1. Background
Due to the complications and chronic nature of congenital heart disease (CHD), providing physical, emotional, and social care to these children at various life stages is vital (1). Apart from the serious health implications for patients, the substantial medical expenses and frequent hospitalizations pose significant challenges for their families (2). Numerous studies have demonstrated that parents of children with health issues are more susceptible to facing social, economic, and emotional difficulties that can be constraining, detrimental, and far-reaching in nature. While this situation impacts the entire family, mothers often bear the brunt of responsibilities due to their traditional caregiving role (2-4). As primary caregivers, mothers not only grapple with financial burdens but also contend with grief, depression, anxiety, anger, despair, shame, and even physical and physiological ailments such as heart conditions throughout their lives (5). Naturally, the need for surgery in treating a disease exacerbates stress levels, particularly for mothers, as children with congenital heart defects require surgical intervention, intensifying the physical and psychological strain on parents, especially mothers, throughout the treatment process (6).
Given that parents' caregiving experiences may vary based on their geographical location (7) and that cultural norms, legal frameworks, and healthcare systems can influence the experiences of mothers whose children undergo heart surgery (8), it is essential to explore these aspects. A review of the literature reveals that most studies on CHD have been quantitative, focusing on measuring parental distress, frustration, and quality of life, with fewer studies delving into the specifics of CHD surgery. Qualitative research proves invaluable when there is insufficient understanding of the phenomenon in question and when existing measurement tools are inadequate. Given the considerable number of children affected by CHD and the fact that surgery is often the primary treatment modality, qualitative studies are warranted in Iran, where socio-economic status, religious beliefs, cultural practices, healthcare systems, and treatment facilities differ from those in other countries where such research has been conducted.
2. Objectives
This study aimed to elucidate the experiences of Iranian mothers regarding their child's CHD surgery.
3. Methods
3.1. Design
This qualitative study employed a conventional content analysis approach based on Graneheim and Lundman's method (9).
3.2. Participants
Twenty mothers were purposively selected based on predefined inclusion criteria. Eligible participants were primary caregivers accompanying children undergoing CHD surgery in the pediatric cardiac surgery and intensive care units at the Pediatrics Medical Center in Tehran. Inclusion criteria required participants to be fluent in Persian and have no history of cognitive or mental disorders. Exclusion criteria included a decision by participants to withdraw from the study. Maximum variation sampling was utilized to ensure diverse perspectives and a comprehensive understanding of the phenomenon. Participants were selected with varying educational backgrounds, ages, children of both genders, and different CHD diagnoses. Sampling was conducted between June 2019 and September 2020.
3.3. Data Collection
The primary data collection method employed was unstructured interviews. Each participant underwent face-to-face interviews at three stages: pre-surgery (at least 24 hours after the child's hospitalization), perioperative (during the operation and 8 - 12 hours post-operation), and post-discharge (up to two weeks after discharge). These interviews took place in a designated quiet room provided by the hospital, both during the child's hospitalization and during post-operative follow-up visits. The timing of the first two interviews was arranged in person with the participants, while the timing of the third interview was coordinated via phone. Prior to each interview, informed written consent was obtained from the participants, along with permission to record the sessions. Participants were encouraged to share their experiences and memories by responding to open-ended questions. The interviews commenced with the key question: "Please tell me about your feelings, concerns, and needs during these days when (child’s name) is hospitalized/ operated/ discharged." Subsequent questions were tailored based on the participant's responses and the research objectives. Exploratory questions, such as "Can you explain more/give an example?" were utilized to guide the conversation in line with the participants' narratives. Additionally, at the conclusion of each interview, open-ended questions such as "Do you think there is something you did not say?" were posed. Nonverbal reactions were recorded using note-taking. The duration of interviews ranged from 45 to 90 minutes, contingent upon the participants' willingness and cooperation. The researcher also documented field notes and any unplanned observations. Data collection persisted until data saturation was achieved, indicating that all research concepts were sufficiently elucidated, and subsequent interviews did not yield new categories.
