1. Background
Today's modern healthcare has increasingly recognized the pivotal role of informal caregivers in supporting patients both within and outside of formal healthcare systems (1). Informal caregivers are acknowledged as indispensable resources for health systems (2). Aligned with this approach, holistic nursing, as a contemporary healthcare paradigm, aims to enhance patient outcomes and ensure patient efficacy, support, and quality of life through engagement with patients' families (3). Notably, the realm of cancer care stands out as a critical context for the involvement of informal caregivers (4).
Caregivers of cancer patients require support to navigate the spectrum of hospital treatments and continue care at home following discharge (5). Beyond providing medical assistance at home, families of cancer patients may assist with daily life activities, manage patients' medications, arrange healthcare visits (6), and aid patients in adjusting to the new realities of their lives (7). Moreover, caregivers are often involved in making a myriad of healthcare decisions from the time of diagnosis to end-of-life care. These decisions encompass choosing treatment priorities, considering surgeries, transitioning between care settings and providers, engaging in self-care practices, navigating insurance coverage, and seeking palliative care towards the end of life (8, 9).
New caregivers often face numerous challenges (1), especially when it comes to addressing their emotional and informational needs to effectively fulfill their caregiving roles. These responsibilities can pose risks to their own health and well-being, particularly for those who are new to caregiving (10). They commonly encounter challenges such as anxiety (11, 12), fear of disease progression (11), uncertainty, financial constraints, time management issues, personal health concerns, and sleep disturbances. Recognizing the psychological and emotional strains experienced by informal caregivers, researchers advocate for their preparation through emotional support and targeted information provision (13-15). Additionally, advancements in medical science have underscored the importance of caregivers receiving training to deliver complex levels of care (16).
Despite the significance of caregivers being adequately prepared to administer home-based healthcare and manage patients' health issues, researchers suggest that informal caregivers often lack the necessary training to acquire the knowledge and skills essential for effective patient care and support in cancer settings (10). Alternatively, they may experience information overload, where the amount of information provided exceeds their capacity to process it effectively, or encounter a dearth of resources for optimal learning, resulting in cancer information overload (17). Conversely, some caregivers may lack the motivation to seek information. Research findings indicate that caregivers express the need for mandatory participation in face-to-face or online classes to enhance their motivation for learning (18).
Given that client health education constitutes a crucial component of holistic nursing care, it is imperative for nurses to devise effective strategies to address the educational needs of cancer caregivers. However, limited studies have been conducted in this area.
2. Objectives
This study aimed to compare the impact of providing structured health information versus needs-based education for caregivers on the anxiety levels of family members of cancer patients.
3. Methods
3.1. Study Design
This randomized controlled clinical trial was conducted at cancer centers affiliated with Rafsanjan University of Medical Sciences, located in Rafsanjan, Kerman province, Iran, from December 2022 to May 2023.
Upon approval of the research project, sampling commenced. One of the researchers, a nurse, visited the cancer centers, explained the study's objectives, and obtained informed written consent from eligible participants.
3.2. Study Participants and Sampling
Participants included family members of cancer patients admitted to cancer centers affiliated with Rafsanjan University of Medical Sciences within six months of their cancer diagnosis. Initially, purposeful sampling was conducted based on predefined inclusion criteria. Subsequently, eligible participants were assigned to two study groups (A: Education based on family members' needs, B: Structured education) using the random minimization method. This allocation was based on educational background (diploma or academia) and baseline anxiety intensity categories (moderate or severe). Randomization units were sequentially enrolled, with the first sample in each category and study group determined by random drawing using sealed envelopes. Subsequent samples with matching characteristics were assigned to the remaining group within the same category. This process continued until the desired sample size was reached.
3.3. Inclusion Criteria
Participants had to be above 18 years old, first-degree family members of the patient (spouse, father, mother, child, siblings), possess at least a high school diploma, demonstrate sufficient cognitive ability to learn, comprehend, and communicate, not have a known psychopathy or substance abuse history, not have experienced adverse events in the past six months, receive a cancer diagnosis within the last six months, and obtain a moderate to high anxiety score on the Spielberger State Anxiety Inventory.
3.4. Exclusion Criteria
Exclusion criteria included reluctance to participate in the study and the occurrence of any acute conditions.
