1. Background
Gallstones are a prevalent condition affecting around 10% to 20% of adults and can cause significant economic and social burdens when complications arise (1). While most affected adults do not experience symptoms, the prevalence of gallstones is linked to age, gender, and ethnicity. Women are more prone to gallstones than men, with estrogen thought to play a role in their formation due to its effect on cholesterol (2-4). Gallstones and hypothyroidism are two common medical conditions that can occur due to various factors (5). Hypothyroidism is an endocrine disorder affecting 3.7% of people worldwide, and it is more common in women (4). This condition involves the formation of hard deposits of digestive fluid in the gallbladder, which can cause symptoms such as abdominal pain, nausea, vomiting, and fever. Gallstones can result from various factors, including genetics, obesity, and a high-fat diet (2, 3). Hypothyroidism can be overt (clinical) or subclinical, where the serum level of thyroxine is lower than normal. In cases where serum thyroid hormones are within the normal laboratory range but serum thyroid-stimulating hormone (TSH) levels are slightly elevated, subclinical hypothyroidism (mild thyroid insufficiency) is diagnosed (4). It is essential for individuals experiencing symptoms of gallstones to seek medical attention promptly to prevent complications and ensure proper management of the condition (6).
Studies suggest that approximately 13 - 24% of patients with gallstones have hypothyroidism (4). Recent clinical research indicates a correlation between thyroid activity and gallstone formation (2). The possible reason for this correlation is that movement disorders in the bile duct and sphincter of Oddi, combined with hyperlipidemia, may contribute to gallstone formation in patients with hypothyroidism (5). A study involving 3,749 participants aged 20 to 79 found an independent correlation between the presence of gallstones and elevated serum TSH levels in men, while a positive correlation was observed in women (6). However, another study concluded that there is no apparent correlation between the development of gallstones and hypothyroidism (7). In a study on 746 patients with hypothyroidism, 44.5% of women were found to have gallstones (8). Gallstones are believed to form due to a combination of factors, including cholesterol crystals in the bile. There is a well-established link between thyroid disease and lipid disorders, which can affect the composition and transport of lipoproteins. Hypothyroidism is linked to hypercholesterolemia and increased low-density lipoprotein (LDL) cholesterol levels, while hyperthyroidism leads to lower levels of total cholesterol, LDL, and high-density lipoprotein (HDL) cholesterol. Evidence suggests a possible association between hypothyroidism and cholesterol gallstone disease due to reduced LDL clearance and sphincter of Oddi dysfunction. The absence of thyroxine's pro-relaxing effect on the sphincter of Oddi may cause delayed biliary tract emptying, making individuals more prone to gallstone formation (9). On the other hand, recent studies have discovered a correlation between the ABO blood group system and various types of cancer, as well as several benign and malignant diseases, including some rheumatologic conditions, medullary thyroid cancers among thyroid diseases, and autoimmune diseases. Additionally, a new association between blood groups and autoimmune diseases has emerged. These findings suggest a potential link between the most commonly seen benign thyroid diseases, particularly Hashimoto’s thyroiditis, and blood groups. However, no study has yet shown a direct association between these diseases and blood groups (10).
2. Objectives
Therefore, this study aims to establish a correlation between hypothyroid function and the occurrence of gallstones in patients from different blood groups.
3. Methods
3.1. Study Design and Setting
This is a retrospective case-control study conducted in 2023 on patients with gallstones who were candidates for cholecystectomy in hospitals affiliated with Abadan University of Medical Sciences. Patients with a history of thyroid surgery, those using drugs and substances that cause hypothyroidism (such as amiodarone, lithium, antidepressants, phenytoin, and interferon), as well as drugs that cause gallstones (such as estrogen-like fenofibrate and gemfibrozil) were excluded (11). After applying the inclusion and exclusion criteria, a total of 450 patients were selected for the study, with 150 individuals in the case group (who had been hospitalized for gallstone surgery) and 300 individuals in the control group (who did not suffer from gallstones). Both groups were matched based on age, sex, and place of residence, and were evaluated for blood groups and hypothyroidism.
