1. Background
Antiphospholipid syndrome (APS) is an autoimmune disease primarily characterized by thrombosis (1-3). Thrombosis can occur in any organ of the patient. This disease is generally marked by coagulation processes triggered by antiphospholipid antibodies (4). While antiphospholipid antibodies can be present naturally in healthy individuals, in AP patients, they lead to arterial thrombosis, decreased platelet count, and disrupted fetal development. Antiphospholipid syndrome can present as an isolated condition or in conjunction with other autoimmune diseases (5-8). The exact pathogenesis of thrombosis in AP patients remains unclear; however, a reduction in anticoagulant proteins has been identified as a potential contributing factor. Recent studies have indicated decreased serum levels of proteins S and C in AP patients. Additionally, elevated homocysteine levels have been observed in AP patients with thrombosis. Despite these findings, few studies have comprehensively examined the relationship between serum levels of anticoagulant factors and thrombosis in AP patients (9, 10).
One study found that increased levels of protein S, protein C, and factor V Leiden in AP patients were associated with a heightened risk of thrombosis (11-13). Various studies have also indicated that disruptions in the structure or function of coagulation factors in AP patients can be linked to miscarriage. For example, one study demonstrated that abnormalities in protein C and its receptor were associated with miscarriage in pregnant women (14). However, other studies did not find a correlation between coagulation factors and miscarriage incidence (15).
2. Objectives
Given the contradictory results of previous studies and the limited scope of research on the relationship between multiple coagulation factors and miscarriage, this study aimed to investigate the prevalence of protein S, protein C, factor V Leiden, and homocysteine in AP patients.
3. Methods
This study was approved by the Ethics Committee of Jundishapur University of Medical Sciences, Ahvaz. It is a retrospective study based on the clinical information of patients available in their files at Golestan Hospital, Ahvaz.
In this study, we examined the files of patients who had experienced miscarriages and were referred to Golestan Hospital and private rheumatology clinics in Ahvaz since 1995. These patients had been examined for coagulation factors. The inclusion criteria comprised patients with no underlying diseases or coagulation disorders. The exclusion criteria included patients with incomplete file information and those with coagulation disorders.
A pre-prepared checklist, designed by the researcher, was used to collect clinical information from the patients' records. The checklist included demographic information, prevalence of miscarriage, vascular disorders (arterial-venous), pulmonary and venous thrombosis, preterm labor, intrauterine fetal death (IUFD), intrauterine growth restriction (IUGR), and deficiencies of proteins C and S, as well as levels of homocysteine.
3.1. Ethical Section
The code of ethics obtained for conducting this study was IR.AJUMS.HGOLESTAN.REC.1400.056 from the Ethics Committee of Ahvaz University of Medical Sciences.
3.2. Statistical Analysis
In this research, descriptive statistics, including mean and standard deviation (for quantitative variables) and frequency and frequency percentage (for qualitative variables), were used. After assessing the normality of the data using the Kolmogorov-Smirnov test, we examined the research hypotheses. Depending on the normality of the data, parametric statistics (independent t-test, paired t-test, and analysis of variance) or non-parametric tests (Mann-Whitney, Kruskal-Wallis) were used to test the research hypotheses. All statistical analyses were performed using SPSS version 22 software.
4. Results
4.1. Demographical Information
The following table presents the demographic data of the patients. The average age of the patients was 32.24 ± 6.05 years. Pregnancy and miscarriage data are shown in Table 1 as frequency and percentage, ranging from zero to 10. Information regarding live birth, IUFD, and IUGR is shown with frequencies ranging from 0 to 3. A reduction of C and S proteins was observed in 18 (15.1%) and 20 (16.8%) patients, respectively. Thrombosis was present in 103 (86.6%) patients, and 27 (22.7%) patients had Aps Ab. The level of homocysteine in all patients was within the normal range. Other data and their frequencies are detailed in Table 1.
