1. Context
Chronic kidney disease (CKD) is characterized by the progressive and irreversible destruction of the kidneys, which, like other chronic diseases, affects all aspects of a patient's life and has numerous physical and psychological consequences. Dialysis and kidney transplantation are the primary treatment options for this condition, but dialysis itself is a highly stressful process that can lead to significant psychological stress and a host of psychosocial problems (1). The prevalence of end-stage renal disease (ESRD) is increasing, with cases doubling every seven years (2). In Iran, approximately 38,000 patients undergo dialysis each year, and this number was projected to double by 2020 (3).
The annual cost of treating CKD patients is substantial. In the United States, total Medicare expenditures for these patients exceeded $12.36 billion in 2000, and this figure increased by 11% to $17 billion in 2002 (4). The overall medical costs per patient per year, including transportation, visits, hospitalization, and hemodialysis, exceed $75,000 in the United States (5). In addition to the financial burden, these patients experience numerous side effects due to the disease process and treatment regimen. They face various psychological stresses, which can lead to mental health disturbances, including behavioral changes such as depression, isolation, and hallucinations due to the inability to cope with these challenges (6).
Depression is the fourth leading cause of disability worldwide and one of the most common mental disorders in CKD patients (6). Drayer et al. found that 36.7% of hemodialysis patients suffer from mood disorders, with 9.6% experiencing severe depression and 27.1% experiencing mild depression (7). Depression is a disorder characterized by a lack of energy and interest, feelings of guilt, difficulty concentrating, lack of appetite, and recurrent thoughts of death or suicide. It also affects an individual's activity levels, cognitive abilities, speech, and other biological functions. Moreover, depression can lead to various physical complications, including fatigue, insomnia, decreased libido, diarrhea, and constipation (8, 9). The prevalence of depression among hemodialysis patients in Iran ranges from 50% to 80%, and anxiety affects 20% to 60% of these patients (10). Overall, 20% to 30% of dialysis patients suffer from depression (11, 12).
Depression in hemodialysis patients can increase the risk of suicide, with a prevalence of suicide among depressed dialysis patients estimated at 15%, higher in men and young people than in other demographics. Depression may be more prevalent among dialysis patients than in those with cancer, congestive heart failure, or other severe chronic diseases (13, 14). Depression in these patients is associated with a range of adverse outcomes, including increased fatigue, lower performance status, decreased physical activity, and reduced quality of life (15, 16). Counseling has been shown to be effective in reducing psychological symptoms in patients undergoing hemodialysis (17, 18).
Given the importance of this issue, various questionnaires have been developed in recent years to measure the prevalence of depression. One of the most well-known and widely used instruments is the Beck Depression Inventory (BDI), first developed in 1961 by Beck et al. (19). The BDI is a 21-item, multiple-choice inventory employing Guttman scaling, designed to assess the level of depression in adults. Each item is scored from 0 to 3 points, with a total score range of 0 to 63. The scale was developed as a quantitative measure of depression and was not originally intended as a diagnostic instrument. Suggested score ranges are 10 - 19 for mild depression, 20 - 30 for moderate to severe depression, and 31 or higher for severe depression (20).
Numerous studies have been conducted on depression among dialysis patients in Iran using the Beck questionnaire, reporting various prevalence rates. For instance, the prevalence of depression among these patients was estimated at approximately 56.7% by Mogharab in 2011 in Birjand (21) and around 70% by Afshar et al. in 2010 in Tehran (22). However, these studies do not provide a comprehensive picture of the issue. Aggregating the results of studies on the prevalence of depression among dialysis patients is crucial for evidence-based decision-making by health managers and policymakers.
2. Objectives
Therefore, the present study aimed to conduct a systematic review and meta-analysis of the prevalence of depression among dialysis patients in Iran.
3. Methods
This study was a systematic review and meta-analysis conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines (23).
