1. Background
The health of the mouth is crucial for speaking and eating. Oral mucosal problems are prevalent in society and can significantly impact oral function and overall well-being. After dental issues, oral mucosal diseases are the second leading cause of oral health problems (1). Chronic or acute lesions in the oral mucosa can cause severe pain during oral function, leading to a reduced quality of life for patients. These lesions can disrupt eating, swallowing, and speaking, as well as negatively affect oral health (2). Additionally, they may result in bad breath and hinder social communication for patients (3).
Mucosal diseases encompass a wide range of conditions, from benign and self-limiting to malignant and potentially fatal. These lesions can appear on various areas of the oral mucosa, including the cheeks, floor of the mouth, tongue, palate, and lips. They may be localized or involve the entire oral mucosa (4). There are over 200 types of oral mucosal diseases, which can be caused by various factors. Some of these diseases are associated with systemic conditions like pemphigus vulgaris, which can lead to ulcers in the oral mucosa. Others are caused by local factors, such as the sharpness of a broken tooth, which can result in hyperkeratosis of the cheek mucosa (5). Certain conditions like geographic tongue, recurrent mouth sores, pregnant tongue, and oral melanotic macule have unknown causes. However, it has been proven that smoking is a significant risk factor for the development of oral mucosal lesions (6).
Sohrabi et al. reported a tobacco addiction prevalence of approximately 14% among Iranians. They found that cigarette use is the most common method of tobacco consumption among Iranians, while hookah is the preferred method among Iranian youth (7). Hookah smoking is more socially accepted in Iranian culture compared to cigarettes and is believed to have fewer complications. However, the prevalence of hookah use has been increasing in recent years (8). The method of tobacco use can influence the type of oral complications that arise (4). For instance, smoking cigarettes can lead to hyperplastic candidiasis and nicotinic stomatitis, whereas non-smoking tobacco use can cause pouch keratosis (9). A study conducted on Indian dental students who use tobacco by Hadzic et al. (10) identified tongue discoloration as the most common oral complication associated with hookah use. Other complications of smoking include teeth discoloration, periodontal problems, and halitosis, some of which can also be observed in non-smokers (4).
Most studies conducted in Iran have primarily focused on the complications of cigarette smoking and paid less attention to the complications of hookah use. There exists a perception among the Iranian population that hookah smoking carries fewer risks compared to other forms of tobacco use, which has contributed to the increased prevalence of hookah use in recent years (11). However, we did not find any studies investigating the differences in oral mucosal complications between cigarette smoking and hookah use specifically in Iran.
2. Objectives
This study aims to assess the prevalence of oral lesions among individuals who smoke cigarettes or use hookah and compare it with those who do not use tobacco. By conducting this research, we hope to gain insights into the potential disparities in oral complications resulting from different methods of tobacco consumption.
3. Methods
3.1. Study Population
After obtaining permission from the Ethics Committee, this cross-sectional study was conducted from Spring 2022 to Winter 2023. The study focused on patients who were referred to the Faculty of Dentistry for dental treatments and were selected using consecutive sampling methods. The statistical population of the study consisted of three groups: Cigarette users, hookah users, and non-tobacco users. The inclusion criteria for the study were as follows: Individuals aged between 15 and 60 years, absence of any systemic diseases, no alcohol or drug use except for cigarettes and hookah, and not using removable or partial dentures. The cigarette group comprised individuals who had smoked at least five cigarettes or more daily for a minimum of one year and did not use hookah (group A). The hookah group included individuals who used hookah more than twice a week for at least one year and were not addicted to cigarettes (group B). The non-tobacco user group consisted of individuals who had abstained from both hookah and cigarette use for at least one year (group C).
3.2. Data Collection
The oral examination of the subjects was conducted by an oral medicine specialist using a mirror, probe, and dental gauze to hold the tongue. The examination took place under the light of a dental unit. Any findings on the mucous membranes of the palate, tongue, cheeks, floor of the mouth, and gums were documented using a pre-prepared form. In addition to the examination, participants were asked about their age, gender, and type of tobacco use (cigarettes or hookah) or non-use. For those who reported tobacco use, information regarding the duration and frequency of hookah or cigarette use was also collected. Participants were also questioned about symptoms such as dry mouth, bad taste, and halitosis, and their responses were recorded on a specialized data collection form. The classification of oral mucosal lesions diagnosed in individuals followed the criteria set by the World Health Organization (WHO). If necessary, a biopsy or swab was performed to confirm the diagnosis (12).
