1. Background
In late 2019, a novel coronavirus caused a series of acute respiratory infections in Wuhan, Hubei Province, China. The disease spread rapidly, leading to an epidemic in China and other countries worldwide (1). The COVID-19 pandemic, caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has had a significant impact on global health (2, 3). Patients with end-stage renal disease on maintenance hemodialysis (ESRD-HD) represent a distinct group with characteristics that may increase their susceptibility to infection or severe disease. End-stage renal disease patients on maintenance hemodialysis patients are more likely to develop COVID-19 compared to the general population due to their weakened immune system and frequent visits to healthcare facilities. End-stage renal disease patients on maintenance hemodialysis patients require hospital stays for treatment at least three times per week and are predominantly immunocompromised due to uremia. Many of these patients are elderly and have comorbidities such as diabetes, hypertension, coronary disease, and lung disease, which are associated with poorer outcomes in COVID-19 (4, 5). Therefore, ESRD-HD patients are at higher risk for contracting COVID-19 than the general population (6, 7). Supporting this, a previous study showed that the mortality risk in patients with kidney disease was more than three times higher than in others (8). Recent studies by Oyelade et al. and Rastad et al. reported mortality rates of 53.3% and 38% in chronic kidney disease (CKD) patients, respectively (9, 10). Consistent with previous studies, the mortality rate of COVID-19 in ESRD patients is significantly higher than in the general population. This higher mortality rate may be partly explained by immune system dysfunction and a high prevalence of comorbidities such as hypertension, cardiovascular disease, and diabetes in ESRD patients. Chronic renal disease is associated with an increased risk of pneumonia and a high pneumonia-related fatality rate (11, 12). It is linked to an inflammatory status and impaired immune function. In CKD patients, the overexpression of angiotensin converting enzyme 2 (ACE2) receptors in tubular cells may contribute to the severity and worse prognosis of COVID-19 (13, 14). Lymphopenia and high LDH levels have been identified as key predictors of mortality in infected hemodialysis patients (15), potentially related to impaired immune function. Additionally, high levels of C-reactive protein (CRP), an inflammatory marker, and high AST levels, a risk factor for acute respiratory distress syndrome, have been associated with death in these patients (16). One study found that nearly one-third of hospitalized dialysis patients with COVID-19 died (17), while other research indicated that half of the dialysis patients died within 28 days of ICU admission (18). However, several studies have reported mortality among dialysis patients with COVID-19 of 20% or greater (5, 19, 20). Thus, evaluating the clinical features and severity of COVID-19 in ESRD-HD patients is crucial for understanding and accurately managing the disease.
2. Objectives
The aim of this study was to evaluate the outcomes of ESRD-HD patients hospitalized with COVID-19, and to examine the risk factors and clinical presentation associated with death in these patients. To achieve this, we conducted a propensity-matched retrospective analysis of all ESRD-HD patients admitted to Ahvaz Razi Hospital with a diagnosis of COVID-19 from February 2020 to May 2021.
3. Methods
3.1. The Study Population
In this retrospective cohort study, we examined the presentation and outcomes of COVID-19 in patients with ESRD-HD. Data were collected retrospectively from medical records of 180 ESRD-HD patients from February 2020 to May 2021. Patients aged 18 years and older with ESRD-HD and COVID-19 infection were included in the study. Exclusion criteria included insufficient information in medical records and patients who received dialysis at our center as a single session, while routinely receiving dialysis at other centers. The diagnosis and severity of COVID-19 were determined according to the guidelines for the diagnosis and treatment of COVID-19 (eighth edition).
Demographic characteristics (age, gender), comorbidities (such as diabetes, hypertension, and ischemic heart disease), clinical presentations, and laboratory results (including serum electrolytes, liver function tests [aspartate aminotransferase, alanine transaminase, alkaline phosphatase, total and direct bilirubin], complete blood count, blood sugar, uric acid, albumin, lactate dehydrogenase, creatine phosphokinase, coagulation factors, troponin, erythrocyte sedimentation rate, C-reactive protein, D-dimer, ferritin, and procalcitonin) were extracted from the patients' electronic medical records. Disease outcomes included the duration of hospitalization, ICU admission, mechanical ventilation, the need for and frequency of hemodialysis, and in-hospital mortality.
