1. Background
In health systems, nurses are the main element of care in the treatment team. Nurses have always faced a high workload, given the nature of the job and the pressures caused by the high job demands. Workload includes both physical and mental elements. A systematic review has already shown that nurses present high levels of mental workload (MWL) (1, 2). In this regard, the results of the meta-analysis study have shown that the highest MWL was reported in China (82.26 ± 14.82), Iran (75.18 ± 20.01), and America (71.40 ± 13.62), respectively (3).
An increase in MWL occurs when a person has many tasks to process and carry out in a certain period. If the job demands exceed the individual's capacity and ability and the individual cannot face the new conditions with proper strategies, their performance and efficiency could decrease (4). Indeed, a high MWL can affect people's attention and physical skills and increase errors in performing tasks. Fatigue and excessive workload could be the potential reasons for medical errors (5). Thus, one of the major factors significantly increasing human error is the high MWL, which finally leaves adverse effects on the efficiency of people in the workplace (6, 7). Moreover, according to the study on nurses, people's work engagement negatively correlates with excessive MWL (8). Hence, MWL is a significant variable for understanding people's performance in work environments (5). Moreover, some studies have indicated that a high MWL in people results in physical fatigue and emotional exhaustion and could increase stress and burnout (9-11). Therefore, in sensitive working conditions, especially when there is time pressure and stress, such as the working conditions of nurses, paying attention to factors affecting MWL can play an important role in reducing errors and MWL.
The MWL is a multidimensional concept and is associated with the nature of a task, the abilities of the individual, and the characteristics of the environment. Hence, the MWL is affected by the cognitive demands of tasks and other factors like working conditions and motivation levels (8, 9). Epidemiological studies have shown that variables such as age, sex, and work experience are demographic risk factors associated with MWL (4, 5). A review of demographic risk factors in this occupation specifies that age, work experience, and having no children are some of the individual factors that affect the MWL (1). Therefore, for this study, we hypothesized that demographic characteristics affect MWL (Hypothesis 1).
One of the most important factors affecting MWL is the psychosocial factors of the work environment. Psychosocial factors are actually employees' perceptual experiences of the quality of work environments. Factors such as stress, emotional needs, burnout, job satisfaction, and the quality of leadership are known as the most important psychosocial risk factors (10, 11). The results of a study conducted on nurses in intensive care units have shown that 57% of the participants perceived high levels of exposure to psychosocial risk factors, and psychosocial factors explained 10.36% of MWL (12). Also, the results of a study conducted on emergency nurses showed that job satisfaction was significantly related to mental demand and frustration. The results of this study showed that the mean scores for mental demand and frustration increased significantly in participants with low job satisfaction (13). In this regard, the results of the study conducted on healthcare workers have shown that MWL is inversely related to job satisfaction and job control (11). Also, the results of a study conducted on MWL among nurses have shown that social support was significantly negatively associated with the MWL in nurses (12). Psychosocial factors at work are among the main triggers of MWL; however, studies carried out in this field of health and also in the field of nursing on working conditions are scarce and focused on some psychosocial factors. Given this evidence, we examined the relationship between all psychosocial factors and MWL (Hypothesis 2).
2. Objectives
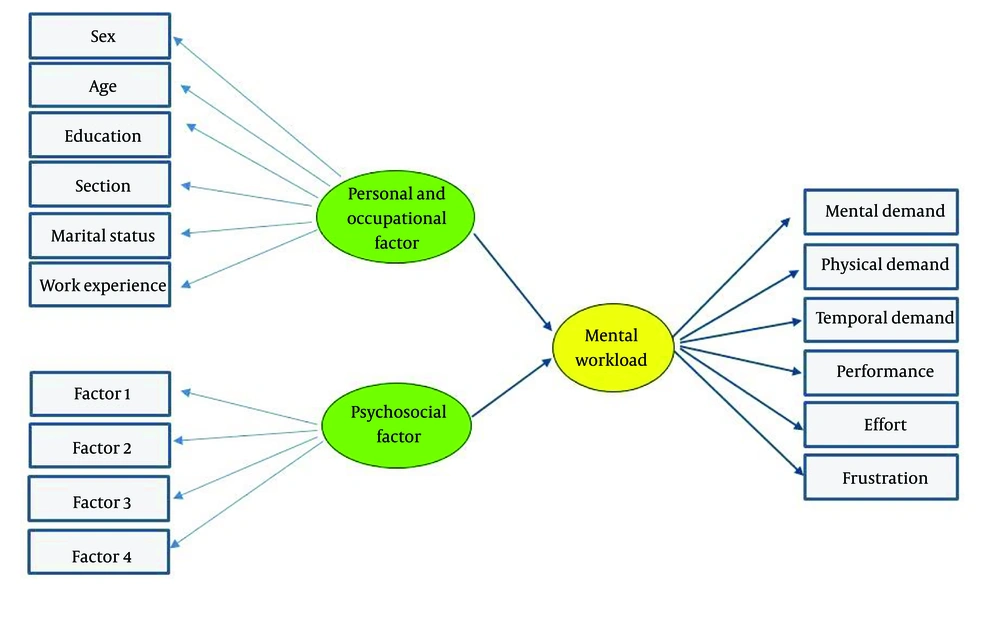
The study aims to (1) determine the MWL of nurses; (2) evaluate and identify psychosocial and demographic factors that affect MWL; and (3) present a conceptual model to predict the factors that affect the MWL (Figure 1).