3.4. Data Analysis
The data analysis was conducted concurrently with data collection, utilizing the Graneheim and Lundman content analysis approach (9) and MaxQDA software version 2010. The following steps were undertaken:
1. The verbatim transcription of the interviews was initially hand-written, then typed into Word software, and subsequently imported into MaxQDA software. Each interview, including paragraphs, sentences, and words, was treated as a semantic unit. The interviews and field notes were thoroughly reviewed multiple times to ensure a comprehensive understanding of the content.
2. Semantic units were extracted and then abstracted and conceptualized to reveal the underlying concepts, which were then labeled with codes.
3. Primary categories were developed through the merging and classification of semantic units to summarize and categorize cohesive units, with appropriate labels assigned.
4. Sorting the primary categories based on similarities and differences led to the creation of sub-categories.
5. Final categories were conceptualized by synthesizing similarities, differences, and constant comparisons, and suitable titles were selected to encompass the derived categories (9).
All coding and classification steps for both interviews and field notes were independently performed by the three members of the research team. Subsequently, the results were compared, and any discrepancies were resolved through consultation and consensus.
Trustworthiness, or rigor, defines the quality criteria in qualitative research, as per Lincoln and Guba (10, 11). To ensure credibility, several strategies were employed, including prolonged engagement, persistent observation, triangulation, and member checks. Researchers engaged with the data extensively by dedicating ample time to both data collection and analysis. They integrated various data collection methods, such as interviews and field notes, and recorded unplanned observations. Continuous comparison analysis and review by participants were conducted by sharing the results with five participants to verify the accuracy of the researchers' analyses and interpretations. To ensure transferability, sampling with maximum variation was employed, and a descriptive, data-rich report was provided, not only detailing behaviors and experiences but also their context. The results were also presented to five mothers with similar statuses who were not participants, to evaluate the consistency of the findings with their experiences. Dependability and confirmability were strengthened through team analysis methods and review by experts. Parts of interviews, coding, and classifications were shared with two external auditors to supervise and confirm all research steps. Reflexivity was enhanced by observing bracketing with researchers, who documented all assumptions and values at every stage of the research to avoid interpretation bias.
3.5. Ethics Approval and Consent to Participation
All methods were conducted in accordance with the Helsinki declaration. The study protocol received approval from the Ethics Committee of Lorestan University of Medical Sciences (ethics code: IR.LUMS.REC.1398.125). Written informed consent was obtained from all participants for their participation and for recording the interviews. Participants were informed of the voluntary nature of their participation and their right to withdraw from the research at any time. They were assured that their statements would not be reported directly to hospital officials or staff. Confidentiality of information, including the removal of names and identifying marks from recorded interviews and texts during publication, was guaranteed.
4. Results
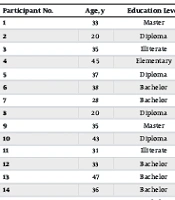
The participants' age ranged from 20 to 50 years, and their educational level varied from illiterate to master's degree. Demographic characteristics of the participants and their children are presented in Table 1.
