1. Background
Diabetes mellitus is recognized as a major global public health problem, especially in developing countries (1). According to the International Diabetes Federation, in 2019, 463 million people aged 20 - 79 had diabetes, and this number is expected to exceed 552 million by 2030 (2). In Iran, the prevalence of diabetes is also rising, with recent studies indicating that approximately 14% of the adult population is affected, and 100,000 new cases are added each year (3). The increasing trend of diabetes in developing countries has created significant medical and economic challenges (4). Diabetes causes dysfunction in blood vessels and affects the structure of various body tissues, leading to complications such as retinopathy, nephropathy, and neuropathy (as microvascular complications) and ischemic heart disease, stroke, and peripheral vascular disease (as macrovascular complications) (5, 6).
Poor glycemic control is a critical factor in the development and progression of these complications, and it is ultimately responsible for many diabetes-related deaths. Intensive glycemic control is crucial for preventing diabetes complications (7, 8). Monitoring glycemic levels not only helps evaluate the effectiveness of treatment but also provides the opportunity to adjust lifestyle and medication to achieve optimal glycemic control (9). Hemoglobin A1c (HbA1c), the most commonly used glycemic biomarker, provides an objective measure of glycemic control over the previous 8 - 12 weeks (10). The American Diabetes Association (ADA) recommends an HbA1c target of < 7% for most patients with type 2 diabetes mellitus (T2DM) to reduce the risk of complications (11).
Despite the well-established importance of glycemic control, studies indicate that many T2DM patients do not achieve the recommended HbA1c targets. According to a survey conducted in 49 developing countries, glycemic control remained suboptimal in people with type 2 diabetes over a 12-year period (12). A systematic review by Gebreyohannes et al. found that only 33.2% of patients with T2DM attained HbA1c < 7% (13). In Iran, the rate of very good glycemic control has been reported to range between 23.1% and 56% among people with diabetes (14, 15). The reasons for suboptimal glycemic control in T2DM patients are complex and multifactorial. Several patient-related factors have been associated with poor HbA1c control, including younger age, male gender, poor knowledge of diabetes, lower education status, longer diabetes duration, improper insulin injection, and the presence of diabetes complications (16-18).
Identifying characteristics of patients who achieve glycemic control can guide future interventions aimed at improving diabetes care and reducing complications. Although previous studies in Iran have examined sociodemographic and clinical predictors of HbA1c control, such as age, education level, income, diabetes duration, and treatment type, the results of these studies have not always been consistent (19-21). Given the ethnic differences in the epidemiology of diabetes, findings from one population may not be generalizable to others (22).
2. Objectives
Therefore, to address this gap, the present study was designed to identify demographic and clinical factors associated with achieving HbA1c targets in patients with T2DM at the Yazd Diabetes Center in Iran.
3. Methods
This retrospective study analyzed data from the Yazd Diabetes Center, a specialty clinic in Yazd, Iran. Data were extracted from the medical records of 3,454 patients who visited the clinic between March 2020 and December 2022. The electronic records contained both demographic information (age, gender, education) and clinical information (age at diagnosis, type of diabetes, blood pressure), as well as results from medical tests performed during each visit. The study population consisted of adults aged 18 years or older with a diagnosis of T2DM who had at least two recorded HbA1c values per year. Patients with type 1 diabetes or gestational diabetes were excluded from the study.
3.1. Data Analysis
The statistical analysis involved bivariate comparisons using chi-squared tests for categorical variables and t-tests or Mann-Whitney U tests for continuous variables. Multivariable logistic regression was used to identify predictors of achieving HbA1c levels < 7%, adjusting for various covariates. Initially, a model was fit to include interaction effects between gender and age, as well as gender and diabetes duration. However, the interaction term between age and diabetes duration was removed as it was not supported by the data (P = 0.22). The final logistic regression model included gender, age, education level, diabetes duration, and the interaction between gender and diabetes duration as predictors. The model, fitted using R version 4.2.0, provided adjusted odds ratios and profile-likelihood 95% confidence intervals for each predictor.
3.2. Ethical Considerations
This project was approved by the ethics committee of Shahid Sadoughi University of Medical Sciences, Yazd, Iran. (No: IR.SSU.REC.1400.143).