3. Methods
3.1. Participants
This cross-sectional descriptive-analytical study was conducted in 2021. Participants were 234 nurses from a teaching hospital in Ilam, Iran. The sample size was calculated by considering a power of 95% and a probability of type I error of 0.05. According to a previous study and Equation 1, the required sample size was 234 people (13). The criteria for inclusion were: (a) work experience of more than 1 year, and (b) not suffering from chronic diseases or psychological problems.
3.2. Measurements
3.2.1. NASA Task Load Index
NASA Task Load Index (NASA-TLX) is a multidimensional subjective MWL evaluation method. In this method, the overall workload score is obtained according to the weighted average of 6 subscales of workload. The subscales examined in this method were mental demand, physical demand, temporal demand, performance, effort, and frustration (Table 1). In this questionnaire, each field of activity is divided into 100 points with 5-point steps. The overall workload score was calculated according to the weighted average of ratings in 6 dimensions. The NASA TLX interpretation categorizes workload score values of 0 - 9 as low, 10 - 29 as medium, 30 - 49 as somewhat high, 50 - 79 as high, and 80 - 100 as very high (14). The validity and reliability of the Persian version of NASA-TLX have been examined in a previous study (13).
| Dimension | Description |
|---|---|
| Mental demand | How much mental and perceptual activity was required (e.g., thinking, deciding, calculating, remembering, looking, searching, etc.)? Was the task easy or demanding, simple or complex, exacting, or forgiving? |
| Physical demand | How much physical activity was required (e.g., turning, controlling, activating, etc.)? Was the task easy or demanding, slow or brisk, slack or strenuous, restful or laborious? |
| Temporal demand | How much time pressure did you feel due to the rate or pace at which the tasks or task elements occurred? Was the pace slow and leisurely or rapid and frantic? |
| Performance | How successful do you think you were in accomplishing the goals of the task set by the experimenter (or yourself)? How satisfied were you with your performance in accomplishing these goals? |
| Effort | How hard did you have to work (mentally and physically) to accomplish your level of performance? |
| Frustration | Level How insecure, discouraged, irritated, stressed, and annoyed versus secure, gratified, content, relaxed, and complacent did you feel during the task? |
NASA-TLX Scales
3.2.2. Copenhagen Psychosocial Questionnaire
Copenhagen Psychosocial Questionnaire (COPSOQ) is one of the most complete and reliable questionnaires that examine psychosocial factors. In this study, the second version of COPSOQ with 4 main factors and 16 subfactors was used. The respondents to the COPSOQ are asked to respond to the questions using items on a 5-point scale, most of which are as follows: A = Always, B = Often, C = Sometimes, D = Seldom, and E = Never/Hardly, or as A = To a very large extent, B = To a large extent, C = Somewhat, D = To a small extent, and E = To a very small extent. Based on the subjects' ratings, each item (scores A to E) scored 0, 25, 50, 75, and 100, respectively, and the average score of the items on each of the factors determined the score of that factor. Giving a lower rate to each of the factors indicates better and more ergonomic psychosocial conditions of that work environment (15). In this study, the Persian version of the COPSOQ was used (16).
3.2.3. Demographic Form
Demographic information of the individuals, such as age, gender, marital status, work history, work department, degree, and field of study, was collected through a form.
3.2.4. General Health Questionnaire-12
The questionnaire is the short version of Goldberg's 60-question general health questionnaire, measuring a person's mental health in 12 items. Each item is scored on a four-point scale (less than usual, no more than usual, rather more than usual, or much more than usual). The questionnaire questions examine the mental state of the person in the last four weeks (one month). The positive items scored from 0 to 3, and the negative ones from 3 to 0. Total scores range from 0 to 36, with a score of 11 or 12 considered typical, scores > 15 suggesting evidence of distress, and scores > 20 considered severe problems with psychological distress (17). In this study, the Persian version of the General Health Questionnaire-12 (GHQ-12) was used (18).
