1. Background
The escalating prevalence of diabetes mellitus (DM) has become one of the top global public health challenges of the 21st century (1). The number of people living with DM is estimated to double, from 529 million in 2021 to approximately 1.3 billion by 2050 (2). As reported by the Iranian National Institute of Health Research (INIHR) in 2021, the prevalence of this condition in adults over 18 years old in Iran is projected at 14.15%, representing a 45.5% increase compared to 2016 (3). Diabetes mellitus patients are prone to multiple complications, including retinopathy, nephropathy, neuropathy, and cardiovascular diseases, which need to be minimized over time (4).
Health behavior theories often emphasize raising public knowledge as a key element in changing health-related behavior and achieving better outcomes (5, 6). Consequently, healthy lifestyle education (HLSE) programs aim to help DM patients acquire knowledge, skills, and empowerment for self-care (7). One accessible approach is peer education, where trained DM patients support others with the same condition in managing their disease (8). A systematic review by Madmoli et al. demonstrated the significant impact of peer education on improved self-care in DM patients (9).
Another cost-effective, comprehensive strategy for chronic patient education is utilizing virtual education methods via mobile-based apps (10, 11). Virtual education refers to a learning environment where teachers and learners are connected at different times and locations, and sometimes simultaneously. Educational materials are delivered through information technology apps, multimedia resources, the Internet, and video conferences (12, 13). This creates an excellent opportunity for teaching and learning beyond geographical boundaries, eliminating the need to physically attend classroom sessions (14, 15). Recently, mobile apps have been widely used in both developed and developing countries due to their potential to provide personalized medical recommendations (16). According to figures published by BankMyCell on January 9, 2024, 85.74% of people worldwide use mobile devices. This indicates that mobile devices are an ideal platform for virtual education (17, 18), as mobile-based apps offer patients continuously updated and accessible educational content (19).
Research has shown that individuals with higher levels of self-esteem tend to engage in better self-care, achieve a higher quality of life (20, 21), and experience more success in modifying lifestyle factors such as nutrition, physical activity, and stress management (22-24). Self-esteem reflects one's ability to adapt to life's challenges and find happiness in achieving effectiveness (25). It also involves positive or negative self-evaluation or the extent to which individuals perceive themselves as worthy. This can develop in relation to others or independently (26, 27). Chronic stress associated with long-term health conditions can significantly reduce patients' self-esteem (28). Previous studies have reported varying results regarding the effects of education delivered through peer groups and the mHealth app (29, 30).
A review of credible databases revealed no study comparing the effects of two comprehensive educational methods—peer education and virtual education via mobile apps—on patients with DM. Therefore, exploring the impact of HLSE through these two approaches on patients' self-esteem represents an innovation in the present study.
2. Objectives
This research compared the effects of HLSE using peer education and virtual education via interactive virtual sessions and the mobile-based mHealth app on self-esteem in patients with type 2 diabetes mellitus (T2DM).
3. Methods
3.1. Study Design
This three-group randomized controlled trial was completed in 2022 and registered on October 6, 2021, on the Iranian Registry of Clinical Trials (No. IRCT20210808052115N1).