4. Results
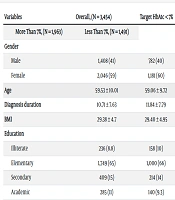
Our analysis included 3,454 patients with type 2 diabetes, focusing on the likelihood of maintaining HbA1c levels below 7%. The cohort was predominantly female (59%) and primarily educated at the elementary level (65%), with an average age of 59.5 years (SD = 10) and a mean diabetes duration of 10.7 years (SD = 7.6). Additionally, 77% of the patients had a family history of diabetes, and the average BMI was 29.38 (SD = 4.7). Approximately 43.2% (1,491) of the patients achieved the HbA1c target (Table 1).
| Variables | Overall, (N = 3,454) | Target HbA1c < 7% | P-Value b | |
|---|---|---|---|---|
| More Than 7%, (N = 1,963) | Less Than 7%, (N = 1,491) | |||
| Gender | 0.20 | |||
| Male | 1,408 (41) | 782 (40) | 626 (42) | |
| Female | 2,046 (59) | 1,181 (60) | 865 (58) | |
| Age | 59.53 ± 10.01 | 59.06 ± 9.72 | 60.15 ± 10.34 | < 0.001 |
| Diagnosis duration | 10.71 ± 7.63 | 11.84 ± 7.79 | 9.24 ± 7.15 | < 0.001 |
| BMI | 29.38 ± 4.7 | 29.40 ± 4.95 | 29.36 ± 4.49 | 0.90 |
| Education | < 0.001 | |||
| Illiterate | 236 (8.8) | 158 (10) | 78 (6.7) | |
| Elementary | 1,749 (65) | 1,000 (66) | 749 (64) | |
| Secondary | 409 (15) | 214 (14) | 195 (17) | |
| Academic | 285 (11) | 140 (9.3) | 145 (12) | |
| Family history of diabetes | ||||
| Yes | 1649 (77) | 957 (58.04) | 692 (41.96) | 0.87 |
| No | 480 (23) | 292 (60.84) | 188 (39.16) | |
a Values are expressed as No. (%) or mean ± SD.
b Pearson's chi-squared test; Wilcoxon rank sum test.
In the multivariable logistic regression model (Table 2), education was a significant predictor of achieving HbA1c < 7%. Compared to the illiterate group, those with elementary education had 40% higher odds (B = 0.34, OR = 1.40, P = 0.031), secondary education increased the odds by 94% (B = 0.664, OR = 1.94, P < 0.001), and academic education more than doubled the odds (B = 0.834, OR = 2.30, P < 0.001). Gender differences were notable, particularly in newly diagnosed patients; females had a 47.3% higher probability of achieving HbA1c < 7% compared to males at the time of diagnosis, holding other variables constant.
| Characteristic | OR (95% CI) | P-Value |
|---|---|---|
| Age | 1.03 (1.02 to 1.04) | < 0.001 |
| Gender | ||
| Male | - | |
| Female | 1.47 (1.11 to 1.96) | 0.008 |
| Diagnosis duration | 0.96 (0.94 to 0.97) | < 0.001 |
| Education | ||
| Illiterate | - | |
| Elementary | 1.40 (1.03 to 1.92) | 0.031 |
| Secondary | 1.94 (1.35 to 2.82) | < 0.001 |
| Academic | 2.30 (1.55 to 3.44) | < 0.001 |
| Gender × diagnosis duration | ||
| Female × diagnosis duration | 0.97 (0.95 to 0.99) | 0.011 |
Abbreviations: OR, odds ratio; CI, confidence interval.
a Null deviance = 3,482; Null df = 2,539; Log-likelihood = -1,666; AIC = 3,348; BIC = 3,394; Deviance = 3,332; Residual df = 2,532; No. Obs. = 2,540.
The interaction term revealed that each additional year of diabetes duration led to a 3% greater reduction in the odds of achieving HbA1c < 7% for females compared to males (B = -0.029, OR = 0.97, P = 0.011), indicating gender-specific impacts of diabetes duration. For males, each additional year decreased the odds by 4% (B = -0.045, OR = 0.96, P < 0.001), whereas for females, this decrease was 7% (B = -0.074, OR = 0.93). The model explained 20% of the variance in HbA1c levels. This study highlights that age, gender, duration of diabetes, and education level are crucial in managing HbA1c levels, with the interaction between gender and diabetes duration being particularly significant.
5. Discussion
The present study showed that less than half (43.2%) of T2DM patients had good glycemic control, which is higher than findings from studies conducted in India (23.4%) (23) and Ethiopia (32.6%) (24). This difference may be attributed to the impact of social determinants of health, as communities with lower income and more limited healthcare facilities tend to have poorer glycemic control (25). Compared to other countries in the Middle East region, patients in our study exhibited better glycemic control than those in Saudi Arabia (25.1%) (26) and Kuwait (34.5%) (27). The difference in these results can be linked to variations in the demographic characteristics of the research samples, such as weight and age. The mean age of participants in both of those studies was lower than in our study, and as will be discussed further, older individuals tend to have better glycemic control than younger ones, suggesting a possible learning curve in managing diabetes (28).
