physical condition and lesser progression of the underlying disease in younger patients, as well as lower BUN levels.
This study also found a significant decrease in mortality with an increase in education level, frequency of dialysis per week, and adequacy of dialysis. Shabankhani et al. (26) discovered that patients with higher education levels had a 36% lower risk of mortality compared to those with lower education levels. A study examining the relationship between dialysis adequacy and mortality in 18 242 hemodialysis patients by Hong and Lee (31) showed that patients with dialysis adequacy below 1.2 faced a much higher mortality risk than those with dialysis adequacy between 1.2 and 1.4. Similarly, Hekmat et al. (32) found dialysis adequacy to be a significant determinant of survival rate in hemodialysis patients, with an OR = 1.193.
In this research, the survival rates for patients with fistulas and Shaldons were 46.27 and 10.93 months, respectively. This contrasts with a study by Torreggiani et al. (33), which found survival rates for patients with fistulas and Shaldons to be 31 ± 26 and 14.5 ± 14 months, respectively, and a study by Kim et al. (34), which reported 5-year survival rates for patients with fistulas and Shaldons as 27% and 12%, respectively.
According to Torreggiani et al., patients with fistulas have a survival chance that is twice as high compared to those without (33, 34). Similarly, do Sameiro-Faria et al. (35) noted that the risk of mortality was higher in patients using a Shaldon catheter as their vascular access compared to other methods, with a hazard ratio (HR) of 3.03 (95%CI = 1.49 - 6.13) (35). In the current study, the hazard ratio for patients with a fistula was estimated at 0.17, whereas Ko et al. reported a hazard ratio of 1.13. This indicates a significantly high survival rate for patients with fistulas (36). These studies suggest that patients with fistulas are typically younger and have fewer comorbidities, indicating their better physical condition. Often, in older patients with a lower life expectancy, physicians may delay placing a fistula, opting instead for alternative access methods at the initiation of dialysis. Furthermore, vascular catheters are associated with a higher risk of infection and longer hospital stays compared to fistulas, contributing to the superior survival rates of patients with fistulas over other vascular access methods (29, 33, 37).
Hemoglobin level was identified as an important mortality predictor in hemodialysis patients. A reduction in hemoglobin levels below 10 g/dL and an increase in calcium levels above 9.5 mg/dL significantly elevated mortality risks compared to their normal ranges. Ferreira et al. (27) also found that ferritin levels below the normal range and calcium levels above 11.01 mg/dL significantly increased mortality risks (HR = 4.102, 95%CI: 1.35 - 12.46).
This study investigated the survival rate and predictors of hemodialysis patients over 1 - 5 years, identifying variables such as age, education, and type of vascular access as significant factors. While its findings align with some international studies, observed variations in survival rates point to regional disparities and nuances in healthcare practices. Fistulas are shown to enhance patient survival, emphasizing the critical role of access type. Nonetheless, the presence of incomplete records and potential confounders necessitates a cautious interpretation of the results and calls for further comprehensive research. Such studies are essential for a broader validation and understanding of hemodialysis outcomes.
5.1. Limitations of the Study and Efforts Made to Address Them
(1) Incomplete records: Rigorous data verification methods were implemented to mitigate the impact of incomplete records.
(2) Regional specificity: By including multiple hospitals across Qazvin province, the study aimed to diversify the patient population, reducing regional bias. However, it's recognized that this does not fully represent global demographics.
(3) Confounding factors: Advanced statistical models, such as Cox regression analysis, were employed to adjust for known confounders, minimizing their impact on the findings.
(4) Scope and sample size: Despite being limited to 378 patients, the study used a census method for inclusion to ensure comprehensive coverage of all eligible patients during the study period, enhancing the representativeness of the sample.
(5) Need for further research: Recognizing the necessity for more extensive research, this study establishes a detailed analytical framework, laying the groundwork for future studies to expand upon these findings in various or larger populations.
5.2. Conclusions
The median survival rate of hemodialysis patients in Qazvin Province, Iran, was 38.5 months (95% CI: 31.35 - 45.65 months), indicating that half of the patients survived for at least 38.5 months post-initiation of hemodialysis. The 1, 2, 3, 4, and 5-year cumulative survival rates of the hemodialysis patients, along with their standard errors, were 84.3 ± 2.0%, 68.1 ± 2.7%, 53.2 ± 3.2%, 39.8 ± 3.9%, and 18.0 ± 7.1%, respectively. Regarding the relationship between mortality and various variables, mortality increased significantly by 2% with each one-year increase in age and by 1% with each one-mg/dL increase in BUN levels. Mortality significantly rose with decreases in hemoglobin levels below 10 g/dL and increases in calcium levels above 9.5 mg/dL. Mortality decreased by 54% in patients undergoing dialysis 3 - 4 times a week compared to those dialyzing 1 - 2 times a week. Regarding the type of vascular access, mortality was significantly lower with a fistula compared to Shaldon and Permcath. Additionally, patients with higher education levels and greater adequacy of dialysis experienced significantly lower mortality rates.
In summary, while the findings offer valuable insights for healthcare professionals in Qazvin Province, their applicability in other regions or countries might require further validation or adaptation due to differences in demographics, healthcare systems, and cultural aspects. These factors should be considered before directly implementing the study's recommendations elsewhere.