1. Background
Among common cancers, breast cancer occurs in every individual, age group, and race. It is a major health problem. It impacts community health. It is the second leading cause of cancer deaths in women, after lung cancer (1). The World Health Organization reports this cancer makes up 30% of all women's cancers worldwide. Annually, about 500,000 women are diagnosed with it (2). Each year, over 1.6 million new cases of breast cancer are found in women worldwide. The age-specific incidence rate of breast cancer is 38.9 per 100,000 women globally. It is 86.4 in developed countries and 27.3 in less developed ones (3). In Iran, 23.3 women per 100,000 get breast cancer each year. It is expected to rise by 34% by 2025 (4).
The onset of this common disease can be stressful for affected women. Neglecting their mental health may hurt their survival. It can affect their treatment and follow-up care (5). Lotfi Kashani et al. showed that this disease causes psychological issues. It also speeds up cancer progression (6). Alongside concerns from this disease, we should consider a fear of its progression. It is a rational response to the threat of cancer and its treatments. It includes many real fears about the disease. It is a normal, proper response to a chronic, disabling, or fatal illness. However, this fear can lead to negative effects on the patient's mood and excessive anxiety (7). Dinkel et al. say that patients with serious illnesses often fear their illness, its treatment, and its social and psychological effects (8-10). Fear of disease progression is when patients worry their illness will get worse. This concern includes psychological, social, and biological effects. It's a normal reaction, not a sign of mental illness, and patients are fully aware of it. Patients may have real, lasting, or exaggerated fears. These can harm their well-being and quality of life (10). It causes many challenges, including caring for children and family, losing a job, feeling out of control, changes in sexual relationships, anxiety, emotional disorders, and a loss of confidence (11). Fifty six percent of cancer patients in the world and 49% of cancer patients in Iran suffer from this fear (12, 13). Koch Gallenkamp et al. found that 13 percent of a sample of colon, rectal, prostate, and breast cancer survivors had moderate to severe fear (14-16). Therefore, these cases show that this group of patients needs support after diagnosis, and during and after treatment (17, 18). Cancer and its treatment have many dimensions. So, we can't summarize a cancer patient's treatment using only clinical factors. We must also consider psychological treatments alongside clinical ones (19).
Psychological approaches seem key in treating cancers and their outcomes. They boost self-care, improving health and preventing disease. Among effective psychological approaches, cognitive-behavioral stress management stands out. Therapy is likely to be more effective and lasting if it addresses the emotions and thoughts that affect behavior. Cognitive-behavioral stress management is better than usual care. It reduces fear of disease progression (20). Cognitive-behavioral stress management is better than usual care at reducing the fear of disease progression. Its effect size is 0.2 to 0.37 (21). Cognitive-behavioral stress management is a multifaceted approach that teaches individuals various techniques, including relaxation training, diaphragmatic breathing, mindfulness, identifying automatic negative thoughts, replacing them with logical ones through cognitive restructuring, coping skills training, anger management, and assertiveness training (22). Cognitive-behavioral stress management helps patients accept their chronic conditions. It also helps them improve their physical health. Patients see their emotions, thoughts, and behaviors as bad. Negative thoughts can trap them in an unhealthy cycle. Cognitive-behavioral stress management breaks this cycle. It teaches individuals to change their negative thoughts and behaviors. It helps them adopt behaviors that can improve their mood. It helps the patient cope with their fear of disease progression. This prevents negative reactions to that fear. It does not focus on the past. It works on the patient's current life problems (23). Cognitive-behavioral stress management can lower stress hormones. It can also boost the immune system. This may slow disease progression. In this regard, Phillips et al. (24) showed that cognitive-behavioral stress management reduces cortisol levels. It also increases relaxation in women with breast cancer 4–8 weeks post-surgery. Additionally, the study by Khatibian et al. showed that group CBT significantly reduces stress in women with breast cancer (25).
2. Objectives
Considering the psychological damages in women with breast cancer and the effectiveness of cognitive-behavioral therapy in alleviating psychological damages in various individuals, and also considering that this method has no specific side effects and no study has yet investigated the effect of cognitive-behavioral stress management on fear of disease progression in women with breast cancer in Iran, the present study aimed to evaluate the effect of this treatment on fear of disease progression in women with breast cancer.