3.1. Search Strategy
In this study, articles published in English and Persian up until April 19, 2024, were included. The focus was on studies investigating the prevalence of depression among dialysis patients in Iran, without any time restrictions. The following databases were searched: Web of Science, PubMed, Scopus, PsycINFO, Scientific Information Database (SID), MagIran, and the Google Scholar search engine. The search was conducted using the following keywords: Prevalence, depression AND hemodialysis OR renal replacement therapy OR depressive disorders OR end-stage renal disease OR dialysis AND patient AND Iran OR Iran* OR Islamic Republic of Iran. Additionally, the references of the collected articles were reviewed to ensure that all potentially relevant articles were included (Table 1).
| Database and | Search Strategy | Initial Search |
|---|---|---|
| PubMed | (("Dialysance"[All Fields] OR "dialysances"[All Fields] OR "dialysation"[All Fields] OR "dialysator"[All Fields] OR "dialysators"[All Fields] OR "dialyse"[All Fields] OR "dialysed"[All Fields] OR "dialyser"[All Fields] OR "dialysers"[All Fields] OR "dialysing"[All Fields] OR "dialysis solutions"[Pharmacological Action] OR "dialysis solutions"[MeSH Terms] OR ("dialysis"[All Fields] AND "solutions"[All Fields]) OR "dialysis solutions"[All Fields] OR "dialysate"[All Fields] OR "dialysates"[All Fields] OR "dialyzate"[All Fields] OR "dialyzates"[All Fields] OR "dialysis"[MeSH Terms] OR "dialysis"[All Fields] OR "dialyses"[All Fields] OR "dialyzability"[All Fields] OR "dialyzable"[All Fields] OR "dialyzation"[All Fields] OR "dialyze"[All Fields] OR "dialyzed"[All Fields] OR "dialyzer"[All Fields] OR "dialyzer s"[All Fields] OR "dialyzers"[All Fields] OR "dialyzing"[All Fields] OR "renal dialysis"[MeSH Terms] OR ("renal"[All Fields] AND "dialysis"[All Fields]) OR "renal dialysis"[All Fields] OR "end-stage renal disease"[All Fields] OR ("haemodialysis"[All Fields] OR "renal dialysis"[MeSH Terms] OR ("renal"[All Fields] AND "dialysis"[All Fields]) OR "renal dialysis"[All Fields] OR "hemodialysis"[All Fields]) OR "renal replacement therapy"[All Fields]) AND ("depressed"[All Fields] OR "depression"[MeSH Terms] OR "depression"[All Fields] OR "depressions"[All Fields] OR "depression s"[All Fields] OR "depressive disorder"[MeSH Terms] OR ("depressive"[All Fields] AND "disorder"[All Fields]) OR "depressive disorder"[All Fields] OR "depressivity"[All Fields] OR "depressive"[All Fields] OR "depressively"[All Fields] OR "depressiveness"[All Fields] OR "depressives"[All Fields] OR "depressive disorders"[All Fields]) AND ("iran"[MeSH Terms] OR "iran"[All Fields] OR "iran*"[All Fields] OR "Islamic Republic of Iran"[All Fields])) AND ((ffrft[Filter]) AND (1000/1/1:2024/4/19[pdat]) AND (english[Filter] OR persian[Filter])) | 64 |
| Scopus | TITLE-ABS-KEY (dialysis OR "end-stage renal disease" OR hemodialysis OR "renal replacement therapy") AND TITLE-ABS-KEY (depression OR "depressive disorders") AND TITLE-ABS-KEY (Iran) AND (LIMIT-TO (PUBSTAGE,"final”)) AND (LIMIT-TO (OA,"all")) AND (LIMIT-TO (DOCTYPE,"ar”)) AND (LIMIT-TO (LANGUAGE,"English”) OR LIMIT-TO (LANGUAGE,"Persian")) | 25 |
| Web of Sci-ence | (ALL= (depression OR “depressive disorders”) AND ALL= (dialysis OR "end-stage renal disease" OR hemodialysis OR "renal replacement therapy") AND ALL= (Iran)) and Open Access and Article (Document Types) and English (Languages) and All Open Access (Open Access) | 41 |
| PsycINFO | Depression AND (dialysis OR "end-stage renal disease") AND Iran | 10 |
| Magiran | Depression + Dialysis | 85 |
| SID | Depression AND Dialysis | 42 |
| Search engine | ||
| Google scholar | Allintitle: Depression AND (dialysis OR "end-stage renal disease" OR hemodialysis OR "renal replacement therapy") AND Iran | 9 |
Abbreviation: SID, scientific information database.
