1. Background
The global prevalence of diabetes, one of the major health crises of the last century, has increased alarmingly from 1980 to 2014. It is estimated that by 2035, 592 million people worldwide, primarily in developing countries and among low-income populations, will be affected by this disease (1). According to estimates by the World Health Organization, this number will reach six million people in Iran by 2030 (2).
Despite the importance of adhering to care instructions, many studies have shown that diabetic patients often do not fully follow treatment guidelines (diet, blood sugar monitoring, and exercise). Reports indicate adherence rates ranging from 23% to 50% (3).
The problems caused by diabetes significantly impact individuals, families, and society at large, imposing considerable costs (4). Consequently, the challenge of the 21st century has become the effective implementation of self-care behaviors for chronic diseases such as diabetes (5). Educational planning to empower patients to manage their disease is a crucial aspect of treatment, shifting focus from mere obedience to medical advice. In this context, the role and involvement of family members, especially spouses of diabetic patients, are crucial and undeniable (5). Spouses are considered the primary source of support for patients, helping them feel accompanied through the difficulties of the disease and providing the motivation needed to continue treatment. Unfortunately, in our country, the role of this vital support system has not received sufficient attention (6).
Illness perception, which encompasses a person’s understanding of their disease, includes five main areas. The decisions patients make when assessing their symptoms are influenced by their cognitive and emotional perceptions of the disease (7). Studies have found a significant relationship between individuals' beliefs and attitudes about their illness and their cooperation with treatment, which in turn affects disease outcomes (8).
Another focus of this study is on examining the perceived stress levels in patients. High stress levels and inadequate coping mechanisms can lead to feelings of defeat and result in undesirable self-care behaviors. Research indicates that diabetic patients often struggle with emotional regulation and employ inconsistent stress response strategies, which can lead to complications and increased hospitalization rates (9, 10).
Self-care activities for diabetic patients include following a healthy diet, taking medications regularly, exercising, and monitoring blood sugar levels (11). Education plays a vital role in helping patients adhere to these self-care principles. Addressing the educational needs of both the patient and their family, considering the changes imposed by this chronic disease, is a key aspect of care and requires ongoing and dynamic education
In this research, we implemented an empowerment training program for couples, aimed at increasing patients' capacity to navigate the challenging treatment process. Given the strong relationships between spouses, especially in Iranian families, and their mutual influence, the program assessed and enhanced the awareness of both the patient and their family, equipping them with the necessary information to actively participate in managing this chronic condition (6). Unfortunately, in our country, insufficient attention has been given to the critical role of the spouse in managing chronic diseases like diabetes.
2. Objectives
Considering the increasing prevalence of diabetes and the scarcity of studies on family-centered empowerment training focusing on spouses, this research was conducted to empower family-oriented spouses in understanding the disease, managing perceived stress, and improving self-care behaviors of diabetic patients.
3. Methods
This research is a semi-experimental study with two groups conducted from September to February 2021 in Shahrekord. The study was approved by the Ethical Committee of Shahrekord University of Medical Sciences (code: IR.SKUMS.REC.1400.127). The participants included 72 spouses of diabetic patients referred to Imam Ali Clinic in Shahrekord. The criteria for inclusion were: (1) a definite diagnosis of type 2 diabetes, (2) age greater than 20 years, (3) physical and mental ability to participate in the sessions, (4) literacy of the patient’s spouse, (5) no stressful events experienced in the last 6 months by either the patient or the spouse, (6) the patient must be under the direct care of the spouse at home, and (7) all patients should be under oral antidiabetic or insulin therapy. The samples were selected based on convenience sampling. An equal number of red and blue cards were placed in a pot; those who drew a red card were assigned to the intervention group, and those who drew a blue card were assigned to the control group. This randomization applied only to the patients. Data were collected using questionnaires on demographic characteristics, the summary of the Diabetes Self-care Behavior Scale by Toobert et al., the Illness Perception Questionnaire (IPQ) by Weinman et al., and Cohen’s Perceived Stress Questionnaire (13). The Illness Perception Questionnaire includes 9 questions designed to evaluate the emotional and cognitive visualization of the disease. The score range for the first 8 questions is from 1 to 10, while Question 9 is open-ended and asks for the three main causes of diabetes in order (14). The Perceived Stress Questionnaire, designed by Cohen et al., consists of 10 items scored on a five-point Likert scale ranging from zero (never) to four (very much). Items 7, 5, 4, and 8 are scored in reverse. The overall score is obtained by summing the item scores, with a higher score indicating greater perceived stress (15). The Diabetes Self-care Questionnaire includes 15 questions that assess self-care activities over the past week. In the scoring method, except for smoking behavior, which is scored from zero to one, each behavior is rated from zero to seven on an 8-point Likert scale. The total score is obtained by summing the individual scores, with the overall scale score ranging from 0 to 99 (16).