3.3. Data Analysis
The data were analyzed using SPSS version 23 and LISREL 8.8. The correlations between demographic factors, psychosocial factors, and MWL were explored using correlation analysis. Structural equation modeling (SEM) was used to identify causal relationships between variables. Psychosocial and demographic factors were considered independent variables, and MWL was considered dependent in this study. In SEM, the fit of the model was examined after estimating the model parameters and prior to interpreting them. The goodness-of-fit index, X2/df < 2, GFI, CFI, NNFI, NFI > 0.90, and RMSEA < 0.08 were considered to indicate an adequate model fit.
4. Results
The mean general health score of the participants in the study was 1.36 ± 1.02, and the maximum GHQ score was 3. Thus, considering the cut-off point of the GHQ questionnaire, all the participants in the study met the inclusion criteria. The mean age of the nurses participating in the study was 36.62 ± 8.25. The mean work experience of the participants was 8.86 ± 4.89 (Table 2).
| Variables | Values |
|---|---|
| Age (y) | 36.62 ± 8.25 |
| Work experience (y) | 8.86 ± 4.89 |
| Height (cm) | 169.70 ± 10.35 |
| Weight (kg) | 69.99 ± 11.12 |
| Gender | |
| Female | 114 (48.7) |
| Male | 120 (51.3) |
| Marital status | |
| Single | 57 (24.4) |
| Married | 172 (73.5) |
| Divorced | 5 (2.1) |
| Educational level | |
| Bachelor degree | 177 (75.6) |
| Master degree | 47 (20.1) |
| PhD | 10 (4.3) |
Demographic Information of the Participants (n = 234) a
4.1. Psychosocial Factors
The mean score of the total psychosocial factors of the subjects examined was specified as 1.87. Psychosocial factors 2 (general health, burnout, work-family conflict, emotional demands, stress) and 1 [quality of leadership, social support from supervisor, recognition (reward), justice, trust regarding management, predictability] had the highest scores, respectively (Table 3).
| Factors | Mean ± SD |
|---|---|
| Factor 1 (quality of leadership, social support from supervisor, recognition, justice, trust regarding management, predictability) | 1.76 ± 0.44 |
| Factor 2 (general health, burnout, work-family conflict, emotional demands, exhaustion, stress) | 1.85 ± 0.27 |
| Factor 3 (meaning of work, commitment to the workplace, influence, role clarity) | 1.57 ± 0.27 |
| Factor 4 (offensive behavior) | 2.54 ± 0.2 |
| Total score | 1.87 ± 0.34 |
Mean and Standard Deviation of Psychosocial Factors (COPSQ) (n = 234)
4.2. Mental Workload
The mean score of the overall MWL of the subjects examined was determined as 70.09 ± 9.51. The analysis of the dimensions of MWL indicated that the mean scores of efforts (71.41 ± 8.93), frustration level (71.38 ± 5.50), and physical demand (70.74 ± 7.00), respectively, in the group of nurses examined were higher than other dimensions of MWL (Table 4).
| NASA-TLX | Mean ± SD |
|---|---|
| Mental demand | 69.68 ± 6.24 |
| Physical demand | 70.74 ± 7.00 |
| Temporal demand | 68.95 ± 7.17 |
| Effort | 71.41 ± 5.93 |
| Performance | 69.70 ± 7.35 |
| Frustration | 71.38 ± 8.50 |
| Overall work load | 70.09 ± 2.51 |
Mean and Standard Deviation of Mental Workload Subscales (n = 234)
4.3. Correlation Analysis
The results of the correlation of MWL with psychosocial and demographic factors showed that MWL has a positive correlation with factor 3 (meaning of work, Commitment to the workplace, Influence, Role clarity), factor 1 (quality of leadership, Social support from supervisor, Recognition (reward), Justice, Trust regarding management, Predictability), factor 4 (offensive behavior), and the total score of psychosocial factors (P < 0.05) (Table 5).