| Participant No. | Age (y) | Education Level | Child’s Diagnosis | Child’s Age (mon) |
|---|---|---|---|---|
| 1 | 33 | Master | Tetralogy of Fallot | 6 |
| 2 | 20 | Diploma | Transposition of great arteries | 18 |
| 3 | 35 | Illiterate | Tetralogy of Fallot | 6 |
| 4 | 45 | Elementary | Tricuspid atresia | 60 |
| 5 | 37 | Diploma | Single ventricle | 24 |
| 6 | 38 | Bachelor | Single ventricle | 8 |
| 7 | 28 | Bachelor | Pulmonary atresia | 12 |
| 8 | 20 | Diploma | Transposition of great arteries | 6 |
| 9 | 35 | Master | Tetralogy of Fallot | 13 |
| 10 | 43 | Diploma | Aortic stenosis | 6 |
| 11 | 31 | Illiterate | Pulmonary atresia | 18 |
| 12 | 33 | Bachelor | Aortic stenosis | 8 |
| 13 | 47 | Bachelor | Atrioventricular septal defect | 6 |
| 14 | 36 | Bachelor | Tetralogy of Fallot | 6 |
| 15 | 38 | Bachelor | Ventricular septal defect -Pulmonary HTN | 23 |
| 16 | 30 | Bachelor | Anomalous left coronary artery from the pulmonary artery | 12 |
| 17 | 38 | Bachelor | Tetralogy of Fallot | 18 |
| 18 | 40 | Diploma | Transposition of great arteries | 6 |
| 19 | 30 | Diploma | Pulmonary Venous Connection | 18 |
| 20 | 39 | Diploma | Single ventricle | 18 |
Demographic Characteristics of the Participants and Their Children
From a total of 60 interviews and 11 field notes, 897 codes, 26 primary categories, 10 subcategories, and 4 main categories were abstracted (Table 2).
| Main Categories | Subcategories | Initial Categories |
|---|---|---|
| Bitter and difficult motherhood experience | Shocked by the child's abnormality | Unexpectedness |
| Facing with child’s difficulties | ||
| Stormy feelings | ||
| Challenges to being resilient in child care | Changes in living conditions | |
| Alone in taking care of the child | ||
| Difficulty in accessing available services | ||
| The need to be strong | ||
| In search of reassurance | In search of information | Consulting with staff |
| Observe and ask the peers | ||
| Searching the Internet | ||
| In search of the best services | Seeking the diagnosis confirmation | |
| Making sure of the surgeon and hospital | ||
| Tides in supportive network | Personnel conscientiousness with low empathy | Improper preparation |
| Breaking the communication ice for surgical success | ||
| Surrounding people: Stressful supporters | The difficulty of accepting the child problem | |
| Without hesitation support from others | ||
| Peers stressful support | Transferring stressful information | |
| Receiving empathy and experience | ||
| Relative calm after the storm | Overcoming the nightmare of surgery with spirituality | Accepting the surgery |
| Exhausting waiting | ||
| Relying on spirituality | ||
| Light of hope after the nightmare of surgery | Happiness to see the child alive after surgery | |
| Facing the unpleasant condition of the child after surgery | ||
| Getting the spirit after witnessing recovery of the symptoms | ||
| Endless concerns | Discharge with worries about home care | |
| Sensitivity and stress of child care at home | ||
| Worried about the ambiguous future |
Main Categories, Subcategories and Initial Categories
4.1. Bitter and Difficult Motherhood Experience
The birth of a child with CHD made the motherhood experience bitter and difficult due to being "shocked by the child's abnormality" and subsequent "difficult resilience in taking care of the child."
4.1.1. Shocked by the Child's Abnormality
Mothers' experience of becoming the mother of a child with CHD was marked by "unexpectedness," wherein they "faced the child’s difficulties" with "stormy feelings."
4.1.1.1. Unexpectedness
Participants expressed that this experience caught them off guard. One mother stated, "My husband and I had no family member with this problem at all, or even in our ancestors. I did not think of such a thing at all" (Participant 5).
4.1.1.2. Facing Child’s Difficulties
Mothers devoted significant time to their child's daily care, including attending to special medical and nutritional needs and preventing infections. One mother explained, "All the time I was just looking after my son, giving him medication, breastfeeding, and monitoring his breathing, not letting him cry" (Participant 11).
4.1.1.3. Stormy Feelings
Mothers experienced fear, worry, and persistent negative thoughts about losing their child, often desiring to withdraw from others. A mother expressed, "Everything was messed up. My husband and I were very anxious and worried. We could not concentrate on anything. We did not want to see anybody" (Participant 6).