3.2. Study Selection and Data Extraction
Inclusion criteria for this study were all observational studies, including descriptive (survey), cross-sectional, longitudinal, and correlational studies published in Persian and English that used the BDI questionnaire. The components of the PICO model were as follows:
-Participants: Patients
- Intervention/Exposure: End-stage renal disease
- Control: None
- Outcomes: Depression
Exclusion criteria included articles without free access to the full text, review articles, commentaries, letters to the editor, conference abstracts, gray literature, articles reviewed during the COVID-19 pandemic, books, qualitative studies, and studies that did not report the prevalence of depression using the BDI questionnaire.
After applying the inclusion and exclusion criteria and removing duplicates, two authors (PI and MA) independently screened the titles and abstracts. Any disagreements during this process were referred to a third author (RB) and resolved through consensus. Four authors (SA, MAF, MAR, and HS) reviewed the full-text articles. The reviewed studies covered several provinces in Iran, including Tehran, Isfahan, Chaharmahal and Bakhtiari, and Markazi (central region); Golestan, North Khorasan, Ardabil, and Mazandaran (northern region); Fars (southern region); and South Khorasan and Razavi (eastern region).
Data extraction was performed using a researcher-made checklist. This checklist consisted of four parts: General information of the article (authors' names, year of publication, location), participants' characteristics (age, sample size), study method details (type of study, data collection tool), and the outcomes (prevalence of depression) (Table 2).
| Authors and Ref. | Publication Year | Location | Prevalence (%) | Sample Size | Mean Age | Instrument | Quality Score |
|---|---|---|---|---|---|---|---|
| Mogharab (21) | 2011 | Birjand | 56.7 | 60 | 54.4 | BDI | 15 |
| Afshar (22) | 2010 | Tehran | 70 | 120 | 57.6 | BDI | 14 |
| Raeesi (24) | 2005 | Tehran | 60 | 80 | 52.9 | BDI | 14 |
| Modanlou (25) | 2005 | Gorgan | 68.2 | 129 | — | BDI | 12 |
| Zahir al-Din (26) | 2005 | Tehran | 69 | 120 | 53.5 | BDI | 13 |
| Salehi and Noormohammadi-Sarab (27) | 2014 | Tehran | 50 | 60 | 41.3 | BDI | 13 |
| Roozbeh (28) | 2011 | Shiraz | 76 | 135 | 52.4 | BDI | 13 |
| Hemati (29) | 2013 | Shahrekord | 69.5 | 171 | 57.52 | BDI | 11 |
| Ossareh (30) | 2014 | Tehran | 40.7 | 150 | 56.4 | BDI | 14 |
| Hashemi (31) | 2014 | Shirvan | 39.2 | 46 | — | BDI | 11 |
| Anjomshoa (32) | 2014 | Kerman | 57.4 | 217 | 53.6 | BDI | 14 |
| Sanavi (33) | 2012 | Tehran | 70 | 120 | 75.5 | BDI | 15 |
| Ekramzadeh (34) | 2015 | Shiraz | 62 | 110 | 47.8 | BDI | 14 |
| Norozi Firoz (3) | 2019 | Mazandaran | 44.8 | 310 | 59.6 | BDI | 14 |
| Taraz (35) | 2012 | Tehran | 61.4 | 83 | 57.4 | BDI | 14 |
| Amirkhanlou (36) | 2017 | Gorgan | 83.9 | 194 | 54.01 | BDI | 13 |
| Baghcheghi and Koohestani (37) | 2020 | Saveh | 89.54 | 172 | 49.09 | BDI | 13 |
Abbreviation: BDI, beck depression inventory.