3. Methods
3.1. Research Design and Participants
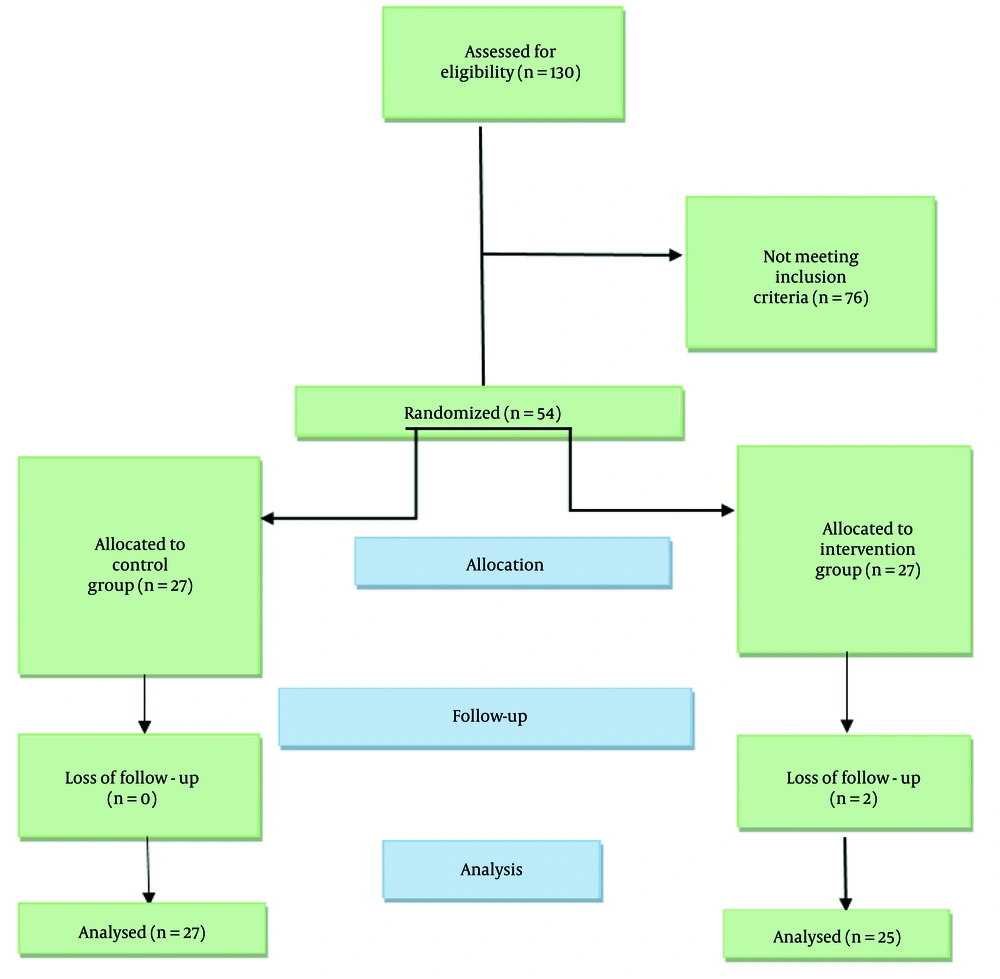
The present study is a randomized controlled trial aimed at determining the effectiveness of cognitive-behavioral stress management on fear of disease progression in women with breast cancer. Figure 1 shows the flowchart of the progress through the phases of the trial.
This study was approved by the Ethics Committee of Ahvaz Jundishapur University of Medical Sciences with the code number IR.AJUMS.REC.1400.611. After obtaining the clinical trial code IRCT20220122053798N1, sampling was initiated by the researcher.
3.2. Population and Research Sample
The study population included all women with breast cancer referred to the Oncology Department of Golestan Hospital in Ahvaz in 2021. The research sample consisted of 54 women from the study population who met the inclusion criteria, did not meet the exclusion criteria, and were willing to participate. After obtaining consent, we provided a demographics form and a Fear of Progression Questionnaire (FOP) to women who met the study criteria and agreed to participate.
Entry criteria included: A cancer diagnosis by an oncologist, a score above 85 on the FOP, literacy in Persian, willingness to participate in the study, and completion of treatment (surgery, chemotherapy, radiotherapy).
The study excluded participants with: Incomplete questionnaires, simultaneous medical disorders (incurable diseases including neurological, hematologic, infectious, and renal diseases, and diseases requiring special care), concurrent psychotherapy for malignant diseases, and any signs of metastatic disease.
3.3. Sample Size Estimation
A total of 21 subjects were calculated based on the formula, and considering a 25% dropout rate, 27 subjects were allocated to each group (26).
Equation 1.
Z1-α2 = 1.96: Considering a power of 95%; Z1-β = 1.28: Considering a power of 90%; S1 = 7.48; S2 = 12.12;
3.4. Randomization
After completing the questionnaires, they were scored and reviewed. Then, 54 women who scored above 85 on the FOP Questionnaire were selected. Participants were randomly assigned to intervention and control groups using block randomization with 4-member blocks. The allocation ratio was 1:1. To conceal the random allocation, 27 A's and 27 B's were placed in separate opaque envelopes. These envelopes were given to the center's secretary. To provide more assurance, we ensured that neither the researcher nor the participants knew their group assignments.