4.1.2. Challenges in Building Resilience in Childcare
Mothers faced hurdles in overcoming "Changes in life conditions," "Loneliness in caring for the child," "The need to be strong," and "Difficulty in accessing services" while caring for their child.
4.1.2.1. Changes in Living Conditions
The birth of a child with CHD brought about significant changes in the mothers' lives. One mother expressed, "I couldn't even go to the park. Once he had a lung infection, I stayed home for two months. I didn't even visit my parents, and no one visited us either" (Participant 1).
4.1.2.2. Isolation in Childcare
Many mothers found themselves alone in caring for their child, often due to the need to isolate the child to prevent infections. A mother shared, "I had no prior experience in childcare. I thought my family would assist, but I ended up handling everything alone. Although they were willing to help, I couldn't allow it due to the child's condition" (Participant 1).
4.1.2.3. Difficulty Accessing Services
Most mothers encountered challenges in accessing essential healthcare services for their child, particularly surgery. One mother explained, "The lack of facilities and specialized doctors in our city, even in the provincial capital, compelled us to travel to Tehran" (Participant 9).
4.1.2.4. The Need for Strength
Mothers had to summon strength to navigate through challenging situations in caring for their children. One mother affirmed, "I tried to learn and cope. I had to face the problems head-on" (Participant 8).
4.2. In Search of Reassurance
Mothers endeavor to ensure the correct diagnosis and appropriate quality of treatment for their child by seeking information and providing the best medical services.
4.2.1. Seeking Information
Before the child’s surgery, mothers endeavored to enhance their knowledge and skills regarding the child’s diagnosis, surgery, prognosis, and care by consulting with staff, observing and asking peers, and searching the Internet.
4.2.1.1. Consulting with Staff
One of the most important sources of acquiring information for mothers was consulting with hospital staff. One mother said: "At first, I did not know what the problem was. I asked her doctor and one of the nurses. I felt relieved and better when they said that this disease can be cured" (Participant 11).
4.2.1.2. Observing and Asking Peers
Mothers observed the recovery of similar children and tried to learn from their mothers to take care of their child. "Here in the hospital, we met families having children with the same disease as ours. The information they gave us helped a lot," one mother said (Participant 5).
4.2.1.3. Searching the Internet
After the child's diagnosis is raised, mothers search the Internet to increase their information about the disease. "I read on the Internet about her illness and wanted to know if it may be cured by medication, but all the sources stated that it can only be cured through surgery," said one mother (Participant 17).
4.2.2. In Search of the Best Services
The mothers’ efforts to ensure the correct diagnosis and to provide safe care and surgery for their child involved seeking confirmation of the diagnosis and making sure of the surgeon and the hospital.
4.2.2.1. Seeking Diagnosis Confirmation
Almost all the mothers consulted several specialists and underwent multiple diagnostic tests. A mother said: "At first, even when we did the echo, it was not acceptable to us. Then we went to another doctor, and he said that again, this time we take him to a super-specialist" (Participant 15).
4.2.2.2. Making Sure of the Surgeon and Hospital
After accepting their child's diagnosis, the mothers sought to find a suitable hospital and the most skilled surgeon to perform their child's surgery. "Our biggest concern was to find a good doctor and a good hospital to do the operation," said one mother (Participant 1).
4.3. Tides in Supportive Networks
Mothers, to overcome the difficulties of their child’s CHD, benefit from the various supports of their social support network. However, they sometimes face inappropriate and stressful behaviors from this network. The subcategories were "personnel conscientiousness with low empathy", "surrounding people: stressful supporters", and "peer stressful support".
4.3.1. Personnel Conscientiousness with Low Empathy
The "improper preparation" and "breaking the communication ice for surgical success" indicated that the staff performed their duties with low empathy for the mothers.
4.3.1.1. Improper Preparation
Inadequate preparation of mothers for the child’s surgery intensified their anxiety and fear of surgery. For example, just talking about the complications of surgery, when obtaining surgical consent, instead of supporting the mothers, was more disclaiming the responsibility from the doctor and staff. One mother said: “What the doctor said about the surgery increased our stress. We felt like someone whose child went to the battlefield" (Participant 4).