3.3. Quality Assessment
Mitton's checklist was used to evaluate the quality of the reviewed articles (Appendix in Supplementary File) (38). This checklist consists of 5 items and assesses various aspects of methodology, including literature review, research questions and design, population and sample, data collection, and analysis. Each item in this checklist is scored as follows: Zero (not present or not reported anywhere in the article), 1 (present but of low quality), 2 (present and of midrange quality), or 3 (present and of high quality). The maximum possible quality score is 15, with a score of 10 or above considered acceptable. Articles were scored independently by two researchers, and any disagreements were resolved by a third reviewer.
3.4. Statistical Analysis
Given that the prevalence of depression among dialysis patients followed a normal distribution, the variance for each study was calculated using the variance of the normal distribution formula: Var
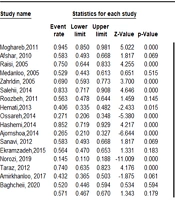
To calculate the prevalence of depression among dialysis patients by year, quality, and region, a subgroup analysis was conducted. Meta-regression was used to investigate the relationship between the prevalence of depression among dialysis patients and factors such as the year of publication, mean age, and sample size. All analyses were performed using Meta-Analysis software (version 2.2.064).
4. Results
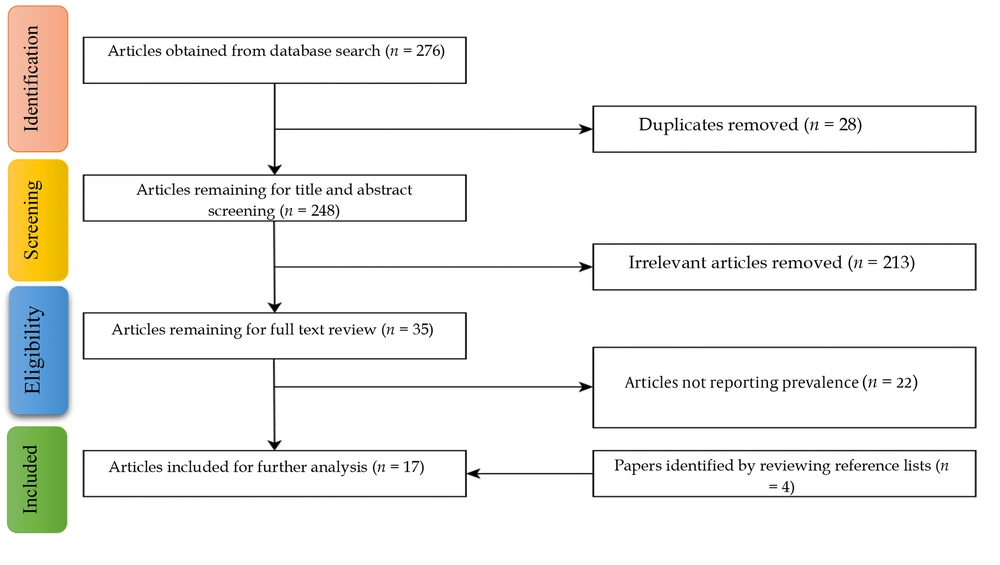
A total of 276 articles were identified in the initial search. In the first and second stages of screening, 28 duplicates and 213 irrelevant articles were excluded after examining the titles and abstracts. In the third stage, after a careful review of the remaining articles, 22 articles were removed because they did not report the prevalence of depression among dialysis patients using the BDI questionnaire. Four additional papers were obtained from the reference lists of the articles. Finally, 17 articles were included in the study to assess the prevalence of depression among dialysis patients in Iran (Figure 1).
4.1. Characteristics of Included Studies
A total of 17 observational articles, encompassing 2,277 patients, were analyzed. The earliest article was published in 2005, and the most recent in 2020. These studies were conducted across 12 provinces of Iran, with the majority being performed in Tehran province (9 studies). The sample sizes in the included studies ranged from 46 to 310 participants. In terms of methodological quality, all studies demonstrated the lowest level of bias (Table 1).