3.1. Intervention Procedure
The sessions were conducted in small groups using a combination of questions and answers, slide shows, movies, discussions, and exchanges of opinions between the researcher, the patient, and the patient's spouse.
The first to third sessions focused on the perceived threat step of the family-centered empowerment model. These sessions covered the nature of the disease, prognosis, symptoms, complications, and the risks of not following necessary prevention measures. They also included methods for preventing and controlling diabetes, and self-care behaviors relevant to the needs of the patient and his spouse, as outlined in the self-care questionnaire. The content was presented using slides and relevant images.
In the fourth to sixth sessions, the discussion centered on recognizing the problem, finding solutions, and addressing how the patient faced issues related to the disease. This included diagnosing the problem (the disease process, contributing factors, complications, risks, and the stress experienced by the patient and family), analyzing the problem, setting goals, presenting solutions, choosing the best solution, and discussing how to implement it based on available resources. Evaluation of the process was conducted throughout the intervention and in all sessions, allowing patients and their spouses to apply what they had learned.
The impact of the empowerment stages and the effectiveness of the learning were assessed. During the research, the researcher-maintained contact with the participants through phone calls to address any questions or issues. Evaluation occurred in two stages: Immediately after the intervention and three months later. At each stage, the questionnaires were completed again by both groups. The control group received routine care during the intervention, and the researcher also contacted them by phone. Data were analyzed using SPSS software version 21 (SPSS Inc., Chicago, IL, USA), employing descriptive statistics (mean, standard deviation, frequency, and percentage) and analytical tests (t-test, Mann–Whitney test, chi-squared test, repeated measures analysis, and Friedman test).
4. Results
Demographic characteristics are provided in Table 1. The mean age of patients in the intervention group was 50.5 ± 9.9 years, while in the control group, it was 46.6 ± 10.6 years. According to the independent t-test, there was no significant difference between the intervention and control groups (P = 0.45).
| Variables | Intervention | Control | P-Value |
|---|---|---|---|
| Gender | 0.48 | ||
| Male | 18 (50) | 21 (58.3) | |
| Female | 18 (50) | 15 (41.7) | |
| Total | 36 (100) | 36 (100) | |
| Education | 0.75 | ||
| Illiterate | 8 (22.2) | 2 (5.6) | |
| Primary | 14 (38.9) | 10 (27.8) | |
| Diploma | 9 (25) | 15 (41.7) | |
| University | 5 (13.9) | 9 (25) | |
| Total | 36 (100) | 36 (100) | |
| Hire statement | 0.48 | ||
| No job | 17 (47.2) | 10 (27.8) | |
| Student | 1 (2.8) | 3 (8.3) | |
| Employed | 5 (13.9) | 6 (16.7) | |
| Retired | 8 (22.2) | 10 (27.8) | |
| Unemployed | 5 (13.9) | 7 (19.4) | |
| Total | 36 (100) | 36 (100) |
a Values are expressed as No. (%).
