1. Background
Caesarean section (CS) is one of the most commonly undertaken operations worldwide and the frequency and desire of pregnant women to have CS rather than vaginal delivery is growing, which is not done in a standardized way (1). On the other hand, CS is a surgical procedure with numerous potential complications for both mother and child such as infection, organ injuries (2), thromboembolic complications (3), uterine rupture, and placental anomalies such as placenta previa, increta, or accrete (4). Recently it has been demonstrated that subsequent infertility is probably one of the serious complications of CS, which has not been well studied (4-7). On the other hand, it has been accepted that chronic diseases have some stresses for the body; especially, when they cause weight loss, they can interfere with ovulation, which is the main cause of infertility (8). A recent meta-analysis study evaluated the impact of CS on subsequent infertility reporting that CS decreased the subsequent birth rate by 11% (8). Moreover, some studies have reported that elective CS does not appear to cause infertility. In a study performed by Oral E et al., it was demonstrated that in recent studies, which have tried to explain the association between CS and subsequent fertility, some biases and confounding factors might lead to some unacceptable adverse effects of emergency CS (9). Furthermore, Smith GC et al. showed that it is unlikely that performing CS for the first pregnancy decreases the fertility of women in the second pregnancy (10). As to the best of our knowledge, there is not enough prospective study about this issue and on the other hand, due to antithesis results reported by the limited studies, this study was designed to evaluate subsequent infertility after CS.
2. Methods
2.1. Study Design and Target Group
This retrospective epidemiological study was conducted in obstetrics and gynecology of Ahvaz Imam hospital, south-west of Iran, from November 2011 to May 2015. All the patients with infertility after the first delivery were enrolled in the study. Inclusion criteria included patients referring to the infertility clinic of Ahvaz hospitals with a diagnosis of infertility (inability to conceive after having regular unprotected sex for more than 12 months, or female who cannot carry a full term pregnancy). Exclusion criteria consisted of patients with history of infertility before the first delivery, history of surgery on the pelvis, uterus, ovaries, and fallopian tubes after the first delivery, history of recurrent miscarriage, flawed and insufficient information in patients’ records and lack of access to the patient.
2.2. Participants
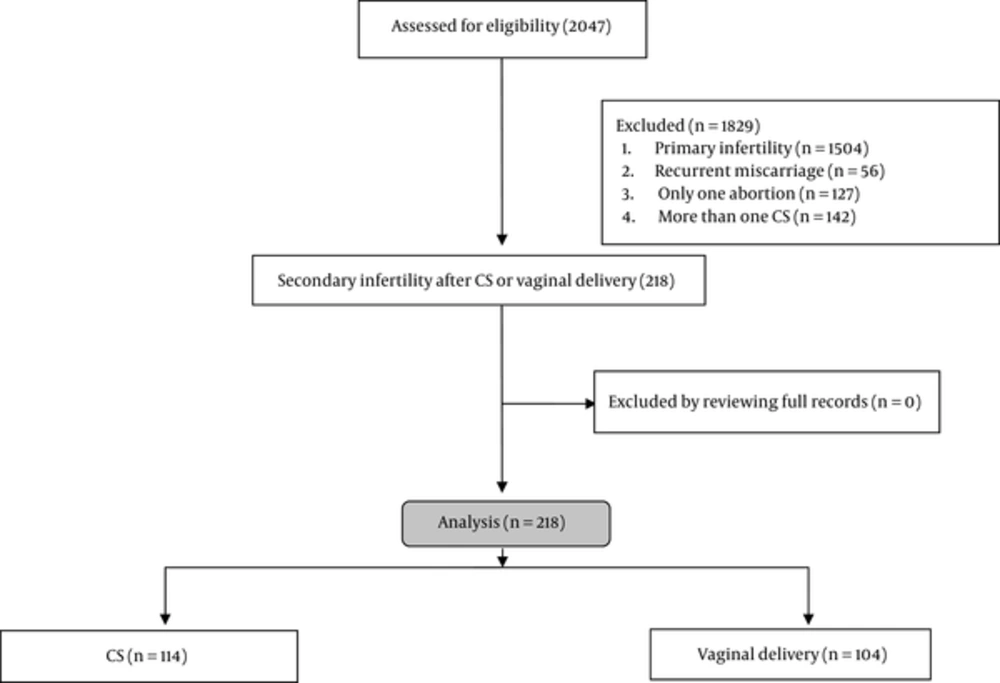
The study flowchart is shown in Figure 1. During the five years, 2047 patient’s records were collected indicating that 1504 cases had primary infertility, 56 cases had recurrent miscarriage, 127 cases had only one abortion, 142 cases had more than one CS and only 218 patients had secondary infertility after CS or vaginal delivery (including 114 (52.29%) after CS and 104 (47.7%) after vaginal delivery). Among 114 pregnant women undergoing CS, 63 cases (55.26 %) had emergency CS and 51 cases (44.73%) had elective CS. 218 patients who had been diagnosed with secondary infertility by an infertility specialist were included based on inclusion and exclusion criteria. Then, information of all patients was extracted from infertility clinic records including demographic features, type and duration