It is important to note that this study focused specifically on the objective of the research, and therefore the registration of dental and periodontal problems of the patients was not included. However, if any dental or periodontal issues were identified during the examination, the patient was referred to the appropriate unit for further evaluation and treatment.
3.3. Calculation of Sample Size
According to the information provided, the sample size formula and a power of 90% were used to determine the sample size for each group in Bardellini's study (13). Additionally, a 10% dropout rate was considered when calculating the final sample size. As a result, a sample size of 29 people per group was determined, totaling 87 participants in the study.
Considering the 10% dropout rate, the adjusted sample size for each group is calculated as follows:
To obtain the total sample size for the study, multiply the adjusted sample size by the number of groups:
3.4. Statistical Analysis
Quantitative variables were reported using measures of central tendency, such as the mean, and measures of dispersion, such as the standard deviation. Qualitative variables were reported using both the number of occurrences and the percentage. To examine the relationship between qualitative variables, a chi-square test or Fisher's exact test was employed. The significance level for these tests was set at less than 0.05, indicating that any observed associations with a p-value below this threshold were considered statistically significant. The data analysis was conducted using SPSS version 23 software, a widely used statistical analysis tool.
3.5. Ethical Considerations
The study adhered to the principles outlined in the declaration of Helsinki and received ethical approval from the Ethics Committee (IR.AJUMS.REC.1397.258). Prior to participation, patients were provided with comprehensive information regarding the research objectives and were assured that their personal information would be kept confidential. Inclusion in the study required patients to provide written consent.
A dedicated research form was used to record data such as age, gender, duration and type of cigarette or hookah use, research-related questions, and clinical findings from oral examinations. Patients were fully informed about the research objectives and their confidentiality rights, and their participation was contingent upon signing a written consent form.
4. Results
In a two-year study, 102 individuals who met the entry criteria were included. Among them, 23 were women (22.5%) and 79 were men (77.5%). The mean age of the participants was 38.39 years, with a standard deviation of 13.05 years. The age range of the participants varied from 19 to 60 years. Out of the total sample, 45 individuals (44.1%) were classified as cigarette users (group A), 30 individuals (29.4%) were classified as hookah users (group B), and 27 individuals (26.5%) did not use cigarettes or hookah (group C).
Within group A, there were 4 women (8.9%) and 41 men (91.1%). Their average age was 40.87 years, with a standard deviation of 13.14 years. Twelve people (26.7%) smoked 5 to 10 cigarettes a day, 12 people (26.7%) smoked 11 to 20 cigarettes a day, and 21 people (46.7%) smoked more than 20 cigarettes a day. Within group B, there were 8 women (26.7%) and 22 men (73.3%). Their average age was 35.67 years, with a standard deviation of 12.28 years. Additionally, 2 people (6.7%) smoked hookah at least twice a week, but not daily, while 28 people (93.3%) used hookah daily. The average duration of each hookah session was 55.37 minutes, with a standard deviation of 31.22 minutes.
Within group C, there were eleven women (40.7%) and sixteen men (59.3%). Their average age was 37.30 years, with a standard deviation of 13.43 years. The demographic characteristics of groups A and B are shown in Table 1. The results of the chi-square test indicated that there were no significant differences between the studied groups in terms of halitosis (P = 0.621) and complaints of dry mouth (P = 0.074).