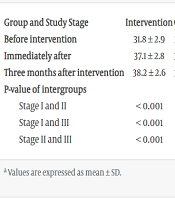
In the intervention group, variance with repeated measures revealed a significant difference in the mean score of disease perception at three measurement stages (before the intervention, immediately after, and 3 months after the intervention) (P < 0.001). In contrast, the control group showed no significant change compared to before the intervention (P = 0.36), and after three months, it still did not show a significant change (P = 0.94). The interaction effect of time and group indicated a significant difference in score changes between the two groups during the study (Table 2).
| Group and Study Stage | Intervention | Control | P-Value |
|---|---|---|---|
| Before intervention | 31.8 ± 2.9 | 31.7 ± 2.5 | 0.64 |
| Immediately after | 37.1 ± 2.8 | 32.1 ± 2.4 | < 0.001 |
| Three months after intervention | 38.2 ± 2.6 | 32.1 ± 2.2 | < 0.001 |
| P-value of intergroups | < 0.001 | ||
| Stage I and II | < 0.001 | 0.36 | |
| Stage I and III | < 0.001 | 0.42 | |
| Stage II and III | < 0.001 | 0.94 |
a Values are expressed as mean ± SD.
The perceived stress score showed significant changes immediately after and three months after the intervention compared to before the intervention (P < 0.001). In the control group, the perceived stress score did not change significantly after the intervention compared to before (P = 0.37), and there was no significant change after three months (P = 0.44). The interaction effect of time and group indicated a significant difference in score changes between the two groups during the study (Table 3).
| Group and Stage | Intervention | Control | P-Value |
|---|---|---|---|
| Before intervention | 28.7 ± 3.4 | 28.8 ± 2.6 | 0.70 |
| Immediately after | 25.4 ± 3.6 | 29.8 ± 3.2 | < 0.001 |
| 3 months after intervention | 24.1 ± 3.8 | 30.4 ± 3.1 | < 0.001 |
| P-Value of intergroups | < 0.001 | ||
| Stage I and II | < 0.001 | 0.37 | |
| Stage I and III | < 0.001 | 0.49 | |
| Stage II and III | < 0.001 | 0.44 |
a Values are expressed as mean ± SD.
Based on the results in Table 4, findings indicated that in the intervention group, the self-care score increased significantly after the intervention compared to before the intervention (P < 0.001), and it showed a significant increase again after three months (P < 0.001). In the control group, the self-care score did not increase significantly after the intervention compared to before (P = 1), and it still did not show a significant increase after three months (P = 0.18). The interaction effect of time and group revealed a significant difference in score changes between the two groups during the study.
| Group and Stage | Intervention | Control | P-Value |
|---|---|---|---|
| Before intervention | 56.5 ± 6.1 | 57 ± 3.6 | 0.76 |
| Immediately after | 64.6 ± 6.6 | 57 ± 4 | < 0.001 |
| Three months after intervention | 65.1 ± 8.4 | 55.5 ± 5 | < 0.001 |
| P-value of intergroups | < 0.001 | ||
| Stage I and II | < 0.001 | 1 | |
| Stage I and III | < 0.001 | 0.05 | |
| Stage II and III | < 0.001 | 0.18 |
a Values are expressed as mean ± SD.
5. Discussion
In this research, the effect of the family-centered empowerment model focused on spouses was investigated with regard to the perception of disease, perceived stress, and self-care behaviors in people with diabetes. According to the study results, the average score of disease understanding in the control group increased significantly after the intervention compared to before (P < 0.001). However, at the three-month follow-up, there was a significant decrease (P = 0.009), indicating the need for ongoing training during treatment.
These findings are consistent with the study by Rahimi and Karami Moghadam titled "the effect of the family-centered empowerment model on the perception of disease in heart failure patients." This study, which included 70 patients with heart failure, demonstrated that the model improved disease understanding and reduced symptom incidence. Rahimi concluded that, as a system, the family influences all its members, and maintaining this balance is crucial for effective management (17).