4.3.1.2. Breaking the Communication Ice for Surgical Success
The experience of mothers showed that as they got closer to the time of surgery, communication with doctors and nurses became closer. A mother stated: "I was crying when I was delivering my son to the operating room. Meanwhile, a young male nurse said kindly: Don’t worry. He will soon get out safe and sound. I have not seen such good behavior before that" (Participant 15).
4.3.2. Surrounding People: Stressful Supporters
Family members, friends, and neighbors, by "the difficulty of accepting the child's problem" and "without hesitation support," had an effective role in both supporting and exacerbating the stress and sadness of the mothers.
4.3.2.1. "The Difficulty of Accepting the Child’s Problem"
Due to unnecessary curiosity about the child's illness, advice to hide the child's illness, and lack of cooperation in following the principles of infection control, surrounding people made the problem harder for the mothers. A mother said: "My sister called me and said, 'Why don’t you take her to a good doctor?' I got so angry that I hung up the phone" (Participant 11).
4.3.2.2. Without Hesitation Support from Others
The mothers generally benefited from the sympathy and emotional or financial support of friends, family, and relatives. One mother said, "My husband’s family helped a lot; they accompanied us, gave us their financial support, and their presence was so comforting for us" (Participant 7).
4.3.3. Peers’ Stressful Support
Mothers with similar problems, by "transferring stressful information" and "giving empathy and experience," while being excellent sources of support, sometimes intensified each other's stress.
4.3.3.1. Transferring Stressful Information
Sometimes receiving irrelevant information from other mothers exacerbated mothers' concerns. "We had very bad thoughts because we were in contact with other families; sometimes they were giving us the wrong information," said one mother (Participant 2).
4.3.3.2. Receiving Empathy and Experience
The transfer of information and experience by other mothers and receiving comfort and hope from them made it easier for inexperienced mothers to accept the situation. A mother said: "Communicating with other mothers, especially those whose child had a successful surgery, gave us a lot of hope, and the process was becoming easier for us to go through" (Participant 16).
4.4. Relative Calm After the Storm
After "overcoming the surgery nightmare with spirituality," the “light of hope after the surgery nightmare,” and "endless worries," the mothers reached a state of relative calm.
4.4.1. Overcoming the Nightmare of Surgery with Spirituality
Usually, mothers overcame the nightmare of surgery by "accepting the surgery" and enduring "exhausting waiting" outside the operating room by "relying on spirituality.”
4.4.1.1. Accepting the Surgery
Despite the possibility of surgery failure and complications, mothers consented to the surgery to free their child from hardship. A mother talked about her acceptance to relieve her child's suffering: “He used to be short of breath, bruise, and faint. I wished his turn for surgery would come sooner to relieve him from suffering" (Participant 17).
4.4.1.2. Exhausting Waiting
The mothers' experiences showed endurance, pressure, stress, and excessive worry during the child's surgery. A mother said: “When the surgery was done, it was a horrible feeling that my child was kept away from me and I could not do anything” (Participant 14).
4.4.1.3. Relying on Spirituality
The mothers’ hope in God, praying, doing charities, and reading the holy Quran helped them relax, especially during the surgery. One participant stated: "The thing that calmed us down in those circumstances was trusting in God and praying. That was the only thing we could do" (Participant 16).
4.4.2. Light of Hope After the Nightmare of Surgery
The mothers experienced "happiness to see the child alive after surgery," but after transferring to the cardiac intensive care unit, they "saw the child in a bad condition." Then gradually, they experienced "getting the spirit after witnessing the recovery of the symptoms" and "a light of hope shone in their hearts" after all their hardships and sufferings.
4.4.2.1. Happiness to See the Child Alive After Surgery
Mothers described it as a joyful moment when the child left the operating room and the surgery was successful. One mother said: "When he came out and the doctor said the operation was successful, I was delighted. It was as if my child had been given back to me" (Participant 11).