4.2. Prevalence of Depression Among Dialysis Patients in Iran
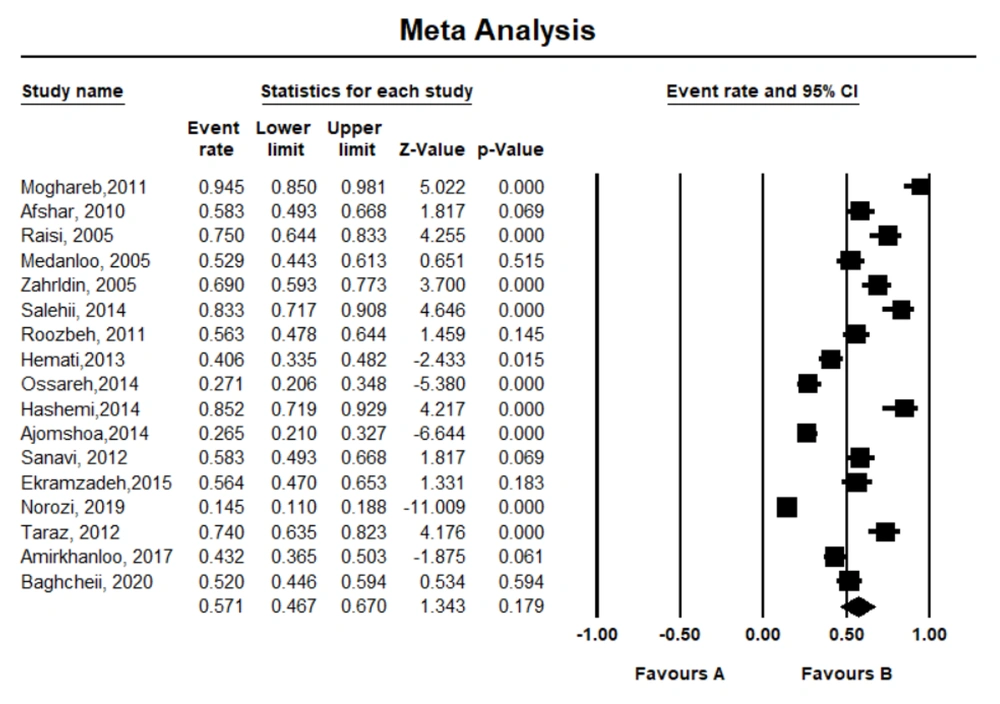
The heterogeneity of the reviewed studies was 95.07%. Using the random-effects model, the pooled prevalence of depression among dialysis patients was estimated to be 0.571 (95% Confidence Interval [CI]: 0.467 - 0.670) (Figure 2).
The results of the subgroup analysis indicated that the highest prevalence rate was reported in the eastern region of Iran, at 0.705 (95% CI: 0.051 - 0.991). Additionally, the pooled prevalence rate was higher in studies conducted before 2010, with a rate of 0.636 (95% CI: 0.536 - 0.727) (P ≤ 0.01). The quality of the 17 included articles was assessed as either high or medium, based on their overall quality scores. Articles classified as high quality had an overall score exceeding 14, while those classified as medium quality had a score lower than 14 (Table 3).