3.2. Participants and Study Setting
Based on a comparable study's (31) mean and standard deviation values, a 95% confidence interval, and 90% test power, the sample size was calculated to be 41 participants per group. To account for a 10% attrition rate, 45 patients with T2DM were examined in each group, calculated as follows:
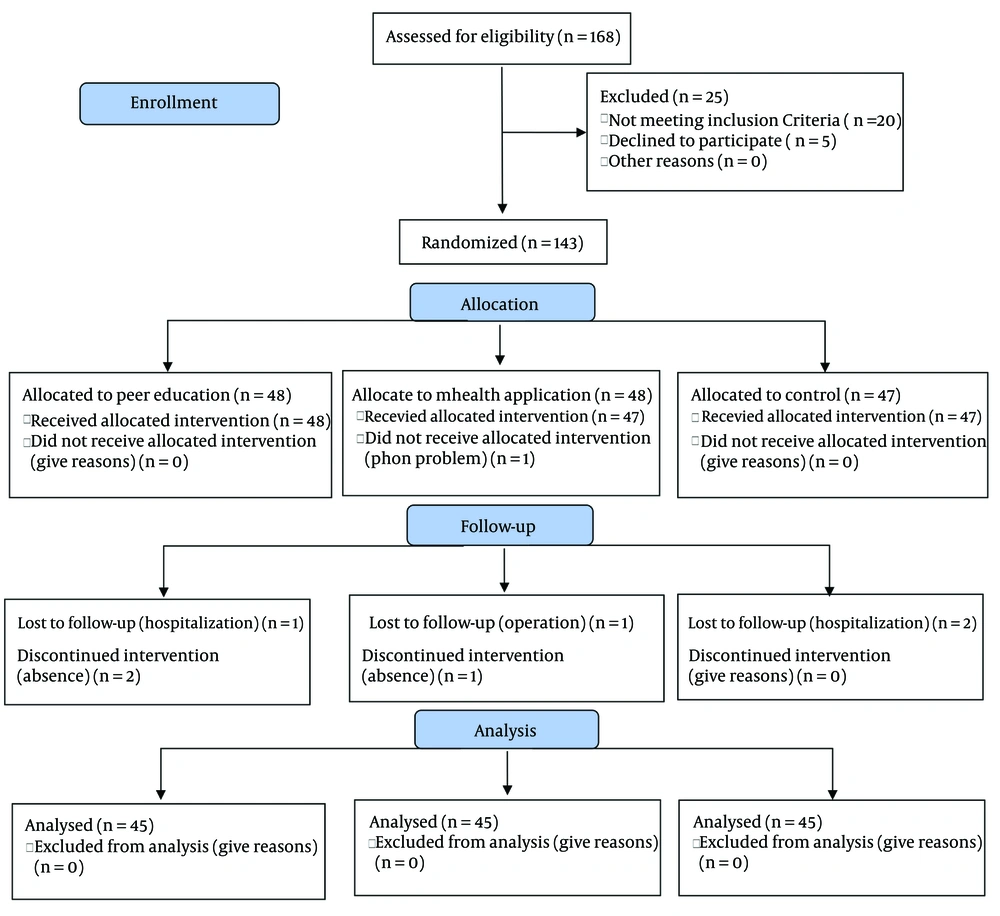
This study was conducted from July to December 2022 at two selected hospitals in Kermanshah Province, Iran. A total of 168 patients with T2DM were recruited using purposive sampling. Of these, 20 patients did not meet the inclusion criteria, and five individuals declined to participate in the study. Out of the remaining 143 patients, 48 were placed in the peer education group, 48 were assigned to the virtual education group (using interactive virtual sessions via a mobile-based app, mHealth), and 47 were selected for the control group.
During the study, one patient from the virtual education group dropped out due to a technical problem with their mobile device, one was removed due to surgery, and another was excluded for missing the virtual education sessions. In the peer education group, one patient was excluded due to hospitalization, and two others were removed for not attending the educational sessions. In the control group, two patients were excluded following hospitalization. Ultimately, data from 45 patients in each study group were analyzed (Figure 1).
Replacement randomization was employed to assign patients to the study groups, ensuring that each patient had an equal probability of being included in one of the three groups. A randomized block design was used, with six patients randomly assigned to each block. The groups were labeled A, B, and C. Each block of six patients was formed by randomly assigning them to the groups. For example, in the first week, if the block sequence was ABCCAB, patients were placed into the groups accordingly. In the first week, patients were assigned to group C, group A, and so on. During the second week, patients were assigned to the peer education group B, and in the third week, they were included in the virtual education group C. This blocking process continued until the required sample size was reached.
The inclusion criteria were as follows: The patient's willingness to participate in the study, a diagnosis of uncontrolled T2DM (fasting blood sugar levels above 126 mg/dL) (32) for at least six months prior to the study, being between the ages of 21 and 75 (33), literacy and proficiency in the Persian language, access to a mobile device and the internet (with the ability to use them and install apps), the ability to make direct phone calls with the patient or their family members, absence of cognitive impairments or physical disabilities, no need for diabetic foot surgery, and no hearing or vision problems. Additionally, patients could not have a background in medical education or recent participation in educational programs for DM management within the past six months.
The exclusion criteria included physical disabilities that hindered self-care, reluctance to continue the study, and not using the specified app.
3.3. Data Collection
The data were collected using the Patient Profile Form, which included information about age, gender, educational attainment, income, head of family, caregiver, presence of hypertension, hyperlipidemia, kidney diseases, unhealed wounds, and a history of DM in first-degree relatives. The Self-Report Rosenberg’s Self-Esteem Scale (RSES) was used to assess patients’ self-esteem. The RSES was completed by the patients before and two months after the intervention program.