of contraceptive methods, past medical history, and infertility problems. In case of incomplete information, we assessed the patients in a five-minute phone call for completing missing data and if we needed to see the patient’s records, we arranged face-to-face appointments. If we needed to contact the patients to complete information, we interviewed just the patient; first, we explained persuasively the issue, methods, and purpose of our study to the patient and the patient’s verbal consent was obtained regarding her participation and completing information. If the patient did not desire to participate in the study, we excluded her from the study. The study received an ethics approval from the ethics committee of Ahvaz Jundishapur University of Medical Sciences, and informed consent was obtained only from patients who participated in phone call assessment or in face-to-face appointments.
2.3. Data Analysis
Data were analyzed and reported only for patients with complete information. Statistical analysis of data was performed using SPSS version 22 software. Chi-square test was used to compare qualitative variables between groups. Kolmogorov-Smirnov test was used to evaluate the normal distribution of quantitative parameters. Student t-test and paired t-test were used for variables with normal distribution while Mann-Whitney and Wilcoxon tests were used for variables without normal distribution. The two tailed P value less than 0.05 was considered significant.
3. Results
Regarding the demographic features, age of participants was similar (P = 0.086) between the two groups (Table 1). The other features such as past medical history (P > 0.05), type (P = 0.711) and duration of using contraceptive methods (P = 0.194), and the interval between decision to pregnancy and referring to infertility clinics were similar between the patients with different methods of first delivery (P = 0.268).
| Variable | Group | P Value | |
|---|---|---|---|
| CS (N = 114) | Vaginal Delivery (N = 104) | ||
| Age, y | 31.85 ± 4.82 | 30.66 ± 5.41 | 0.086 |
| Duration of using contraceptive methods, y | 3.11 ± 1.41 | 2.88 ± 1.17 | 0.194 |
| Interval between decision to pregnancy and referring to infertility clinics, mo | 23.35 ± 12.92 | 25.56 ± 16.45 | 0.268 |
| Contraceptive methods | 0.711 | ||
| Withdrawal | 69 (60.5) | 69 (66.3) | |
| LD | 27 (23.7) | 18 (17.3) | |
| Condom | 15 (13.2) | 14 (13.5) | |
| Etc. | 3 (2.6) | 3 (2.9) | |
| Past medical history | |||
| Thyroid | 7 (6.1) | 10 (9.6) | 0.339 |
| Diabetes | 16 (14) | 7 (6.7) | 0.08 |
| Sign and symptoms | |||
| Dysmenorrhea | 27 (23.7) | 30 (28.8) | 0.386 |
| Dyspareunia | 23 (20.2) | 16 (15.4) | 0.357 |
| Hirsutism | 33 (28.9) | 27 (26) | 0.622 |
| Galactorrhea | 8 (7) | 11 (10.6) | 0.352 |
| Associated disorders | |||
| Men disorders | 86 (75.4) | 75 (72.1) | 0.577 |
| Uterine disorders | 11 (9.6) | 6 (5.8) | 0.286 |
| Fallopian tube disorders | 23 (20.2) | 26 (25) | 0.394 |
| Ovulation disorders | 42 (36.8) | 30 (28.8) | 0.21 |
Study Variables in CS and Vaginal Delivery Groupsa
Furthermore, we found that there were no significant differences between the groups in terms of sign and symptoms such as dysmenorrhea (P = 0.386), dyspareunia (P = 0.357), hirsutism (P = 0.622), and galactorrhea (P = 0.352). Moreover, associated disorders including Men disorders (P = 0.577), Uterine disorders (P = 0.286), Fallopian tube disorders (P = 0.394), and Ovulation disorders (P = 0.21) did not have significant differences between the groups.