| Variables | Number of Studies | Prevalence | CI (95%) | Heterogeneity | |
|---|---|---|---|---|---|
| Percentage | P-Value | ||||
| Region | |||||
| Central | 9 | 0.600 | 0.483 - 0.707 | 92.38 | ≤ 0.01 |
| Northern | 4 | 0.476 | 0.231 - 0.733 | 97.18 | ≤ 0.01 |
| Southern | 2 | 0.563 | 0.500 - 0.624 | 0 | 0.99 |
| Eastern | 2 | 0.705 | 0.051 - 0.991 | 97.69 | ≤ 0.01 |
| Quality | |||||
| High | 9 | 0.543 | 0.365 - 0.711 | 96.67 | ≤ 0.01 |
| Moderate | 8 | 0.599 | 0.500 - 0.690 | 88.71 | ≤ 0.01 |
| Year | |||||
| > 2010 | 13 | 0.550 | 0.426 - 0.669 | 95.56 | ≤ 0.01 |
| ≤ 2010 | 4 | 0.636 | 0.536 - 0.727 | 76.59 | ≤ 0.01 |
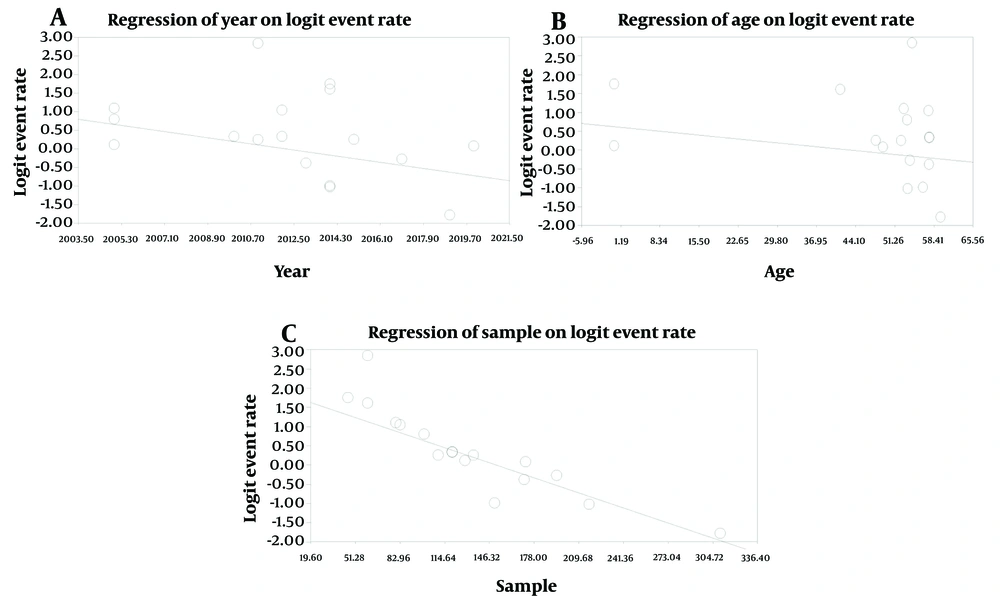
The present meta-analysis exhibited high heterogeneity, likely due to differences in study quality, methodology, and sample size among the studies (I² = 95.07%, P = 0.01). As a result, we used the random-effects model to account for the observed variability. The results of the meta-regression analysis showed a significant relationship between the prevalence of depression among dialysis patients and the year of publication, mean age, and sample size of the studies (P < 0.05) (Table 4 and Figure 3). Specifically, for each unit increase in sample size, the prevalence of depression among dialysis patients decreased by 0.01%. Similarly, the prevalence of depression decreased by 0.09% per year of publication. Additionally, for each unit increase in the mean age of patients, the prevalence of depression among dialysis patients decreased by 0.01%.
| Suspected Variables | Coefficient | Significance (P) |
|---|---|---|
| Year | -0.09 | ≤ 0.01 |
| Sample size | -0.01 | ≤ 0.01 |
| Mean age | -0.01 | ≤ 0.01 |
4.3. Publication Bias
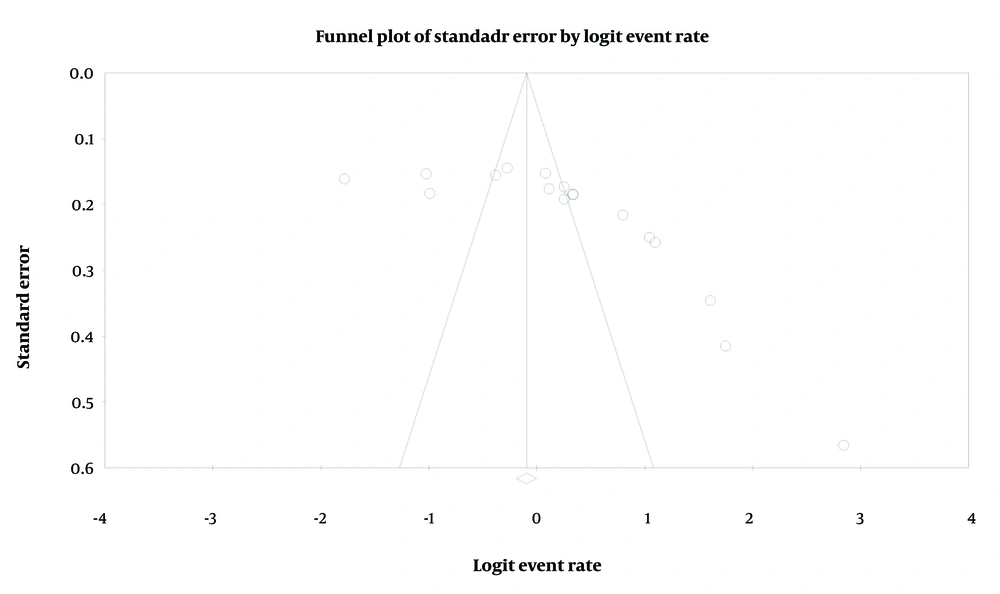
To evaluate publication bias, we used funnel plots and Egger’s test. In the funnel plot, each point represents a separate study, and a symmetrical distribution indicates the absence of publication bias. However, according to Egger’s test, the publication bias was found to be significant (P = 0.02) (Figure 4).