| Variables | No. (%) | Age; Mean ± SD | Number of Years of Addiction |
|---|---|---|---|
| Cigarette users | 40.87 ± 13.14 | 18.27 (11.59) | |
| Women | 4 (8.9) | ||
| Men | 41 (91.1) | ||
| Hookeh user | 35.67 ± 12.28 | 20.62 (6.85) | |
| Women | 8 (26.7) | ||
| Men | 22 (73.3) |
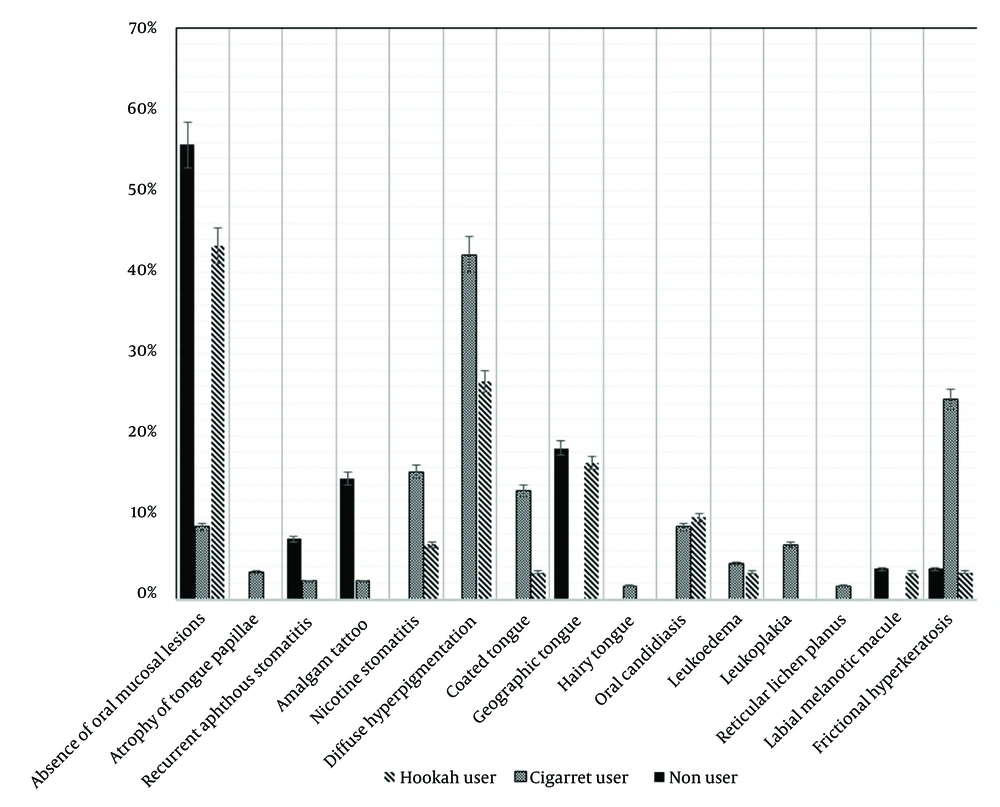
However, group B subjects reported a significantly higher incidence of bad taste in the mouth compared to the other two groups (P = 0.004) (Table 2). Based on the results shown in Figure 1 of individuals who did not use cigarettes or hookah did not exhibit any oral lesions. Among cigarette users, the most frequently observed type of oral lesion was pigmentation of the oral mucosa, while leukoplakia was observed in 6.7% of individuals in this group.
| Variables | A. Cigarette Users | B. Hookah Users | C. Non-users | Total | P- Value |
|---|---|---|---|---|---|
| Complaints of halitosis | 0.621 | ||||
| Yes | 7 (15.6) | 7 (23.3) | 4 (14.8) | 18 (17.6) | |
| No | 38 (84.4) | 23 (76.7) | 23 (85.2) | 84 (82.4) | |
| Complaints of xerostomia | 0.074 | ||||
| Yes | 5 (11.1) | 9 (30) | 0 (0) | 14 (13.7) | |
| No | 40 (88.9) | 21 (70) | 27 (100) | 88 (86.3) | |
| Complaints of bad taste in the mouth | 0.004 b | ||||
| Yes | 16 (35.6) | 9 (30) | 3 (11.1) | 28 (27.5) | |
| No | 29 (64.4) | 21 (70) | 24 (88.9) | 74 (72.5) |
a Values are expressed as No. (%) or mean ± SD.
b P < 0.05.
In the hookah user group, pigmentation of the oral mucosa was also the most common type of lesion (Table 3).