The sample size was calculated to be 80 family members of cancer patients, with 40 participants in each group. This calculation was based on the following formula, with a standard deviation of 4.5, significance level of 0.05, power of 90%, and an effect size of 3.3 in terms of the minimum difference in means changes between groups (19):
3.5. Intervention
After allocating samples to groups, family members in group A received cancer-related health information tailored to their needs and questions. For group B, information was provided in a structured format based on a pre-prepared protocol in a booklet. This information covered various topics such as the nature of cancer, diagnostic and treatment methods, disease progression and consequences, treatment complications, symptoms of disease recurrence, acceptance of the disease by the patient and family, recognition of symptoms requiring immediate intervention, psychological changes in response to cancer, emotional support, proper patient interaction, nutrition, home rehabilitation, and resumption of normal activities.
Since family members had varying information needs, the content provided in group A was individualized based on their questions, with the amount and type of information determined by the nurse researcher in response to these questions. The intervention period for group A ended when all family members' questions were addressed, while for group B, it concluded when all the information outlined in the booklet was provided.
3.6. Data Collection Tool and Technique
The data collection tool consisted of two parts: The first part was demographic information, and the second part was the Spielberger State Anxiety Inventory. Demographic characteristics questionnaire of family members included: Age, sex, marital status, education, and family relationship.
The Spielberger State-Trait Anxiety Inventory (STAI) scale includes 20 items that measure a person's feelings at the time of answering, on a 5-point Likert scale (never score 1, rarely score 2, sometimes score 3, most of the time score 4, almost always score 5). The validity of the scale has been reported with a Cronbach's alpha coefficient of 0.92 and a reliability coefficient of 0.73 to 0.86. The Spielberger's standard questionnaire was standardized on 600 subjects in Mashhad in Mahram's research in 2012. The reliability of the test has been calculated as 0.9451 through Cronbach's alpha formula. Also, for the criteria group separately, this reliability has been calculated and its value is reported as 0.9418. The standard error of the test measurement was calculated as 4.643. Additionally, the correlation of the observed scores with the true score equals 0.972 and with the error scores was calculated to be equal to 0.234 (20).
Measurements were performed at two times. The first measurement was before entering the study as a baseline, and the second measurement was after completing the intervention. Data collection was conducted by the researcher's colleague who was blind to the allocation of samples in the study groups, through face-to-face interviews.
3.7. Statistical Analysis
Data were analyzed using SPSS software version 22, by Shapiro and Wilk statistical tests (to check the normality of quantitative data distribution), chi-square and Fisher's exact test (to compare proportions), Paired Samples T-test (to compare within groups), and independent t-test (for comparison between groups) at a significance level of 0.05.
3.8. Ethical Considerations
In this study, ethical issues in research such as the approval of a research project in the ethics committee in biomedical research (with the code IR.RUMS.REC.1401.092) and obtaining the IRCT code from the Iranian Clinical Trials (IRCT20230611058452N1), obtaining informed consent, freedom to leave the study, confidentiality, and assurance to the participants that their participation or non-participation in the study did not change the quality of patient care, were considered.