| Variables | Patients (N = 119) |
|---|---|
| Age (y) | 32.24 ± 6.05 |
| Gravidity | |
| 0 | 4 (3.4) |
| 1 | 11 (9.2) |
| 2 | 22 (18.5) |
| 3 | 34 (28.6) |
| 4 | 17 (14.3) |
| 5 | 13 (10.9) |
| 6 | 4 (3.4) |
| 7 | 2 (1.7) |
| 8 | 3 (2.5) |
| 9 | 2 (1.7) |
| 10 | 1 (0.8) |
| Abortions | |
| 0 | 22 (18.5) |
| 1 | 16 (13.4) |
| 2 | 37 (31.1) |
| 3 | 17 (14.3) |
| 4 | 11 (9.2) |
| 5 | 5 (4.2) |
| 6 | 1 (0.8) |
| 7 | 1 (0.8) |
| 8 | 1 (0.8) |
| 9 | 1 (0.8) |
| 10 | 1 (0.8) |
| Live birth | |
| 0 | 49 (41.2) |
| 1 | 38 (31.9) |
| 2 | 21 (17.6) |
| 3 | 5 (4.2) |
| IUGR | |
| 0 | 114 (95.8) |
| 1 | 4 (3.4) |
| 2 | 1 (0.8) |
| IUFD | |
| 0 | 108 (90.8) |
| 1 | 8 (6.7) |
| 2 | 2 (1.7) |
| 3 | 1 (0.8) |
| Protein C | |
| Low | 18 (15.1) |
| Normal | 101 (84.9) |
| Protein S | |
| Low | 20(16.8) |
| Normal | 99 (83.2) |
| Homocysteine | |
| Low | 0 (0) |
| Normal | 119 (100) |
| Factor V Leiden | |
| Low | 2 (1.7) |
| Normal | 114 (95.8) |
| High | 3 (2.5) |
| vascular events | |
| Neg | 16 (13.4) |
| DVT+ | 103 (86.6) |
| Thrombose | |
| Negative | 16 (13.4) |
| Positive | 103 (86.6) |
| Aps Ab | |
| Negative | 27 (22.7) |
| Positive | 92 (77.3) |
| FANA | |
| Negative | 6 (5) |
| Positive | 113 (95) |
| CH50 | |
| Low | 1 (0.8) |
| Normal | 118 (99.2) |
| dsDNA | |
| Negative | 5 (4.2) |
| Positive | 114 (95.8) |
| C3 | |
| Low | 1 (0.8) |
| Normal | 118 (99.2) |
a Values are expressed as No. (%) or mean ± SD.
4.2. Evaluation of Relation Between Protein C and Gravidity
Based on logistic regression analysis, it was shown that protein C can be considered a risk factor. The results demonstrated a significant relationship between protein C and the gravidity factor. This relationship was statistically significant (CI 95%: 0.043 - 0.431, P = 0.001) (Table 2).
| Variable | Protein C | P-Value | ||
|---|---|---|---|---|
| Exp (B) | CI 95% | |||
| Upper | Lower | |||
| Gravidity | 0.136 | 0.043 | 0.431 | 0.001 a |
a P < 0.01 show significant P-value.
4.3. Evaluation of Risk Factor of Intrauterine Fetal Demise(IUFD) and Intrauterine Growth Restriction (IUGR) Using Logistic Regression Based on Protein C and Aps Ab
Based on the table below, there was a significant relationship between protein C and the occurrence of IUFD (P = 0.05) and IUGR (P = 0.0726). The results also showed no correlation between APS Ab and IUFD (P = 0.207) and IUGR (P = 0.534) (Table 3).
a P < 0.05 show significant P-value.
b P > 0.05 indicates a non-significant P-value.
4.4. Evaluation of Abs Ab with Protein C, Thrombose and Vascular Events
According to the table below, vascular events were equal in patients with and without Abs, while negative cases were more frequent in the Abs Ab negative group (P = 0.009). The incidence of thrombosis was also the same in both groups, while the prevalence of patients without thrombosis was higher in the Abs Ab negative group (P = 0.009). The percentage of patients with decreased protein C levels was higher in the Abs Ab negative group, and this difference was statistically significant (P = 0.001) (Table 4).
a P < 0.01 show significant P-value.