The study also found that the mean score of perceived stress did not change significantly before and after the intervention in the control group. In contrast, significant changes were observed in the intervention group, suggesting that the intervention was effective in improving perceived stress. These results align with the findings of Parvareshan et al., who investigated the impact of the family-centered empowerment model on perceived threat and self-efficacy in diabetic elderly families at risk of falling. Their study revealed that, while the average scores for perceived threat and self-efficacy were similar before the intervention, a significant increase was observed in the intervention group afterward (18).
Also, the results of this research are consistent with the previous study by Moghaddam Tabrizi and Nournezhad in 2016. In their research, titled "investigating the effect of counseling based on family support on perceived stress after childbirth and the mother-child bond in primiparous women referring to health centers in Urmia," it was reported that perceived stress significantly decreased in the intervention group compared to before the intervention (19).
Additionally, the findings align with the research conducted by Hara et al. in 2014. Their study revealed that gender and age differences are closely related to awareness, coping with stress, and treatment regimens in patients with type 2 diabetes, particularly noting that men are highly dependent on the support of their wives. Thus, providing educational programs is crucial for effective management (20).
The results of the current research are also consistent with the study by Jalili and Borimnejad in 2019, which indicated that implementing a family-centered program leads to a reduction in parents' anxiety and stress (21).
Furthermore, the study demonstrated a positive and significant effect of the family-centered empowerment program on the self-care of people with diabetes. This is in line with the results of Arabshahi et al.'s research in 2019, which examined the "effect of training based on spouse's social support on improving self-care behaviors in men with high blood pressure." This study, involving 112 male patients with primary hypertension and their wives, showed that education based on social support from the spouse improves self-care behaviors and reduces systolic blood pressure in patients with high blood pressure (22).
The current research findings are also supported by Razmarai et al.’s 2015 study, titled "investigation of the effect of family-oriented education on self-care in patients with type 2 diabetes." This experimental study involved 60 diabetic patients and demonstrated that family-oriented education by nurses has significant effects on self-care and its dimensions, including nutrition, physical activity, blood sugar control, and foot care (23).
In addition, the results of the present study align with the research conducted by Teufel-Shoneet al. in 2005, tittled "developing and adapting a family-based diabetes program at the U.S.-Mexico border." Their study demonstrated that effective involvement of family and friends contributed to long-term behavior change, increased self-efficacy, improved self-care, and enhanced dietary habits among patients with type 2 diabetes (24).
Although the results of this study are consistent with many other studies on family-centered program implementation, which have reported positive effects such as improved understanding in heart patients, increased self-efficacy and perceived threat reduction in diabetic patients, decreased anxiety in parents of children with convulsions, and enhanced self-care in diabetic patients, other research has shown that family support and counseling lead to a better understanding and reduced stress among family members in illness situations.
An important aspect of the positive outcomes in this study is the improved understanding of the disease, reduced perceived stress among spouses, and increased self-care ability resulting from the family-centered empowerment program. This is based on two key principles:
(1) Empowering and increasing the knowledge of the patient’s spouse simultaneously with the research team in the family-centered care program, which has strengthened learning and motivation for family care.
(2) Follow-up by the care team along with the strong interest of the family, especially the spouses, in illness and related care, which has led to better understanding, reduced stress, and improved self-care ability among the spouses.
5.1. Conclusions
The findings of this study indicate that a family-centered empowerment program tailored to the educational needs of patients and involving their spouses results in improved disease perception, reduced perceived stress, and enhanced self-care. Given the positive impact of this program in empowering spouses to take a fundamental role in patient care, it can be considered a cost-effective and valuable method within the nursing and health community. This approach could positively affect patients’ skills, enhance self-efficacy, and improve motivation and emotional well-being by fostering family involvement.