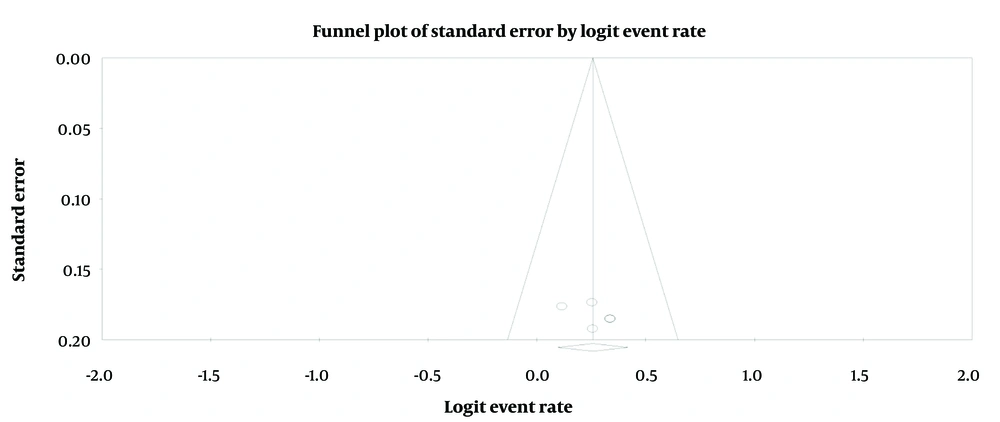
In Figure 4, the relative asymmetry of the results from the primary studies can be observed around the axis, indicating potential publication bias. To address this heterogeneity and possible publication bias, outlier effects were identified and removed through sensitivity analysis. After performing the sensitivity analysis, 12 studies exhibiting publication bias were excluded from the meta-analysis (Figure 5). The resulting funnel plot in Figure 5 is more symmetrical than the one in Figure 4, indicating reduced publication bias.
Furthermore, based on the "safe number of destructions" Index (the number of missing studies required to bring the P-value to alpha), the analysis showed that after introducing 90,000 non-significant effect sizes into the meta-analysis, the calculated random effect size would become non-significant. Consequently, the significance level would shift from 0.02 to above 0.05. As a result of removing the outlier effect sizes, 5 studies remained in the analysis.
Based on the five studies that remained after sensitivity analysis, the pooled prevalence of depression among dialysis patients, using the random-effects model, was estimated to be 0.564 (95% Confidence Interval [CI]: 0.524 - 0.603) (Table 5).