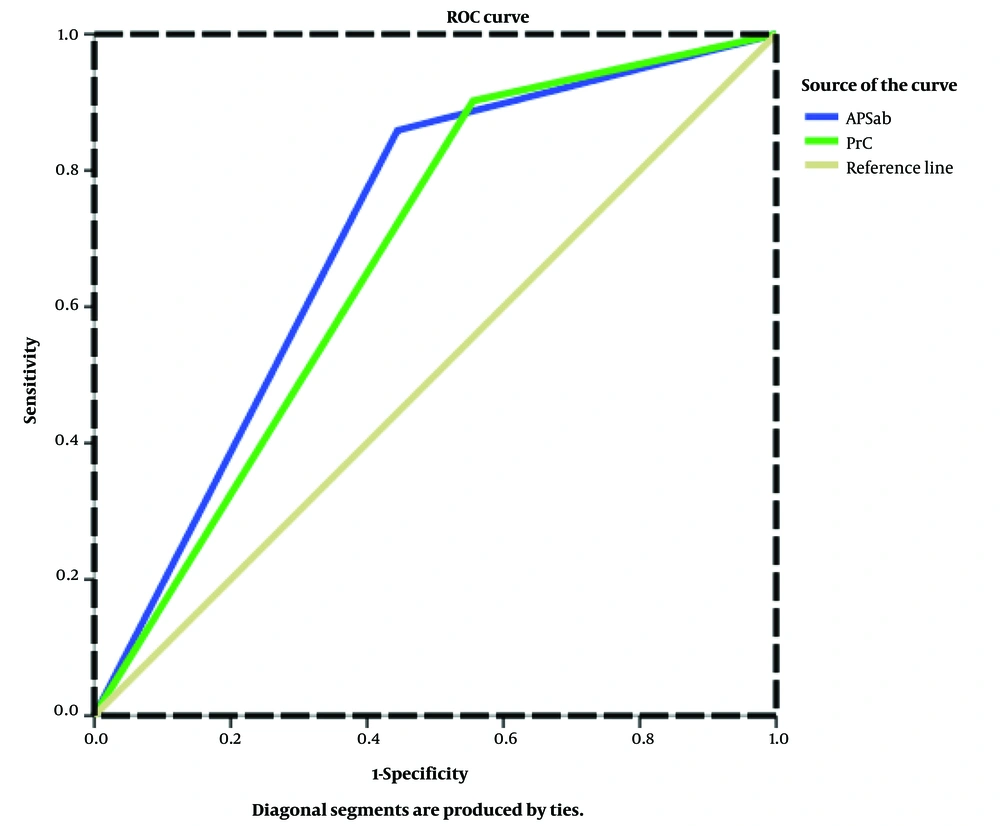
4.5. Evaluation of the Diagnostic Value of Protein C and Abs Ab
To evaluate the diagnostic value of protein C and Abs Ab, receiver operating characteristic (ROC) curves were plotted. The Area Under the Curve (AUC) values were then analyzed. It was found that both protein C and Abs Ab had diagnostic value in AP patients (Figure 1).
Receiver operating characteristic (ROC) curves for models to predict atherosclerosis. The Area Under the Curve (AUC) showed higher value in model for Abs Ab as a marker for gravidity related disorders detection (P < 0.01, AUC = 0.70). Area Under the Curve showed higher value in model for protein C as a new marker for Gravidity related disorders detection (P < 0.05, AUC = 0.67).
5. Discussion
In the present study, the results showed that the reduction of proteins C and S was observed in 18 (15.1%) and 20 (16.8%) patients, respectively. Additionally, 103 (86.6%) patients had thrombosis, and 27 (22.7%) patients had APS antibodies. Based on the results, it was shown that all three factors—protein C, thrombosis, and vascular events—were related to patients with and without APS antibodies, which was statistically significant.
In the study by Matin et al., it was shown that the prevalence of protein C deficiency was the most common defect in patients with miscarriage (16). Conversely, Vomstein et al.'s study indicated that there was no relationship between disorders in coagulation factors such as protein C, protein S, antithrombin III, and other coagulation factors with the incidence of miscarriage in patients with antiphospholipid syndrome (17). Additionally, Mekaj et al.'s study found no correlation between protein C, S, and antithrombin III deficiencies in patients with antiphospholipid syndrome and abortion compared to the control group (15). In the study by Al-Allawi et al., it was shown that there was a relationship between defects in protein C and its receptor and the incidence of spontaneous abortion in pregnant women (14).
The results of previous studies were not consistent with the present study. The reason for this difference may be the prevalence of mutations in coagulation factors. This discrepancy could also be related to the number of patients in each study and the type of diseases investigated.
In the present study, the results showed a significant relationship between Protein C and IUFD. However, there was no significant relationship between Aps Ab and IUFD or IUGR. In the study by Morad et al., it was found that antibodies against dsDNA in patients with antiphospholipid syndrome caused pregnancy complications, including miscarriage (18). Similarly, Al Samarrai et al. showed that the antibody against dsDNA was higher in patients with antiphospholipid syndrome compared to those without it, which was associated with an increase in abortions (19). In contrast, the present study found no correlation between the presence of dsDNA antibodies and the occurrence of abortions. This discrepancy could be due to differences in the number of patients participating in the studies or the classification of patients.
In Zhang et al.'s study, increased antiphospholipid production in patients was associated with the occurrence of pregnancy complications, including miscarriage (20). Similarly, Ruffatti et al. found that the presence of antiphospholipid antibodies was associated with an increase in miscarriages (21). The differences in the results between studies could be due to the examination of different pregnancy outcomes. Different studies have evaluated various variables compared to the present study, leading to differences in the type of outcomes and their respective percentages.
5.1. Conclusions
The results indicated that protein C can be used as a diagnostic factor in AP patients. Additionally, protein C was found to be associated with IUFD in these patients.