3.2. Data Collection Tools
Data collection was carried out using a researcher-designed checklist that included information on demographics, blood groups, thyroid test results, duration of infection, and underlying diseases. Interviews and blood tests were conducted to complete the checklist, which was validated through feedback from field experts. Subclinical hypothyroidism was identified in patients through TSH blood tests. The diagnostic criteria for hypothyroidism were set at TSH levels exceeding 5 μIU/mL, alongside normal levels of T4 (12). Venous blood samples were collected from patients to evaluate their TSH and free T4 (FT4) levels. The samples underwent centrifugation and serum separation before being stored at -20°C. A human TSH measurement kit from Pars Azmoun, an Iranian company, was used to determine TSH levels via the ELISA method. The kit, with a sensitivity of 0.05 μIU/mL, had a measurement range of 0.3 to 5 μIU/mL. Additionally, an ELISA kit procured from Pars was used to measure FT4 levels, with a sensitivity of 0.2 ng/dL and a measurement range of 0 - 10 ng/dL. A specialist confirmed the diagnosis of gallstones based on an ultrasound of the gallbladder and bile ducts. Blood groups were determined with a Cinagen blood group detection kit utilizing Cinagen antibodies, and the outcomes were reported accordingly.
3.3. Data Analysis
The normality of the data was assessed using the Kolmogorov-Smirnov test, which indicated a normal distribution. We used central tendency and dispersion measures such as frequency, percentage, and mean ± standard deviation to compare groups. Additionally, the chi-square test and Fisher's exact test were employed. A logistic regression model was applied to determine the impact of variables on the incidence of gallstones. The data were analyzed using the Statistical Package for the Social Sciences (SPSS) version 26, with a significance level set at P < 0.05.
4. Results
The study included a total of 450 patients, with an average age of 41.42 ± 15.74 years. Among them, 189 patients (42.0%) were male. Hypothyroidism was observed in 56 patients (12.44%), and the average duration of the disease was 5.26 ± 1.58 years. When the patients were analyzed in groups, no significant statistical differences were found in terms of age, gender, and duration of the disease (Table 1).
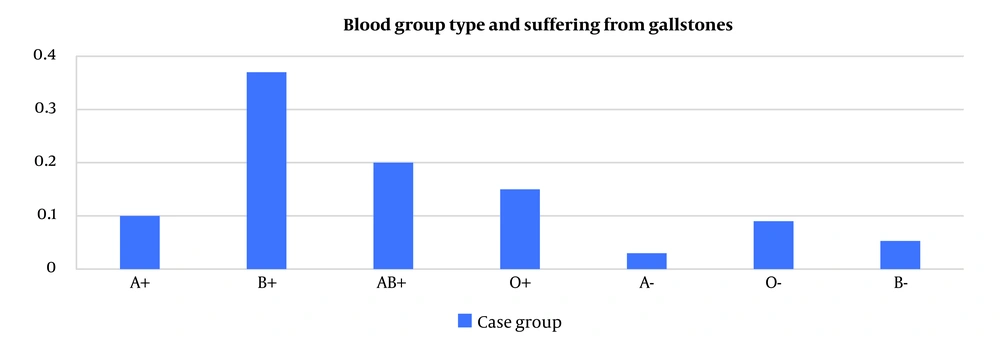
According to Table 1, the incidence of hypothyroidism was significantly higher in the case group (17.3%) compared to the control group (10.0%). Statistical analysis using Fisher's exact test revealed a significant relationship between gallstones and hypothyroidism (P = 0.03). Additionally, the study analyzed the distribution of blood groups among individuals with gallstones and found that the B+ blood group had the highest frequency (37.3%), while the A- blood group had the lowest frequency (8.7%). The chi-square test results demonstrated a significant association between blood type and gallstones (P < 0.001) (Figure 1).
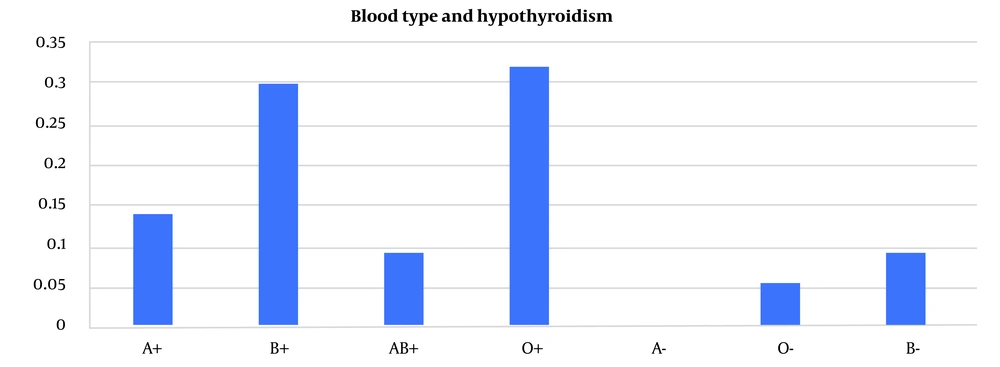
It was found that the most prevalent blood group among individuals with hypothyroidism was O+ (32.1%). A one-dimensional chi-square test revealed a significant correlation (P < 0.001) between blood group and hypothyroidism, as visually represented in Figure 2.