4.4.2.2. Facing the Unpleasant Condition of the Child After Surgery
Mothers began to feel worried when the child was transferred to the intensive care unit for cardiac surgery. A mother said: "I cried all the time because he had tape over his eyes, something was attached to his mouth. He could not look at us at all" (Participant 15).
4.4.2.3. Getting the Spirit After Seeing Recovery of the Symptoms
After surgery, the absence of the child's previous symptoms reassured the mother of the success of the surgery. One mother stated: "Previously, when she cried, she would turn blue and be short of breath. After surgery, she is not like that, and I realized that my baby was doing well" (participant 4).
4.4.3. Endless Concerns
Mothers often experienced "discharge with concern for home care." They had "sensitivity and high stress for child care at home," and they were "worried about the ambiguous future."
4.4.3.1. Discharge with Worries About Home Care
At the time of discharge, mothers were still worried about the possibility of complications after surgery and how to care for the child at home. A mother said: "We had a dual feeling. Happy that we were released from the hospital but sad that something may happen to him at home and we do not have access to anything" (Participant 2).
4.4.3.2. Sensitivity and Stress of Child Care at Home
After returning home, mothers were the primary caregivers of the child and tried to be accurate in providing child care, which was accompanied by a lot of stress. "When we went home, first I was scared and worried, even when I was taking him to a bath or changing clothes," said one mother (Participant 5).
4.4.3.3. Worried About the Ambiguous Future
Mothers were always worried about the restrictions due to this disease and its impact on the employment and marriage of the child in the future. "It's burdensome, what will happen in the future. Can she live like everyone else, can she play like other children, or can she get married?" said one mother (Participant 7).
5. Discussion
This study delved into the experiences of mothers whose children underwent surgery for CHD. "Bitter and Difficult Motherhood Experience" encapsulates the unexpectedness of giving birth to a child with CHD and the necessity of surgery at a young age, which poses challenges for mothers in resiliently caring for their child. The diagnosis of CHD can induce significant emotional shock in mothers (12). Fear of losing a child is identified as one of the most profound and distressing psychological stresses for parents (13). Managing CHD requires continuous monitoring, multiple long-term interventions, and often surgery, which can exacerbate mothers' mental well-being (4, 14, 15). Previous research, such as that by Sabzevari et al., has highlighted how mothers perceive a decline in their quality of life, significantly impacting their ability to care for their child (16). Studies by Bruce et al. have shown that mothers of children with CHD often have to make personal sacrifices (17). Preparing mothers to cope with such challenging circumstances is crucial, starting from the moment the child's diagnosis is confirmed. Hosseinrezaei et al. found that education significantly reduces anxiety among these mothers and improves their caregiving performance (18). Additionally, given the high prevalence of CHD and the challenges associated with timely diagnosis, increasing public awareness and providing facilities for perinatal diagnosis and intrauterine surgery are imperative. The utilization of telemedicine facilities could potentially mitigate issues arising from the lack of diagnostic and treatment resources in less developed regions.
"In Search of Reassurance" refers to the efforts made by mothers to seek information and access the best services. In a qualitative study, David Vainberg et al. found that for parents, the experience of their child undergoing CHD surgery could be perceived as a turbulent period characterized by uncertainty, confusion, and helplessness (19). At this stage, mothers sought to confirm the correctness of the diagnosis and the necessity of surgery by asking questions to healthcare professionals, consulting with parents of children with similar conditions, and searching the Internet. However, in many cases, these efforts led to stress and sometimes resulted in receiving inappropriate information. Khalifehzadeh et al. also emphasized that doctors and other healthcare team members must pay more attention to providing these mothers with information about the disease, treatments, and post-surgery care for children, as well as informing them about supportive care centers (6). Additionally, creating virtual support groups for mothers and monitoring the exchange of accurate information among them, or recommending reputable websites for parents to obtain information and providing educational brochures, can help reassure mothers without requiring extensive time commitments.