4. Results
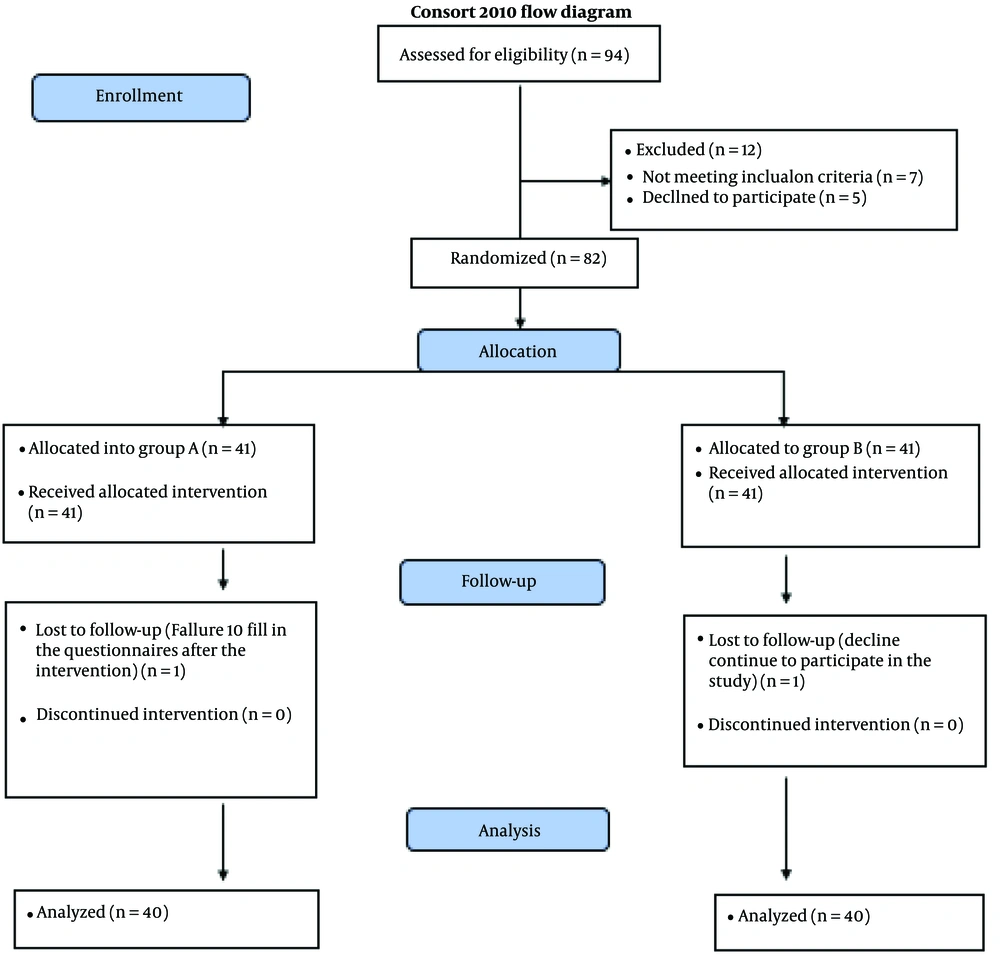
A total of 94 family members who were caregivers of cancer patients were assessed for eligibility. Eighty-two participants entered the study (41 in group A and 41 in group B). One family member was excluded from group A due to failure to fill in the questionnaires after the intervention, and one from group B due to declining to continue participation in the study. Finally, data from 80 cancer family members were analyzed (Figure 1).
The results of the Shapiro-Wilk test showed that all of the quantitative variables had a normal distribution. The data analysis indicated that the mean and standard deviation of the patients and their family members' ages were 58.70 ± 14.00 and 40.45 ± 12.20, respectively. The minimum and maximum ages of family members were 18 and 66 years. The diagnoses of 15 (18.8%) patients were leukemia or lymphoma, 8 (10%) had brain cancer, 14 (17.5%) had breast cancer, 16 (20%) had gastrointestinal cancer, and 27 (33.8%) had other types of cancer.
The comparison of demographic characteristics between the two groups showed that the mean ± SD of the caregiver's age in group A was 39.30 ± 11.7 and in group B was 41.60 ± 12.66. The independent t-test showed no statistically significant difference between the caregiver's ages (P = 0.403). Additionally, the two groups were similar in terms of patient age (P = 0.375) and disease duration (P = 0.736). The comparison of other important demographic characteristics between the two groups is shown in Table 1.
| Group A (n = 36) | Group B (n = 36) | P-Value | |
|---|---|---|---|
| Gender | 0.359 b | ||
| Male | 18 (45) | 13 (32.5) | |
| Female | 22 (62.5) | 27 (67.5) | |
| Education | 1.00 b | ||
| Diploma | 30 (75) | 29 (72.5) | |
| Academic | 10 (25) | 11 (27.5) | |
| Marital status | 0.612 b | ||
| Single | 12 (30) | 9 (22.5) | |
| Married | 28 (70) | 31 (77.5) | |
| Family relationship | 0.253 c | ||
| Child | 26 (65) | 30 (50) | |
| Parents | 1 (2.5) | 1 (2.5) | |
| Spouse | 11 (27.5) | 12 (30) | |
| Sister/brother | 2 (5) | 7 (17.50) |
a Values are expressed as No. (%).
b Chi-squared test.
c Fisher’s exact test.