| Oral Leasion | A. Cigarette Users | B. Hookah Users | C. Non-users | Total |
|---|---|---|---|---|
| Without lesions | 4 (8.9) | 13 (43.3) | 15 (55.6) | 32 (25.6) |
| Atrophy of the lingual papillae | 2 (3.3) | 0 (0) | 0 (0) | 2 (1.6) |
| Oral aphthous ulcer | 1 (2.2) | 0 (0) | 2 (7.4) | 3 (2.4) |
| Amalgam tattoo | 1 (2.2) | 0 (0) | 4 (14.8) | 5 (4) |
| Nicotinic stomatitis | 7 (15.6) | 2 (6.7) | 0 (0) | 9 (7.2) |
| Oral hyperpigmentation | 19 (42.2) | 8 (26.7) | 0 (0) | 27 (21.6) |
| Coated tongue | 6 (13.3) | 1 (3.3) | 0 (0) | 7 (5.6) |
| Geographic tongue | 0 (0) | 5 (16.7) | 5 (18.5) | 10 (8) |
| Hairy tongue | 1 (1.6) | 0 (0) | 0 (0) | 1 (0.8) |
| Candidiasis | 4 (8.9) | 3 (10) | 0 (0) | 7 (5.6) |
| Leukoedema | 2 (4.4) | 1 (3.3) | 0 (0) | 3 (2.4) |
| Leukoplakia | 3 (6.7) | 0 (0) | 0 (0) | 3 (2.4) |
| Oral lichen planeus | 1 (1.6) | 0 (0) | 0 (0) | 1 (0.8) |
| Oral malacotic macule | 0 (0) | 1 (3.3) | 1 (3.7) | 2 (1.6) |
| Frictional hyperkeratosis | 11 (24.4) | 1 (3.3) | 1 (3.7) | 13 (104) |
a Values are expressed as No. (%).
5. Discussion
The use of hookah, also known as a water pipe, is not culturally forbidden in Iranian families, and it is commonly believed that hookah is less addictive and has fewer complications than cigarettes. However, scientific studies have shown that hookah, similar to cigarettes, can lead to cardiovascular and pulmonary complications (14, 15).
While there is limited research specifically focusing on the oral complications of hookah compared to cigarettes, a recent study aimed to investigate the impact of hookah and cigarette use on oral health (16). The present findings revealed that individuals who smoke hookah experience a significantly higher incidence of bad taste in the mouth compared to non-smokers. However, there was no significant difference between tobacco users and non-users in terms of complaints related to dry mouth and halitosis.
The study results also revealed that the prevalence of oral mucosal lesions in people who use cigarettes was higher than in those who use hookah, while the prevalence of oral mucosal lesions in people who did not use tobacco was lower than in the other two groups. The most common oral mucosal lesion observed among hookah smokers was hyperpigmentation. It is important to note that these findings are specific to the oral health effects of hookah and cigarette smoking. Other studies have demonstrated that both forms of tobacco use can have detrimental effects on overall health, including an increased risk of lung cancer, heart disease, and other respiratory conditions (17).
Pigmentation of the oral mucosa was the most common mucosal lesion observed in the mouths of both groups, although its prevalence was higher in cigarette users than in hookah users. These results were consistent with the study by Saeidi et al., which showed that oral mucosal lesions are more prevalent in people who use cigarettes than in those who use hookah. They also reported that the prevalence of oral mucosal pigmentation is 16% in cigarette users and 1% in hookah users (18). Smoker's melanosis in the oral mucosa is a common side effect of tobacco use, with the cheek mucosa being the most frequently affected area (4). However, further studies are needed to determine the reasons behind the lower occurrence of hyperpigmentation in individuals who use hookah compared to cigarette users. These studies should investigate whether the heat generated by burning tobacco or the compounds present in hookah smoke play a role in stimulating an increase in melanin production by oral melanocytes.
In this study, the researchers observed leukoplakia, a premalignant lesion, exclusively in the group of cigarette users and not in the group of hookah users. This finding has already been referenced by oral cancer specialists in India (19). Another study by El-Hakim and Uthman on oral squamous cell cancer suggested that heat and tobacco extract are the primary factors causing cancer in tobacco consumers (20). In the case of hookah use, the smoke inhaled through tobacco has a lower temperature than the ambient temperature. Additionally, unlike cigarettes, no tobacco extract can pass through the water bath in the hookah and travel a distance of 200 to 300 cm to reach the person's mouth (19). These differences in temperature and filtration may contribute to variations in the risk of developing certain conditions between cigarette and hookah users. However, it's important to note that while hookah use may have some differences in risk compared to cigarette smoking, it is still associated with various health risks, including oral and lung diseases. Quitting tobacco use altogether is the best way to reduce these risks.
The results of the present study did not find any significant difference in the self-reported rate of halitosis among the three study groups. It is worth noting that a study conducted by Al-Sadhan in Saudi Arabia demonstrated that both hookah and cigarette users reported a significantly higher rate of halitosis compared to non-smokers (21). These conflicting results are not surprising, as indicated by Kauss et al. (22), who reported a high level of heterogeneity among studies regarding halitosis in tobacco users. One contributing factor to this heterogeneity is the variation in populations studied and the differing definitions provided for halitosis across various research studies (22). Additionally, tobacco use often leads to stale breath, which can be challenging to eliminate. Over time, individuals who use tobacco may become accustomed to this breath, and it may no longer bother them (23). Romano et al. also showed that smokers are likely to underreport their gingival recession and halitosis (24). In other words, it can be stated that tobacco users do not exhibit a higher level of halitosis (self-reported) compared to non-users in society, likely due to their habituation to the smell of tobacco on their breath.