3.2. Statistical Analysis
Data were analyzed using Statistical Package for the Social Sciences (SPSS) version 26. Quantitative data with normal and non-normal distributions were described using mean/standard deviation and median/interquartile range, respectively. Qualitative data were described as frequency and percentage. t-tests and chi-square tests were used to determine the relationship between ICU admission and factors such as age, gender, and underlying disease. Logistic regression was used to identify predictors of in-hospital mortality. A P-value of less than 0.05 was considered significant. The ethics committee of Ahvaz Jundishapur University of Medical Sciences approved this study.
4. Results
4.1. Patient Characteristics and Clinical Data
A total of 180 patients with ESRD-HD who were hospitalized for COVID-19 were included in this study. The median age of the patients was 61.5 years (interquartile range 17.75 years; minimum and maximum ages were 22 and 87 years, respectively). Of these patients, 118 (65.6%) were men and 62 (34.4%) were women.
Among the patients, 82 (45.6%) had diabetes mellitus, 146 (81.1%) had hypertension, 12 (6.7%) had ischemic heart disease, and 22 (12.2%) had other underlying conditions. The most common presenting symptom was shortness of breath (70.6%), followed by cough (47.8%), fever (32.2%), myalgia (28.9%), and weakness (23.3%) (Table 1).
| Variables | No. (%) |
|---|---|
| Cough | 86 (47.8) |
| Shortness of breath | 127 (70, 6) |
| Myalgia | 52 (28.9) |
| Weakness | 42 (23.3) |
| Fever | 58 (32.2) |
| Loss of appetite | 18 (10) |
| Nausea | 14 (7.8) |
| Vomiting | 14 (7.8) |
| Chest pain | 2 (1.1) |
Table 2 shows the laboratory findings upon admission for patients with ESRD-HD and COVID-19. Elevated levels of creatine phosphokinase (median [IQR]: 18), lactate dehydrogenase (322.75), uric acid (1.42), PT time (3), and C-reactive protein (37.25) were observed in patients with ESRD-HD and COVID-19 admitted to Ahvaz Razi Hospital.
| Variable | Median (Interquartile Range) |
|---|---|
| White blood cells | 6500 (8425) |
| Lymphocytes | 865 (977) |
| Platelet | 184000 (74500) |