| Variables | Model | Frequency | Prevalence | Standard Error | Variance | Z-Value | P-Value |
|---|---|---|---|---|---|---|---|
| Before sensitivity analysis | Random | 17 | 0.571 | 0.295 | 0.087 | 1.34 | 0.17 |
| After sensitivity analysis | Random | 5 | 0.564 | 0.023 | 0.001 | 3.14 | 0.002 |
5. Discussion
The purpose of this study was to determine the prevalence of depression among dialysis patients in Iran. Overall, there were 17 studies on this topic up until April 19, 2024. After sensitivity analysis, the prevalence of depression among dialysis patients was estimated to be 0.564. Studies from around the world have reported varying prevalence rates. For example, the prevalence of depression among dialysis patients was reported to be 75% in Pakistan in 2012 (40), 80% in Iraq in 2013 (41), 63% in Saudi Arabia in 2014 (42), and 40.8% in Lebanon in 2018 (43). In Iran, the prevalence of depression among dialysis patients is higher than in the general population. A 2023 study showed that the prevalence of depression among the general Iranian population was 47% (44). Differences in prevalence rates can be attributed to various factors, such as patient characteristics, cultural differences, and socioeconomic and health status in different countries (45-49).
Depression is strongly correlated with patient characteristics such as age, sex, and education level (45-47). For instance, a study in Saudi Arabia in 2020 found that depression was more prevalent among female patients than male patients (45). Socioeconomic status is recognized as a significant social determinant of health in both developed and developing countries, with individuals of higher socioeconomic status more likely to have better physical and mental health (47, 48, 50-52). A 2013 study in Turkey showed that the prevalence of depression was higher in patients with lower education and socioeconomic status (49).
The results of this study showed that for each unit increase in the mean age of patients, the prevalence of depression among dialysis patients decreased by 0.01%. This finding contrasts with a 2010 study by Cengic and Resic, which found that older patients are naturally more likely to have underlying diseases such as hypertension, cardiovascular disease, and diabetes mellitus, which increase the risk of depression (53). However, a 2004 study reported that the prevalence of depression was lower among elderly dialysis patients compared to younger patients (54).
The highest prevalence of depression among dialysis patients was observed in eastern Iran, possibly due to differences in healthcare facilities, the number of beds, and transportation costs in different regions. However, given the small number of studies reviewed, this finding should be interpreted with caution. The studies on the prevalence of depression among dialysis patients in Iran were conducted in a limited number of provinces, which limits the comprehensiveness and generalizability of the findings. Therefore, similar studies should be conducted in other provinces of the country.
The results also indicated that the prevalence of depression among dialysis patients decreases by 0.01% for each unit increase in sample size. This suggests that studies with smaller sample sizes may be subject to sampling bias. Therefore, studies on the prevalence of depression among dialysis patients must ensure sufficient sample sizes and appropriate sampling methods.
Moreover, the prevalence of depression among dialysis patients decreased by 0.09% per year of publication, which could be due to improvements in diagnostic instruments, dialysis procedures, and kidney transplantation techniques over the years.
Patients with chronic kidney disease undergoing hemodialysis experience significant psychological stress in addition to physiological distress. These patients endure not only stressful medical procedures like dialysis but also declining psychosocial function as their disease progresses. Stress and depression are common mental disorders among these patients (55). Therefore, it is crucial to provide solutions for reducing depression in this population.
Like many other studies, this review has some limitations, including: (a) the wide variety of tools used for data collection; (b) the high heterogeneity identified in our study, which was addressed through the use of a random-effects model but still highlights variability between studies, potentially impacting the reliability of the pooled prevalence estimate; (c) the lack of valuable information (e.g., sex, marital status, education level, occupation) that would allow for a more detailed analysis; and (d) the inclusion of articles only in English and Persian, which may introduce language bias and potentially exclude relevant studies published in other languages. Future researchers are encouraged to conduct quantitative studies in other provinces of Iran and to include detailed demographic information in their analyses for use in systematic reviews and meta-analyses.
Despite the challenges faced in analyzing the literature, the results of this study could be valuable in identifying areas where depression among dialysis patients needs improvement. This information could be useful for informing health system policymakers, healthcare professionals, and patients, raising awareness and potentially leading to beneficial outcomes, including reducing depression among dialysis patients.
5.1. Conclusions
Depression is highly prevalent among dialysis patients in Iran, with approximately half of them experiencing this condition. Given the high prevalence of depression in this population, it is recommended to conduct periodic psychiatric examinations for timely diagnosis and treatment of depression in dialysis patients.