According to the findings in Table 2, there is a significant statistical correlation between gallstones and hypothyroidism, regardless of blood group, as evaluated through the chi-square test (P = 0.03). Specifically, the highest frequency of patients suffering from both hypothyroidism and gallstones was observed in blood group O+. These results suggest that there may be a relationship between blood group and the occurrence of gallstones in patients with hypothyroidism.
| Variable | Hypothyroidism | P-Value | |
|---|---|---|---|
| Intervention Group (N = 150) | Control Group (N = 300) | ||
| Blood groups | 0.03 b | ||
| A+ | 2 (8.0) | 6 (19.4) | |
| B+ | 7 (28.0) | 10 (32.3) | |
| AB+ | 0 (0.0) | 5 (16.1) | |
| O+ | 9 (36.0) | 9 (29.0) | |
| O- | 2 (8.0) | 1 (3.2) | |
| B- | 5 (20.0) | 0 (0.0) | |
Consensus Table of Blood Group and Gallstones in People with Hypothyroidism a
Based on the results of the logistic regression test, it was found that an individual's blood group and hypothyroidism status can predict the likelihood of developing gallstones with 12% accuracy. The study revealed that individuals with blood groups A+ and O+ have a significantly higher chance of developing the disease, nearly four times higher than those with other blood groups (13.20 - 1.25 CI: 0.95, OR = 4.06), (12.83 - 1.35 CI: 0.95, OR = 4.16). Additionally, the likelihood of developing gallstone disease nearly doubled for individuals with hypothyroidism, according to the results (3.53 - 1.05 CI: 0.95, OR = 1.93) (Table 3).
| Variables | Regression Coefficient | Standard Deviation of the Error | Parent Statistics | Degrees of Freedom | Significance Level | Odds Ratio | Odds Ratio CI 95% |
|---|---|---|---|---|---|---|---|
| Blood groups | - | - | 34.50 | 6 | 0.000 | - | - |
| A+ | 1.40 | 0.60 | 5.45 | 1 | 0.019 | 4.06 | 13.20 - 1.25 |
| B+ | 0.56 | 0.55 | 1.04 | 1 | 0.307 | 1.76 | 5.20 - 0.59 |
| AB+ | -0.20 | 0.59 | 0.12 | 1 | 0.728 | 0.81 | 2.60 - 0.25 |
| O+ | 1.42 | 0.57 | 6.15 | 1 | 0.013 | 4.16 | 12.83 - 1.35 |
| A- | -0.30 | 0.85 | 0.12 | 1 | 0.723 | 0.73 | 3.95 - 0.14 |
| O- | -0.08 | 0.66 | 0.01 | 1 | 0.898 | 0.91 | 3.37 - 0.25 |
| Hypothyroidism | 0.65 | 0.31 | 4.58 | 1 | 0.032 | 1.93 | 3.53 - 1.05 |
| Constant | -1.23 | 0.73 | 2.81 | 1 | 0.093 | 0.29 | - |
Investigating the Effect of Blood Groups and Hypothyroidism on Gallstones by Logistic Regression Model
5. Discussion
The objective of this study was to investigate the correlation between hypothyroidism and gallstones in patients' blood groups. Gallstone disease refers to the occurrence of symptoms or complications caused by gallstones, a costly gastrointestinal disorder that often leads to hospital admission (13). Gallstones are classified into two main types based on their anatomical location: Gallbladder stones (also known as cholecystolithiasis) and bile-duct stones. Bile-duct stones can be further categorized into extrahepatic duct stones (mostly common bile duct stones, or EHD stones) and intrahepatic duct stones (also called hepatolithiasis, or IHD stones). Treatment strategies, biomedical components, pathophysiology, and associated factors are thought to be distinct for different gallstone subtypes (14, 15). Gallstones may have different prevalences based on factors such as age, anatomical location, gender, and geographical location. There has been less focus on exploring the potential risk factors associated with different blood groups (16, 17). The ABO blood group system is medically significant for investigating various diseases. Genetic differences in blood groups have led to controversial issues regarding the relationship between the ABO blood group and susceptibility to certain infectious and non-infectious diseases. The presence or absence of antigens in certain blood groups can alter the morphology and function of the blood membrane. Functions associated with the structure of blood groups can actively, and sometimes subtly, contribute to the onset of various diseases (18, 19). Various blood groups may play different roles in various diseases, which require further research. These diseases include infectious diseases, rectal, colon, and stomach cancers, high blood pressure, endocrine diseases, pancreatitis, diabetes, and leukemia. Through analyzing the data collected in this study, we aim to better understand the influence of blood groups compared to previous research (18, 20-22).