The dynamics of network support underscore the need to combine the support of the healthcare team with empathy, while also making the support from surrounding individuals and peers less stressful for mothers. In a study by Valizadeh et al., parents considered certain beyond-the-duty tasks performed by the staff, comprehensive family support, and mutual facilitation among peers as resources to support them during their child’s surgery (20). The behavior of the staff plays a significant role in the mental states of patients' companions and can contribute to stress and anxiety (21). Khalifehzadeh et al. reported that healthcare professionals are expected to be more available to respond to mothers' requests (6). Therefore, healthcare providers need to enhance their insights and perspectives on how to support mothers. For example, when obtaining consent before surgery, in addition to discussing the potential complications, it's important to highlight the benefits of the procedure. Overall, the support provided to parents should aim to minimize their negative experiences, thus strengthening their ability to cope internally (19). Accordingly, healthcare providers should assess each family’s support resources and organize them to address deficiencies and shortcomings in the health service delivery system (20). This involves providing both technical and emotional support to mothers to promote humanized care (22) and underscores the importance of creating a perception of support from the healthcare system for mothers (23).
The relative calm after the storm indicates the difficulty of accepting the double-edged sword of surgery. Then, with the assistance of spirituality, the success of the surgery, and the improvement of the child's physical condition, mothers gradually overcome the turmoil of surgery and achieve relative calmness. However, they still harbor endless worries about the child's health and life in the future. Examining the experiences of parents shortly after their children returned home from the hospital following CHD surgery, Simeone et al. also mentioned terms like happiness and uncertainty. They argued that these feelings arise when individuals encounter a new situation without a sense of security (24). The fear of the child's uncertain future, treatment plan, and disease prognosis can lead to psychological problems, especially in mothers (25). In the present study, mothers, despite their child's successful surgery, continued to have endless concerns about possible future issues, inhibiting them from achieving complete calmness. This contrasts with the findings of the Wei et al. study, where parents reported achieving a sense of fulfillment during child care (7). This disparity may stem from differences in parental support and cultural norms regarding the role of parents in different countries. In Iran, parents, even when their children are adults, consider themselves responsible for their children’s lives.
The findings indicate that having faith and true belief in God, and trusting in spiritual powers, were among the comforting factors observed in all mothers at every stage of surgery. Parents' coping strategies heavily rely on their religious beliefs as a source of meaning and comfort (19). Wasserman et al. argue that when stressful situations are beyond one's control, religious coping is more effective than non-religious coping (26). Javedanpour et al. also emphasize the effect of spiritual care and the desire to receive it, believing it greatly aids these parents (27). It is possible to greatly reduce mothers' discomfort and stress by creating an area near the operating room for worship, having a clergyman available to talk to parents when the child is in surgery, providing training and preparation for postoperative care at home, establishing a telephone line for answering parents' questions after discharge, offering home care services, and providing educational brochures about home-based care.
The strength of this research lies in conducting separate interviews at three stages: pre-surgery, during surgery, and post-surgery, with each participant. This approach minimized the likelihood of mothers forgetting their experiences and helped to capture their experiences comprehensively throughout the different stages of surgery and post-discharge. However, a limitation of the research was the absence of fathers in the study. Since fathers are not the primary caregivers of children undergoing CHD surgery in pediatric wards, this limits the generalizability of the results for fathers.
5.1. Conclusions
The shock induced by CHD and the challenges of caring for the child made facing surgery a nightmare for the mothers. Overcoming the surgical nightmare and achieving relative calm became possible through seeking information and spirituality, although concerns for the child's uncertain future persisted. It is recommended that care provision focus on preparing and empowering mothers before surgery. Healthcare team members can also enhance mothers' adaptation and resilience by adopting reassuring behavior, providing spiritual care, and guiding the social network to support them effectively.