In the inter-group comparison, the results of the independent samples t-test showed that there were no statistically significant differences between the two groups at baseline (P = 0.872). However, the results of the independent samples t-test showed a statistically significant difference in the STAI score between the study groups after the intervention (P = 0.001). Also, a statistically significant difference was observed in comparing the mean changes of the STAI score between the study groups (P = 0.001).
In the intra-group comparison of the STAI score before and after intervention in group A, the results of the Paired Samples T-test showed that the change in the STAI score was statistically significant (P = 0.001, 95% CI: 7.32, 10.82). For group B, the results of the Paired Samples T-test showed that the mean changes ± SD of the STAI score were statistically significant (P = 0.006, 95% CI: 0.705, 3.94) (Table 2).
a Values are expressed as mean ± SD.
b Independent samples t-test.
c Paired Samples T-test.
5. Discussion
The results of the study indicated a decrease in the anxiety scores of cancer family members after receiving education, either deemed necessary from their perspective or recognized as necessary by nurses. However, when information was provided based on the family members' needs and questions, the anxiety scores decreased more than when based on nurses' diagnosis. This suggests that individualized health information, which offers proper flexibility and is tailored to the client's needs, prevents information overload. Clients receive content that aligns with their perceived needs, facilitating better understanding and thereby leading to lower anxiety levels.
A review of the literature revealed that in most studies, researchers focus on the effect of the education method on patients' and family members' anxiety rather than adjusting the education content based on the clients' needs. Various methods of providing information on patients' and their family members' anxiety have been tested in numerous studies, yielding contradictory results (21, 22). For instance, Peters et al. conducted a study comparing the impact of standard one-on-one verbal education by nurses with a combination of this method and DVD-structured education. They concluded that there was no statistical difference in family members' anxiety (23). It's noteworthy that the above study aimed to compare the anxiety of family members of patients with leukemia and lymphoma using two different education methods with the same content. In contrast, the current study compared family members' anxiety scores based on receiving client or nurse-diagnosed content with the same verbal one-on-one education.
In other studies, researchers have explored the impact of various training methods on the anxiety levels of patients and their family members. For instance, in Hauken et al.'s study in Norway, a psychological education program was unable to reduce the anxiety levels of children with parents diagnosed with cancer (24). Similarly, in Li et al.'s study in China, the application of a comprehensive education course did not reduce the anxiety levels of patients with breast cancer (25). Additionally, in Hendrix et al.'s study, the implementation of an advanced training program for cancer caregivers of hospitalized patients resulted in short-term improvements in stress, readiness, and self-efficacy for symptom management, but did not significantly impact the psychological well-being of caregivers (26). The researchers attributed these outcomes to the lack of repetition of the intervention and the diverse needs of informal caregivers post-discharge from the hospital.
However, in Gholamian et al.'s study in Iran, the implementation of a collaborative self-care training program involving mothers of children with cancer, psychologists, and oncology nurses significantly reduced the anxiety levels of these mothers (27). It's important to note that collaborative care training programs are highly comprehensive and tailored to the specific needs and circumstances of patients and their families. The reduction in mothers' anxiety may be attributed to their participation in numerous meetings with the patient and receiving specialized emotional support from the collaborative care team.
Similarly, in Abdullahzadeh and Khosravi's study, a family needs-based program was effective in reducing the stress, anxiety, and depression of family caregivers of leukemia patients (28). These findings, akin to those of the present study, underscore that focusing on the concerns of cancer patient caregivers and personalizing interventions leads to improved nursing care quality and better psychological outcomes.
5.1. Limitations and Recommendations
Despite its strengths, such as the precise design and control of confounding factors, including the selection of first-degree family members directly caring for the patient, matching the education level of family members in both groups, and ensuring a six-month period post-cancer diagnosis to mitigate emotional imbalances related to the diagnosis, this study had limitations. These included single-session training and the lack of long-term follow-up of participants. More robust studies are needed to complement existing evidence and provide deeper insights into tailoring educational content in a manner that alleviates anxiety without compromising clients' needs.
5.2. Conclusions
Providing educational content based on clients' needs and requests or based on nurses' diagnosed needs through one-on-one verbal communication can reduce anxiety among family members of cancer patients. However, family members who received tailored educational content according to their needs reported lower levels of anxiety.