| Prothrombin time | 13 (3) |
| Partial thromboplastin time | 34.5 (19.75) |
| International Normalized Ratio | 1.2 (0.42) |
| Lactate dehydrogenase | 648.5 (322.75) |
| Creatine phosphokinase | 90.5 (18) |
| Erythrocyte sedimentation rate | 50 (60) |
| C-Reactive Protein | 41.5 (37.25) |
| Total bilirubin | 0.9 (0.6) |
| Direct bilirubin | 0.2 (0.1) |
| Aspartate aminotransferase | 43.5 (27) |
| Alanine Transaminase | 19 (22.5) |
| Blood sugar | 174.5 (118.75) |
| Uric acid | 7.45 (1.42) |
| D-dimer | 0.65 (0.6) |
| Procalcitonin | 1.2 (0.4) |
| Ferritin | 110 (58.25) |
| Albumin | 3.8 (1.05) |
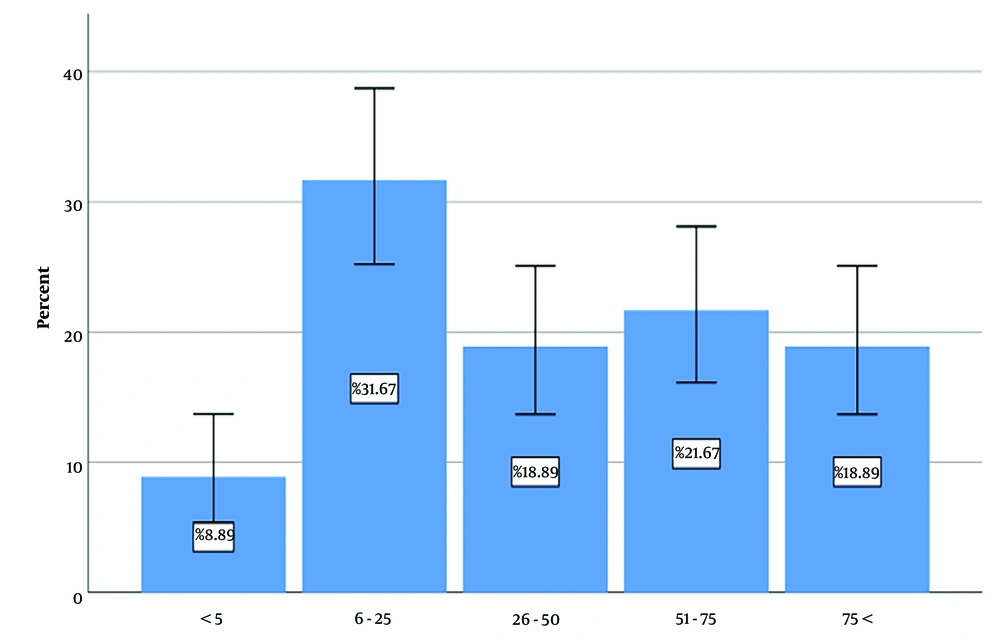
Most patients had 6 to 25% pulmonary involvement (Figure 1). The most common pattern of pulmonary involvement was diffuse, observed in 77 (42.8%) patients. The median length of hospital stay was 9 days (interquartile range 7, minimum 2, maximum 29 days). Seventy-five (41.66%) patients were admitted to the ICU, with a median length of stay of 5 days (interquartile range 5, minimum 1, maximum 26 days). In univariate analysis, admission to the ICU was significantly associated with underlying hypertension and ischemic heart disease (P-values 0.008 and 0.015, respectively) but was not significantly related to age, sex, or underlying diabetes mellitus (P-values 0.099, 0.185, and 0.800, respectively). All patients underwent hemodialysis during hospitalization, with a median of 2 sessions (interquartile range 1, minimum 1, maximum 14). Sixty-two patients (34.4%) required mechanical ventilation, with a median duration of 4 days (interquartile range 6, minimum 1, maximum 26 days).
4.2. Treatment Scheme
The most prescribed drugs for patients after heparin (171 patients, 95%) and pantoprazole (135 patients, 75%) were dexamethasone (75 patients, 41.7%), followed by chloroquine (41 patients, 22.8%), famotidine (39 patients, 21.7%), atazanavir (38 patients, 21.1%), and interferon (35 patients, 19.4%).
4.3. Clinical Evolution and Outcomes
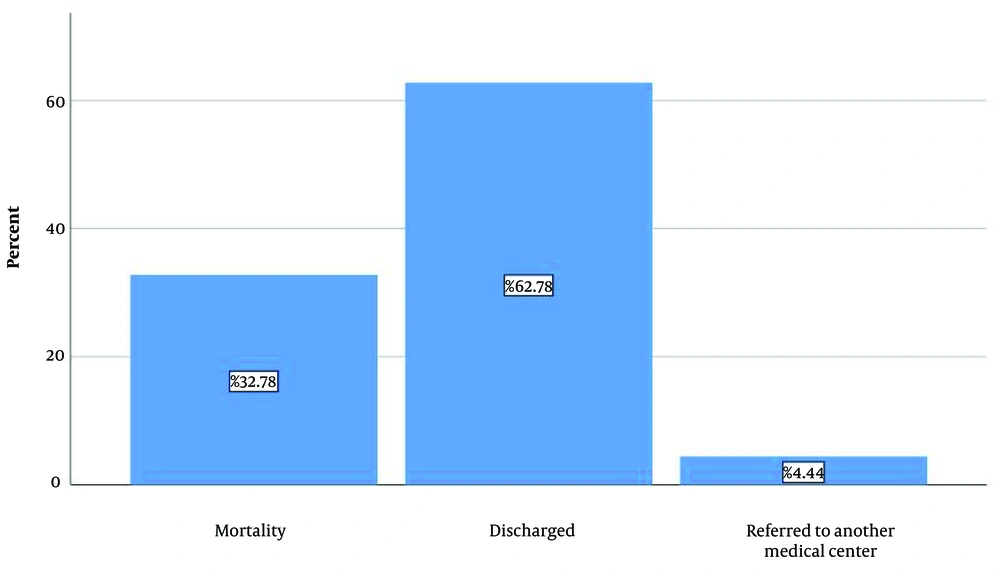
One hundred thirteen patients (62.8%) were discharged, 8 (4.4%) were referred to another medical center, and 59 (32.8%) died (Figure 2).