The RSES, designed by Rosenberg in 1965, is one of the most commonly used tools to measure overall self-esteem (34). This 10-item questionnaire consists of five positive and five negative statements, rated on a four-point Likert scale, ranging from completely disagree (0) to completely agree (3). The total scores range from 0 to 30. Positive statements include items 1 to 5, while negative statements include items 6 to 10. The scores are categorized into three levels of self-esteem: Low (below 17), moderate (17 - 21), and high (above 21) (35).
The internal consistency of the RSES has been widely validated in studies worldwide, with a reported coefficient of 0.84, and its test-retest reliability within two weeks was also 0.84. In domestic studies, the reliability values of the RSES, measured using Cronbach’s alpha, test-retest, and split-half reliability coefficients, were reported as 0.69, 0.78, and 0.68, respectively (34). In Rajabi et al.’s (as cited by Kariminejad) study of the Iranian population, the internal consistency coefficient was reported to be 0.84 (36). The Cronbach’s alpha coefficient for this scale in the present study was 0.78.
3.4. Intervention Program
Three patients with T2DM were initially selected from the list provided by both hospitals in Kermanshah Province, Iran. These patients did not have chronic complications of DM, such as kidney failure, blindness or acute vision loss, diabetic foot ulcers, or amputations. Their glycosylated hemoglobin (HbA1c) levels were also within the normal range. The researchers trained these peer educators in person for two hours using the lecture method. The educational materials were prepared according to the patients' needs, and peers received small gifts as tokens of appreciation after completing the educational sessions.
Initially, all patients in the study groups completed the patient profile form and the RSES. The patients in the peer education group were then divided into three subgroups of 15. The researchers contacted them by phone to invite them to attend the educational sessions. Each subgroup participated in four 35-minute face-to-face sessions over two days, led by their peer educators under the supervision of the researchers. During these sessions, the peers shared their experiences, teaching participants how to increase self-esteem and manage their diabetes more effectively.
For the patients in the virtual education group, the researchers provided educational materials designed to boost self-esteem in patients with DM via a social messaging app. The app allowed for interactive communication, including a question-and-answer feature. Once the app was successfully installed on the patients' mobile devices, a message was sent to each patient announcing the start of the educational program and providing instructions on how to participate in the sessions.
The educational materials were delivered over three sessions, held every other day for a week through the social messaging app. These sessions included audio slides prepared in Microsoft PowerPoint, video clips, and text and audio files shared via the app. The content covered topics such as an introduction to DM, diagnosis modes, symptoms, lifestyle modifications, mental and spiritual health, physical activity, diet, self-confidence, and coping strategies. The technical and educational content of the app was approved by four faculty members from the School of Nursing at Aja University of Medical Sciences in Tehran, Iran. Participants could easily log in to the app to access the educational materials, and their participation was monitored by their usernames. Researchers also sent reminders to the patients to review the educational materials during each session.
It is important to note that the educational materials provided to both the peer education group and the virtual education group were the same. To prevent patients from other groups from accessing the app's educational content before the end of the study, a login password was implemented for the virtual education group. All patients, regardless of group, received routine healthcare services from physicians and nurses at the selected hospitals. After the study was completed, the educational materials were also provided to the patients in the control group. The statistical analyst was blinded to the random assignment of the patients into groups A, B, and C.
3.5. Data Analysis
The data were analyzed using IBM SPSS Statistics software. Descriptive statistics (mean, standard deviation, frequency, percentage) and analytical tests (paired-sample t-test, chi-square test, Fisher’s exact test, and one-way ANOVA) were used. The Kolmogorov-Smirnov test confirmed the normality of the variables, and a significance level of P > 0.05 was considered.
3.6. Ethical Considerations
This study was approved by the Research Ethics Committee of Aja University of Medical Sciences (IR.AJAUMS.REC.1400.131), Tehran, Iran, and registered on the Iranian Registry of Clinical Trials (No. IRCT20210808052115N1). The declaration of Helsinki provisions were followed, and written informed consent was obtained from all participants. Confidentiality, voluntary participation, and the right to withdraw from the study were ensured.