| Variables | Factor 1 | Factor 2 | Factor 3 | Factor 4 | Total Score (COPSOQ) |
|---|---|---|---|---|---|
| Mental demand | 0.311* | 0.180** | 0.248* | 0.143 | 0.318* |
| Physical demand | 0.164 | 0.264* | 0.232* | 0.083 | 0.110 |
| Temporal demand | 0.180 | 0.028 | 0.194** | 0.167 | 0.906 |
| Effort | 0.257* | 0.030 | 0.188** | -0.146 | 0.206** |
| Performance | 0.198** | -0.250* | 0.324* | 0.283* | 0.227* |
| Frustration | 0.268* | 0.158 | 0.269* | 0.153 | 0.313* |
| Overall work load | 0.303* | 0.034 | 0.334* | 0.299* | 0.312* |
Mental Workload (NASA-TLX) Subscales and Psychosocial Factors (n = 234) a
4.4. Structural Model
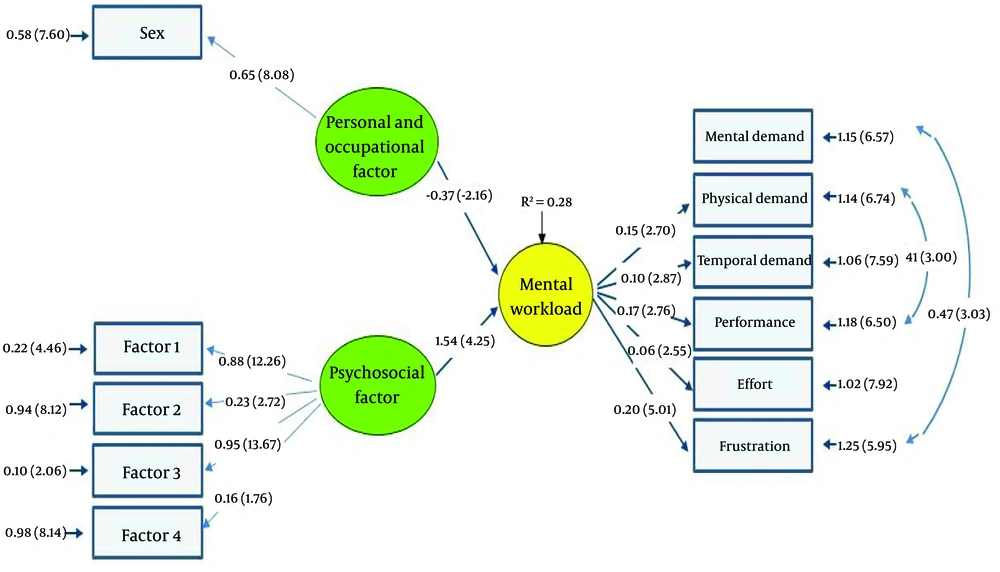
Figure 2 shows the path diagram with standardized factor loadings (numbers outside the parentheses between the latent and visible variables and endogenous and exogenous latent variables), errors (numbers outside the parentheses of the visible variables), and t values (numbers in parentheses) of the model. As Figure 2 shows, some variables show a relatively high correlation. R² = 0.28 is the relative value of the dependent or endogenous variable variance explained by the exogenous variable. The t values indicate that some loaded factors are significant at the 95% confidence interval (the absolute value of t values is greater than 1.96) (Figure 2). There was a significant relationship between individual and psychosocial factors with the MWL, and these factors in interaction had a 28% ability to predict MWL in the presented SEM (Figure 2).
4.5. Validation of the Research Model
As Table 6 shows, most of the fit indices for measuring the fit of the whole model show a good model fit, compatibility, and agreement of the whole model with experimental data.
| Model Fit Indices | X2 | X2/df | AGFI | GFI | NFI | NNFI | CFI | RMSEA |
|---|---|---|---|---|---|---|---|---|
| Cutoff values | > 0.05 | < 3 or 2 < | > 0.9 or 0.8 | > 0.9 | > 0.9 | > 0.9 | > 0.9 | < 0.08 |
| SEM | 0.08 | 2.88 | 0.86 | 0.85 | 0.95 | 0.93 | 0.94 | 0.06 |
The Model Fit Indices for the Effect of Psychosocial and Personal Factors on Mental Work Load
5. Discussion
The study was carried out to predict the psychosocial factors affecting the MWL of nurses based on a structural model. The study revealed that psychosocial factors, as well as demographic variables in interaction with each other, can predict 28% of the MWL of nurses. The study results showed that the mean NASA-TLX score of the nurses who participated was 70.09 ± 9.51. Similarly, the results of a study conducted by Nasirizad Moghadam et al. among ICU nurses in Iran showed that the mean nurses' MWL was 70.21 (19). Regarding this, the study carried out by Li et al. on the MWL of nurses indicated that the mean MWL in 56.96% of the nurses studied was 73.59 ± 8.86, which was in the range of high workload (20). Moreover, the results of a similar study conducted by Shan et al. have indicated that the MWL of 62.9% of the nurses was in the high workload perception group (21). The results of the systematic review study conducted by Yuan et al. have also highlighted that nurses experience high MWL and need urgent interventions to reduce MWL (2). Overall, studies have revealed that nurses experience more workload than other healthcare workers, including the time needed to carry out direct and indirect care (22, 23).