Additionally, the average Body Mass Index (BMI) of participants in the Kuwait study was higher than in our study (33.1 ± 6.7 vs. 29.3 ± 4.7), indicating a higher prevalence of obesity and overweight among patients with diabetes in that population. Previous research has shown that individuals with type 2 diabetes who are obese or overweight generally have poorer glycemic control (29).
In contrast, the proportion of individuals achieving optimal glycemic control in our study was lower than that reported in Germany (78.5%) (30) and Peru (60.2%) (31). The difference in achieving glycemic targets could be due to variations in lifestyle, accessibility, and the quality of medical services across different communities. A systematic review highlighted that patients' financial limitations and incomplete access to healthcare services are significant barriers to effective diabetes management (32). Overall, there remains a need to improve educational, therapeutic, and care services to achieve optimal glycemic control in diabetic patients worldwide (32, 33).
According to the results, age was one of the significant factors influencing glycemic control, with the likelihood of achieving the HbA1c target (< 7%) increasing with age (OR 1.03, P < 0.001; CI: 1.02 - 1.04). The positive effect of increasing age on improved glycemic control has also been demonstrated in previous studies conducted in Taiwan and Northwest Ethiopia (34, 35). Researchers suggest that elderly individuals with diabetes tend to be more concerned about their health than younger patients and dedicate more time to self-care, which can lead to better disease management and blood glucose control (36). Furthermore, a systematic review revealed poorer glycemic control in the very young and very old groups. Since most participants in our study fell between these age extremes, it can be inferred that as patients age, their adherence to treatment improves, which positively affects their glycemic control (37).
The results also showed that the role of gender in HbA1c control was influenced by the duration of the diabetes diagnosis. For each additional year of diagnosis, the likelihood of achieving the HbA1c target decreased by 4% for males (B = -0.045, OR=0.96, P < 0.001) and 7% for females (B = -0.074, OR = 0.93), indicating a significant difference. In other words, over time, females exhibited poorer glycemic control than males. This finding aligns with similar studies conducted in India and Western Ethiopia, which established that longer diabetes duration is a predictor of poorer glycemic control (38, 39). This can be explained by the progressive dysfunction of beta cells in insulin secretion and increased insulin resistance over time (40). As beta-cell failure progresses, patients' positive responses to diet and oral medications diminish, leading to disrupted glycemic control (26).
Gender differences in glycemic control have been well-documented in multiple studies. Research conducted in Brazil, Venezuela (41), Iraq (42), and Yemen (43) found better glycemic control among males. Several factors can explain this difference, including biological variations between men and women, such as differences in body composition, fat storage patterns, glucose homeostasis, and treatment responses (41, 44, 45). Additionally, in societies where women are often responsible for the care of their entire family, these responsibilities may negatively impact their ability to achieve self-care goals, including glycemic control (38, 43).
Another important finding of this study was the significant association between higher education levels and better HbA1c control. Patients with primary, secondary, and academic education had 1.40, 1.94, and 2.30 times higher chances, respectively, of achieving HbA1c targets compared to illiterate patients. Similar findings were reported in studies from Saudi Arabia and Chicago, which also demonstrated the association between illiteracy and uncontrolled blood glucose (46, 47). Patients with higher education levels generally have more knowledge about their disease, and education, as an important social determinant, directly correlates with self-care behaviors in chronic diseases (47, 48). In summary, higher education enables individuals to make better decisions regarding self-care behaviors and improves their blood sugar control (49).
5.1. Strengths and Limitations
The strength of this study lies in its considerable sample size. In fact, this study utilized one of the largest samples of Iranian adults with T2DM to date, providing novel, population-specific insights into glycemic control and its influencing factors. However, a potential limitation is that patient data were collected from only one center (a referral center), which may affect the generalizability of the findings to all patients with diabetes in the broader population. This limitation should be considered when interpreting the results.
5.2. Conclusions
In this large sample of Iranian adults with type 2 diabetes, demographic factors such as older age and higher education were significantly associated with better glycemic control. However, the duration of diabetes diagnosis had a negative impact on HbA1c outcomes, with this effect being more pronounced in females than in males. These findings can guide future interventions, emphasizing the need for targeted strategies focusing on illiterate women who have had diabetes for several years.