In this study, reports of bad taste in the mouth were significantly higher in hookah users than in cigarette users and non-users. This study is the first to address this issue specifically in relation to hookah use. However, numerous studies have been conducted on the impact of tobacco use (excluding hookah) on the sense of taste, yielding conflicting results. For instance, Michalak et al. demonstrated that a bad taste in the mouth is the most commonly reported complaint among patients who use tobacco (25). This finding is consistent with the present study, indicating that any form of tobacco used in the mouth, whether smoked or smokeless, can affect the oral mucosa and alter the sense of taste. The extent of damage caused by tobacco depends on factors such as exposure time, concentration, and toxicity (26). Hookah users typically take 100 to 200 puffs during each one-hour session, which is significantly higher than the 8 to 10 puffs taken with cigarettes. This prolonged exposure to hookah smoke poses a risk to the oral mucosa. Additionally, the combustion of charcoal used to light the tobacco in hookah produces harmful substances like carbon monoxide and other chemicals not found in cigarette smoke (27). These factors may explain the increased reports of bad taste in the mouths of hookah users. However, further research is necessary to fully understand the implications of these findings.
Various mechanisms have been proposed to explain the reduced sense of taste in tobacco users. These include changes in the shape, size, and blood supply to the fungiform papillae, a decrease in the number of taste cells, lower levels of zinc, vitamins B and E, and folic acid, as well as the impact of nicotine on sensory nerve endings (28). Previous studies investigating changes in taste after tobacco use have yielded mixed results. For instance, Khan et al. (29) and Peterson et al. (30) found no difference in taste perception between chronic tobacco users and non-users regarding the ability to detect the four main tastes. However, more research is needed to establish conclusive evidence in this area. A systematic review conducted by Da Ré et al. (31) found that there is insufficient evidence regarding the effect of tobacco on the sense of taste, indicating the need for further studies in this area.
To assess the presence of xerostomia (dry mouth) in the study population, the question "Do you feel your mouth is dry?" was utilized. This question was selected from the Fox questionnaire, and a positive response to it indicates mild xerostomia (32). The prevalence of a positive response to this question was higher among cigarette users (35.6%) and hookah users (30%) compared to tobacco non-users (11.1%). However, this difference did not reach statistical significance (P = 0.074). Contradictory results were observed in the reviewed articles concerning this topic. Khan et al. (33) demonstrated that long-term tobacco use does not impact saliva secretion, which aligns with the findings of the present study. Additionally, an animal study indicated that nicotine can potentially increase saliva secretion through its interaction with nicotinic receptors (34). In other words, smoking tobacco can stimulate saliva production through mechanical, chemical, and thermal means, leading to increased saliva secretion (29, 35). However, it has also been observed that tobacco consumption can have the opposite effect and reduce saliva secretion, resulting in complaints of xerostomia (dry mouth) (36-38). Further research is necessary to fully understand this relationship.
Given the reported complaints of bad taste in the mouths of individuals addicted to tobacco, it is recommended that future studies compare the saliva composition of individuals addicted to cigarettes and hookah with that of healthy individuals. It is important to note that the present study has a limitation in terms of its small sample size. To obtain more reliable and conclusive results, larger studies with a greater number of participants are required.
One of the characteristics of hookah use is the widespread variation among consumers in the preparation of tobacco-based smoking mixtures, making it very difficult to standardize. This variability can be considered another limitation of the present study.
5.1. Conclusions
In conclusion, the impact of tobacco use on oral mucosa lesions is evident when comparing individuals who do not use tobacco. The type and severity of these lesions vary significantly among tobacco users, with cigarettes having a more pronounced effect compared to hookah. The complications associated with cigarette use are also more severe. As a result, regular examinations to assess the condition of the oral mucosa are crucial for individuals who engage in tobacco use. By monitoring and evaluating the oral health of tobacco users, healthcare professionals can identify potential issues early on and provide appropriate interventions to mitigate further damage.