4. Results
The mean age of the patients with T2DM was 40.22 ± 11.50 years (range: Twenty-one to 65), and they had been diagnosed with DM for an average of 51 ± 42.04 months (range: Nine to 346 months). Most participants (53.3%) were male, and 67.4% had educational attainment higher than elementary school. About 60% of the patients reported having adequate income. Most patients (40.7%) were married and had children, and more than half (56.3%) were the head of their families. The majority had hyperlipidemia (43%), hypertension (54.1%), kidney diseases (58.5%), and vision loss or unhealed wounds (63%). The most common disease among their first-degree relatives was DM (48.9%). No significant differences were found among the study groups in terms of patient characteristics (P > 0.05) (Table 1).
| Groups | Peer Education a | Virtual Education a | Control a | Statistic | df | P-Value |
|---|---|---|---|---|---|---|
| Individual characteristics | ||||||
| Gender | 1.25 b | 2 | 0.535 | |||
| Male | 21 (46.7) | 26 (57.8) | 25 (55.6) | |||
| Female | 24 (53.3) | 19 (42.2) | 20 (44.4) | |||
| Level of education | -7.448 b | 4 | 0.114 | |||
| Informal literate | 6 (13.3) | 2 (4.4) | 4 (8.9) | |||
| Elementary | 12 (26.7) | 6 (13.3 | 14 (31.1) | |||
| Above elementary | 27 (60) | 37 (82.2) | 27 (60) | |||
| Income | 6.12 b | 4 | 0.192 | |||
| High | 13 (28.9) | 11 (24.4) | 11 (24.4) | |||
| Moderate | 25 (55.6) | 23 (51.1) | 31 (68.9) | |||
| Low | 3 (14.6) | 11 (24.4) | 3 (6.7) | |||
| Head of family | 1.84 b | 4 | 0.800 | |||
| The patient | 22 (48.9) | 27 (60) | 27 (60) | |||
| Spouse | 21 (46.7) | 16 (35.6) | 17 (37.8) | |||
| Children | 2 (4.4) | 2 (4.4) | 1 (2.2) | |||
| A person caring for the patient | 28.67 c | 10 | 0.236 | |||
| Single | 6 (13.3) | 3 (6.7) | 1 (2.2) | |||
| With wife | 24 (53.3) | 10 (22.2) | 14 (31.1) | |||
| Wife and children | 13 (28.9) | 25 (55.6) | 17 (37.8) | |||
| With children | 2 (4.4) | 0 (0) | 3 (6.7) | |||
| With parents | 0 (0) | 6 (13.3) | 10 (22.2) | |||
| Other cases | 0 (0) | 1 (2.2) | 0 (0) | |||
| Hyperlipidemia | 0.911b | 4 | 0.923 | |||
| Yes | 22 (48.9) | 19 (42.2) | 17 (39.5) | |||
| No | 17 (37.8) | 20 (44.4) | 20 (46.5) | |||
| Unknown | 6 (13.3) | 6 (13.3) | 6 (14) | |||
| Hypertension | 3.84 b | 4 | 0.429 | |||
| Yes | 22 (48.90 | 16 (35.6) | 13 (29.5) | |||
| No | 20 (44.40) | 26 (57.8) | 27 (61.4) | |||
| Unknown | 3 (6.7) | 3 (6.3) | 4 (9.1) | |||
| Kidney disease | 33.794 b | 6 | 0.366 | |||
| Yes | 11 (24.4) | 3 (6.7) | 16 (35.6) | |||
| No | 17 (37.8) | 40 (88.9) | 22 (48.9) | |||
| Unknown | 16 (35.6) | 2 (4.4) | 7 (15.6) | |||
| Unhealed wound | 14.03 b | 4 | 0.273 | |||
| Yes | 6 (13.3) | 5 (11.1) | 9 (20) | |||
| No | 21 (46.7) | 34 (75.6) | 30 (66.7) | |||
| Unknown | 18 (40) | 6 (13.3) | 6 (13.3) | |||
| The most important disease of first-degree relatives c | 12.11c | 10 | 0.248 | |||
| Blood pressure | 4 (9.1) | 8 (25.8) | 10 (22.2) | |||
| Diabetes | 28 (63.6) | 46 (51.6) | 22 (48.9) | |||
| Blood fat | 8 (18.2) | 6 (19.4) | 10 (22.2) | |||
| Kidney disease | 4 (9.1) | 0 (0) | 2 (4.4) | |||
| Unhealed wound | 0 (0) | 0 (0) | 1 (2.2) | |||
| Retinopathy | 0 (0) | 1 (3.2) | 0 (0) |
Comparison of Individual Characteristics of Patients with Diabetes in Peer Education, Virtual Education, and Control Groups
Before the intervention, there was no significant difference in the RSES mean scores between the study groups (P = 0.665). However, post-intervention, the RSES mean scores in the virtual education group were significantly higher than those in the other two groups (P = 0.002). The RSES mean scores in the peer education group after the intervention did not differ significantly from the pre-intervention stage (P = 0.067), while the virtual education group using the mHealth app showed a significant increase in scores (P = 0.001). There was no significant difference in the RSES mean scores in the control group before and after the intervention (P = 0.960) (Table 2).