The research results indicated that patients with the B+ blood group had the highest prevalence of gallstones. Furthermore, a significant statistical difference was observed between blood type and the occurrence of gallstones. However, previous studies in this field have presented inconsistent findings. For example, Alsisi et al. discovered that 46.1% of the 266 patients with gallstones had the O+ blood group, which was the highest frequency (23). Kratzer et al. reported that AB+ blood type had the highest frequency of 12.1%, but no significant association was identified between gallstones and blood type (24).
In this study, researchers investigated the connection between blood groups and hypothyroidism. They found that individuals with blood group O+ had the highest occurrence of hypothyroidism, which was statistically significant. This finding is consistent with previous studies by Alazmi et al. and Dagdeviren et al. The results of this research can help further understand hypothyroidism and inform future clinical practice (8, 10). Another study by Prakash et al. found that around 45.5% of infected individuals with blood group O+ had hypothyroidism (25). Previous studies have also shown a higher incidence of hypothyroidism in people with blood type O+. Based on the findings of this study, individuals with a history of hypothyroidism are more likely to have blood group O+ and less likely to have blood group AB+ compared to blood group O+. Blood group O+ does not have A and B antigens, while both antigens are present in blood group AB. The abnormal expression of blood group antigens on thyroid cells may lead to tissue damage, ultimately resulting in hypothyroidism in individuals with blood type O+ (17). The results of this study, as well as the Khoshgoeian et al. study, indicate a potential connection between blood group antigens and hypothyroidism, which necessitates further investigation for a comprehensive understanding (26). A study conducted in India also pointed to the role of blood group O+ in the occurrence of hypothyroidism. This study introduces blood groups A and B as a factor in the occurrence of hyperthyroidism (25).
A recent study has found a relationship between hypothyroidism and gallstones, regardless of blood type. The link between gallstone disease and hypothyroidism can be attributed to several factors. Hypothyroidism hinders cholesterol metabolism in the liver and reduces bile secretion. About 90% of hypothyroid patients have high levels of cholesterol and triglycerides in their blood. The elevated levels of serum cholesterol in hypothyroidism can lead to bile saturation with cholesterol. When bile becomes oversaturated with cholesterol, it can result in decreased gallbladder motility, contractility, and impaired filling, which may lead to prolonged retention of bile in the gallbladder. This extended retention provides enough time for sedimentation and growth of gallstones (27). Interestingly, patients with blood type O+ who had both conditions exhibited the highest frequency. This discovery aligns with a previous investigation by Dhoka et al., which found a positive correlation between gallstones and hypothyroidism in 33.7% of the 86 patients examined (28).
Thyroid hormones play a significant role in maintaining physiological homeostasis by influencing both lipid metabolism and the motor function of the biliary system. The modulation of lipid metabolism by thyroid hormones has significant implications for individuals with thyroid disorders, as it can impact cholesterol levels and increase the risk of cardiovascular disease. Moreover, the effects of thyroid hormones on the biliary system can contribute to the development of gallbladder disease, highlighting the importance of further research in this area (28). A study conducted by Issa involving 232 patients diagnosed with gallstones found that only 32 of them were also diagnosed with hypothyroidism. This suggests that there is no significant association between hypothyroidism and the occurrence of gallstones (7). However, it is possible that the observed correlation between hypothyroidism and study outcomes was not statistically significant due to the high levels of alkaline phosphatase discovered in the bile ducts of the 23 hypothyroid patients. This specific enzyme was found to be within normal levels in patients who were either hyperthyroid or euthyroid. It is plausible that secondary thyroid hormones do not affect the receptors responsible for bile movement, which may lead to biliary and sphincter stasis and Oddi dysfunction. These conditions, caused by thyroxine deficiency induced by hypothyroidism, may cause an increase in biliary pressure and elevated levels of alkaline phosphatase (28).
Many studies have explored the link between ABO blood groups and diseases, proposing potential mechanisms. However, conflicting results have made it difficult to reach a definitive conclusion. Despite this, evidence has been gathered to shed light on this association. ABO blood groups may impact the risk of various diseases through both known and unknown mechanisms. It is now understood that ABO blood groups are not the direct cause of diseases, but rather can predispose individuals to certain health problems.
5.1. Limitations
A limitation of this study is its small sample size, especially considering the significance and scope of the research. Additionally, the study was limited to hospitals in specific regions, which may affect the generalizability of the findings.
5.2. Conclusions
The study has demonstrated a significant relationship between hypothyroidism and gallstones in individuals with specific blood groups. Further research on blood group variables is highly recommended to validate the findings of this study and to uncover the underlying pathophysiological mechanisms that may explain the observed correlation.