4. Discussion
The aim of this study was to find a correlation between first CS and subsequent infertility. According to our results, CS did not increase the risk of subsequent infertility when compared to vaginal delivery. The study performed by Saraswat L et al. showed that women with secondary tubal infertility had the same rate of CS in the first delivery as compared to the other infertile women (21.4% vs. 21.6%) but they showed that CS was significantly lower in fertile control group (14.5%). After adjusting for confounding factors, they found that CS did not have any significant association with tubal infertility. However, they found that other factors such as history of intrauterine device use, pelvic inflammatory disease, ectopic pregnancy, endometriosis, and previous pelvic surgery might lead to secondary tubal infertility (11). Moreover, another study performed by Oral E et al. showed that elective CS did not have any significant correlation with subsequent infertility (9). Smith GC et al. showed that women with planned CS due to breech presentation had higher risk of infertility for the second birth as compared to women with vaginal delivery. However, after adjusting for confounding factors such as maternal and obstetric characteristics, this correlation did not remain significant. Moreover, they found that there is no association between the type of delivery and the number of pregnancy losses between the first and second births (10). All these studies found results similar to our findings.
On the other hand, Tollsnes MC et al. evaluated 596,341 women who had their first delivery during 1967 - 1996 and showed that CS increased the infertility in the second birth (if the infant survived than if it was stillborn or died). This suggests that the increasing infertility was not related to the indication of CS; therefore, reduced fertility in the second birth was due to the CS complications (12). On the other hand, Collin SM et al. evaluating 35,398 women of childbearing age (15 - 49 years) demonstrated that CS is associated with reduction in subsequent natural fertility in sub-Saharan Africa. On the other hand, infertility after CS was reported in developed countries, which reflects the differences in pathological and psychological factors, because most of CS indications in sub-Saharan Africa are emergency procedures for maternal indication, while in developed countries the desire of women for CS is the most indication for CS (13). Furthermore, Tanimura S et al. assessing 22 women with secondary infertility showed that infertility was associated with post-cesarean scar defect (14). Kjerulff KH et al. evaluated 52,498 women who had a first singleton live birth and showed that women who deliver their first child by CS have less chance to have a subsequent birth. They found a 15% reduction in subsequent birth rate after CS (15). Another study performed by Jacob L et al. on 6483 patients in CS group and 6483 in VD group demonstrated that CS is associated with an increased risk of sterility and subsequent infertility in Germany. In this study, they found that CS decreased subsequent pregnancies as polycystic ovary syndrome and deterioration of menstrual cycle did it (16). Gurol-Urganci I et al. assessing 1,047,644 first births to low-risk women using routinely collected data found that there is no or only a slight effect for CS on future fertility; they demonstrated that it is due to residual bias in their adjusted results that would lead to an overestimate of the effect of CS on fertility (17). A recent meta-analysis study in 2013 evaluated the impact of CS on subsequent infertility and reported that CS decreased the subsequent birth rate by 11% (8); therefore, in this meta-analysis (on 18 cohort studies), which is the newest paper regarding the impact of CS on infertility, this effect was proved and the challenges about this subject are related to older papers, which had some limitations such as small sample size, confounding variables, and lack of studying any variable affecting subsequent infertility, which are factors that were considered in our study. The results of these studies are in contrast to ours, which may be due to the different sample size, different methods, and different population features.
4.1. Limitations
We included all patients with subsequent infertility during five years. 2047 patient’s records were collected, but the majority of them were excluded. Therefore, we should perform a study during 10 or 15 years in order to have larger sample sizes for epidemiological studies to be able to draw a definite conclusion about the relationship of cesarean with infertility.
4.2. Conclusions
The results of this study suggest that CS did not increase the risk of subsequent infertility when compared to vaginal delivery. Therefore, in patients who have infertility problems after the first CS, we should evaluate other reasons in order to treat it.