| Variables and Stage | Peer Education | Virtual Education | Control | F | df | P-Value |
|---|---|---|---|---|---|---|
| Self-esteem | ||||||
| Pre-intervention | 16.66 (3.45) | 17.24 (3.43) | 16.48 (5.35) | 0.410 | 2 | 0.665 |
| Post-intervention | 17.78 (3.73) | 22.09 (3.37) | 16.47 (4.65) | 24.941 | 2 | 0.001 a |
| Paired t-test statistics, df, P-value | t = -1.879, df = 44, P = 0.067 | t = -9.850, df = 44, P = 0.001 a | t = 0.050, df = 44, P = 0.960 | - | - | - |
Comparison of the Mean Self-esteem Score of Diabetics Before Training and After Training in Three Groups
Post-hoc test results revealed that the RSES mean scores in the peer education group after the HLSE program did not significantly differ from the control group (P = 0.118). However, a significant difference was observed between the mean RSES scores of the patients with T2DM in the peer education group and those in the virtual education group using the mHealth app after the intervention, with the scores being significantly higher in the virtual education group (P = 0.001). Additionally, the RSES mean scores of the patients in the virtual education group were significantly higher than those in the control group following the completion of the HLSE program (P = 0.001) (Table 3). The overall effect size of the intervention on the patients' self-esteem was 0.61.
Comparison of the Mean Difference in Self-esteem of Patients with Diabetes After Intervention in the Peer Education, mHealth, and Control Groups
5. Discussion
This study compared the effects of HLSE through peer education and virtual education using the mHealth app on self-esteem in patients with T2DM. Both methods positively impacted self-esteem, with the overall effect size being moderate to high. However, virtual education via the mHealth app had a more significant effect on self-esteem than peer education. Trento et al. reported that self-management training and psychological support significantly improved self-esteem in patients with type 1 DM (37). Similarly, Poorgholami et al. found that self-care education boosted self-esteem in hemodialysis patients (38). Fallah et al. also noted that family-centered education significantly elevated self-esteem in patients with T2DM compared to patient-centered education (39).
These findings are consistent with the current study's results, although peer education in this study did not significantly enhance self-esteem in patients with T2DM, which may be attributed to differences in educational methods and study populations. Abd-alrazaq et al. concluded that using mobile apps was more efficient and convenient than traditional methods for communication between healthcare workers and patients (40), aligning with this study’s findings. Molavynejad et al. also showed that tele-education was more effective than in-person education for dietary regimen compliance in patients with T2DM (30).
On the other hand, an interventional study investigating the effects of a structured education program demonstrated no significant change in self-esteem in the intervention group (41). A systematic review by Drew et al. similarly found that lifestyle interventions had only a slight impact on self-esteem in men (42). These discrepancies may be due to differences in the populations examined, as the current study involved patients with T2DM, while Drew et al.'s (42) study involved mentally healthy men. The findings confirm that virtual education via online interactive classroom sessions and a mobile-based app, like mHealth, is more effective than peer education in improving self-esteem in patients with T2DM.
5.1. Limitations and Strengths
One limitation of this study was the potential for patients in the intervention and control groups to share educational materials, particularly in the virtual education group. To mitigate this, patients were asked not to share the content until the end of the study. A key strength of the study was the simultaneous comparison of two innovative educational methods. Another strength was combining virtual classroom sessions with the mobile-based mHealth app.
5.2. Conclusions
The results demonstrated that both educational methods, peer education and virtual education, positively affected self-esteem in patients with T2DM. However, the effectiveness of virtual education using a mobile-based app (mHealth) on self-esteem was more pronounced than that of peer education. These findings provide valuable insights into the optimal use of distance education and educational apps. Since virtual education and apps allow for flexible learning at different times and locations, and learners can repeatedly access the materials to achieve mastery of the content, these innovative, comprehensive methods are highly recommended for managing chronic conditions such as DM. It is further suggested that future studies investigate the impact of virtual education via mobile-based apps and artificial intelligence capabilities on self-esteem in other patient populations.