As shown in Table 3, logistic regression analysis was used to investigate independent factors predicting mortality in patients. According to the results, advanced age, fever, shortness of breath, cough, and the need for mechanical ventilation were significantly associated with in-hospital mortality in ESRD-HD patients with COVID-19.
| Variables | P-Value |
|---|---|
| Older age | 0.016 |
| Fever | 0.033 |
| Shortness of breath | 0.001 |
| Cough | 0.012 |
| Mechanical ventilation | 0.011 |
5. Discussion
In this retrospective observational study, we investigated the outcomes of ESRD-HD patients hospitalized with COVID-19. According to multivariate analysis, older age, fever, shortness of breath, cough, and the need for mechanical ventilation were significant predictors of in-hospital mortality in ESRD-HD patients with COVID-19. Epidemiological research indicates that older adults or patients with chronic diseases are more susceptible to COVID-19 infection and adverse outcomes (21). End-stage renal disease patients on maintenance hemodialysis patients are particularly vulnerable to severe forms of COVID-19 due to their older age and high prevalence of comorbidities such as diabetes and hypertension. Their altered immune systems and frequent hospital visits further increase their risk of viral infections (5). Among ESRD-HD patients, those receiving in-center hemodialysis are at higher risk of COVID-19 infection compared to those undergoing home dialysis (17).
We studied 180 ESRD patients with COVID-19. The average age of the patients was 61.5 years, with 65.6% being men. Hypertension was the most common underlying condition, affecting 81.1% of the patients. The background characteristics of the patients in our study are consistent with other studies. For instance, Min et al. reported 54% female patients, whereas Xiong et al. found 57.3% male patients. Both studies, similar to ours, noted an average patient age between 61 and 66 years, with hypertension being the most common underlying condition (21-23). In contrast, Greene et al. reported an average age of 35 to 40 years from a study involving approximately 20,000 patients, with hypertension being less common than in ESRD patients (24). This discrepancy may be attributed to differences in sample size.
In our study, the most common clinical presentation was shortness of breath (70.6%), followed by cough (47.8%) and fever (32.2%) (25). These findings are consistent with other studies, where shortness of breath, fever, weakness, and cough were commonly observed (21, 23, 26), similar to the symptom prevalence in non-ESRD COVID-19 patients (27). Alimohamadi et al. reported that in the general population, common symptoms of COVID-19 included fever, cough, weakness, and shortness of breath (28). Faes et al. found that the length of hospitalization increased with age: About 3 days for the youngest group, about 5 days for working-age individuals, and about 9 days for those over 60. ICU stay averaged 4 days for the young age group and 6 days for the elderly (29). Given that the average age of ESRD-HD patients with COVID-19 is around 60 years, the average duration of hospitalization and ICU admission in this group is expected to be higher compared to the general population, aligning with the values for their age group. In our study, the average hospital stay was 9 days (ranging from 2 to 29 days), and the average ICU stay was 5 days. The prevalence of ICU admission in our study (41.66%) is higher than in other similar studies (approximately 20%) (30, 31). This difference may be due to varying patient characteristics and different COVID-19 strains. A meta-analysis revealed that the prevalence of ICU admission for COVID-19 patients across 37 studies ranged from 3% to 100% (32).
In our study, the in-hospital mortality rate was 32.8%, which is comparable to findings in similar studies. For example, one study reported that nearly one-third of hospitalized ESRD-HD patients with COVID-19 died (17). Another study found that half of dialysis patients died within 28 days of admission to the ICU (18). Overall mortality among dialysis patients with COVID-19 has been reported to be at least 20% in three large studies (5, 19, 20). A meta-analysis by Alimohamadi et al. reported a mortality rate of 10% for the general population of COVID-19 patients. The higher mortality rate in the ESRD-HD population compared to the general population can be attributed to their higher average age and increased comorbidities. Alimohammadi et al.'s study indicated that the mortality rate in elderly patients is higher than in the general population (19% versus 10%) (33).
This study was conducted retrospectively, which presents limitations in adjusting for many possible confounding variables. This limitation may affect the comprehensiveness of the study findings. Due to the retrospective nature of this study, we could not gather pre-hospital status, including nutritional status and all relevant laboratory tests, for patients who died in-hospital. Additionally, we could not account for the confounding effects of drugs used for COVID-19 treatment during hospitalization, as some antiviral drugs may cause renal tubular dysfunction. We also lack data regarding treatment regimens and the use of renin-angiotensin-aldosterone system antagonists during the hospital stay.
5.1. Conclusions
Our study demonstrated that ESRD-HD patients with COVID-19 are at a higher risk for ICU admission and in-hospital mortality. Advanced age, fever, shortness of breath, cough, and the need for mechanical ventilation were significantly associated with in-hospital mortality in these patients.