Studying the NASA-TLX dimensions in the present study indicated that the mean score of the effort dimension was higher and more challenging than other dimensions. Moreover, the mean score of frustration level and physical demand were higher than other dimensions of MWL, respectively. Consistent with the present study, Li et al. reported that a relatively high score was obtained in the subscales of “effort,” “physical demand,” and “mental demand” among the nurses examined (20). In this line, Sonmez et al. also reported that the highest mean score of the MWL subscales were in mental demand, performance, and effort, respectively (24). In the same way, the results of a study conducted by Bazazan et al. also showed that the effort is more problematic than other dimensions (13). The results of the current study indicated that the level of frustration is another important dimension of MWL. Regarding this, the findings of a study conducted by Ebrahimi et al. have also shown that frustration is the second subscale of MWL with the highest score in evaluating nurses' MWL (25). In this regard, the results of a study conducted by Bazazan et al. also showed that frustration is one of the important dimensions of workload and the mean scores for frustration increased significantly in participants with low job satisfaction scores (13).
The present study results indicated that MWL significantly correlates with psychosocial factors. Thus, the MWL could be reduced by enhancing the identified factors such as quality of leadership, social support from supervisors, recognition (reward), justice, predictability, role clarity, general health, and reducing burnout, stress, work-family conflict, and offensive behavior. The results of SEM analysis in the study indicated that the key psychosocial factors affecting MWL were factor 1 (quality of leadership, social support from supervisors, recognition (reward), justice, trust regarding management, predictability) and factor 3 (meaning of work, commitment to the workplace, influence, role clarity). In this regard, Ceballos-Vásquez et al. examined psychosocial factors and MWL among nurses and reported a negative correlation between psychosocial factors and MWL (26). Studies have shown that nurses with higher levels of coworker and manager support report less daily workload (26, 27). In this line, Al-Hakim et al. also illustrate the critical role of perceived organizational support on nurses' workload and job satisfaction (28). In this regard, in Afshari et al.'s study, the quality of leadership and social support have been mentioned as important psychosocial risk factors identified from the point of view of nurses (29). Moreover, the results of García-Iglesias et al. indicated that social support and quality of leadership are important psychosocial factors (30). Concerning this, Álvarez et al. revealed that social support and quality of leadership are among the psychosocial factors that affect the workload (31). Indeed, the presence of role clarity, autonomy, and supervisor support in the work environment of the nurses could help nurses control and manage workload and thus reduce workload. The results of Cai et al. showed that the leadership style and the logical arrangement of tasks could moderate nurses' workload and prevent the negative effects of high workload (32). Changes in leadership style, influence, and reduction of concentration are the factors that reduce workload and increase motivation and performance from the point of view of nurses (33). In this regard, the results of a study conducted by Cho et al. showed that changing the leadership style and increasing nursing teamwork is important to monitor and modify high workload to protect nurses from elevated fatigue (34). Hence, identifying the psychosocial factors affecting the MWL of nurses could be useful in determining strategies and planning to reduce the MWL and increase productivity.
Besides psychosocial factors, the model presented in the study revealed that gender is one of the demographic factors that affect the MWL. In this regard, studies have shown a significant relationship between gender and MWL (1, 35). Similarly, Bagheri Hosseinabadi et al. also concluded that gender may be effective in increasing the MWL of nurses (4). Hence, identifying individual factors that affect MWL could control and reduce the MWL of the nurses.
5.1. Strengths and Limitations
The present study examined MWL and psychosocial factors using a self-reporting questionnaire. Thus, there could be bias in the study results, and efforts were made to solve this limitation by fully explaining the questions of the questionnaires and the objectives of the study to the participants, which increased the accuracy of answering the questions. Among the other limitations of the study is its being conducted in a teaching hospital. As working conditions in private hospitals vary from teaching hospitals, it is suggested that a study should be conducted to examine psychosocial factors that affect MWL in private hospitals to generalize the results to all hospitals.
5.2. Conclusions
The study findings indicated that nurses' workload was relatively high. Studying the mean scores of the workload scales showed that the effort, frustration, and physical demand scores, respectively, have the highest values relative to other dimensions of MWL. According to the study results, psychosocial factors, including the quality of leadership, social support from supervisors, recognition (reward), justice, trust regarding management, predictability, meaning of work, commitment to the workplace, influence, and role clarity, as well as the demographic factor of gender, were among the factors affecting the MWL of nurses. Thus, the MWL of nurses could be reduced, especially by managing and enhancing the effective psychosocial factors.