3.5. Intervention
After selecting the samples and placing the participants into two 27-member groups (accounting for a 25% dropout rate), cognitive-behavioral counseling sessions were conducted in seven groups — six groups of four members and one group of three members — for the intervention group. Each session consisted of 10 face-to-face meetings, lasting 90 minutes, with 45 minutes dedicated to training and 45 minutes to practical work. The researcher coordinated with the intervention group to schedule the counseling sessions. Each session's training was structured, presenting the educational content first, followed by practical work and a review of new topics. For participants who missed a session, the content was repeated in the next session. However, if they missed more than two sessions, they were excluded from the study. Another test, similar to the first, was conducted immediately after and one month following the 10 group counseling sessions.
The control group received only routine care throughout the study, with no counseling or intervention. As a thank you for their participation and to uphold ethics, a one-day workshop was held for the control group at the end of the intervention. The sessions took place in a classroom in the Oncology Department of Golestan Hospital in Ahvaz. The educational program followed the Antoni, Ironson, Schneider training package (27), consisting of 10 sessions of 90 minutes each, held once a week at a specified time, as follows:
- Session 1: Introduction. Explain stressors and how to respond to them. Discuss awareness of stress's physical effects and potential health risks. Introduce muscle relaxation.
- Session 2: Review of session 1. Stress, and awareness of its effects on emotions, thoughts, and behaviors. Practice muscle relaxation.
- Session 3: Review of session 2. Explain the link between thoughts and emotions, introduce diaphragmatic breathing, visualization, and muscle relaxation.
- Session 4: Review of session 3. Identify negative thoughts and cognitive distortions, and discuss ways to challenge them. Include breathing, visualization, and muscle relaxation techniques.
- Session 5: Review of session 4. Replace irrational thoughts with logical ones. Teach self-suggestion for feeling heaviness and warmth.
- Session 6: Review of session 5. Teach effective coping and self-suggestion for heart rate, breathing, stomach, and forehead.
- Session 7: Review of session 6. Implement effective coping responses, and teach self-suggestion with visualization and self-hypnosis.
- Session 8: Review of session 7. Teach anger management.
- Session 9: Review of session 8. Teach assertiveness in interpersonal relationships and counting breathing meditation.
- Session 10: Review of session 9. Explain social support and teach techniques for growing social networks. Review the entire program and create a personal stress management plan after the test.
In the intervention group, 2 members dropped out due to unwillingness to participate in the remaining training sessions.
3.6. Blinding
Blinding was not possible in this study due to its nature. Therefore, to reduce the likelihood of bias, the allocation of participants to intervention groups was carried out by an individual who did not participate in the sampling and data analysis.
3.7. Outcome Measurement
Participants completed the Fear of Disease Progression Questionnaire before, immediately after, and one month after the 10 sessions of group counseling. The control group received no additional education or counseling, except for routine care, throughout the study. At the end of the intervention, a one-day workshop was held for the control group.
3.8. Data Collection Tools
The data collection tools included a self-made demographic questionnaire, which gathered data on age, menarche age, and marital status. It also inquired about illness duration, breastfeeding history, occupation, education, economic status, and treatment type.
3.8.1. Fear of Progression Questionnaire
This questionnaire consists of 43 items and has 5 subscales. Responses are recorded on a 5-point Likert scale, ranging from "never" to "most of the time". To obtain the total score, all subscale scores are summed, excluding the anxiety coping subscale. Scores above 85 indicate fear, which is above the average.
3.9. Reliability and Validity
The FOP is a self-report tool developed by Herschbach on a sample of cancer, rheumatism, and diabetes patients in Germany. The final version comprises 43 items and 5 subscales: Emotional response, family, occupation, loss of independence, and anxiety coping. It measures responses on a Likert scale from "never" to "most of the time." The total score is the sum of all subscale scores, excluding the anxiety coping subscale (28). Herschbach et al. reported an internal consistency of 0.95 and a test-retest reliability of 0.94 for the questionnaire (8).
In Iran, the Cronbach's alpha method found the test's reliability to be 0.86 for emotional response, 0.72 for family, 0.76 for occupation, and 0.71 for loss of independence, with an overall alpha of 0.91 (29). Three faculty members of the Psychology and Educational Sciences Department at the Islamic Azad University of Tabriz reviewed the questionnaire and confirmed its face and content validity (30).
3.10. Statistical Analysis
Descriptive statistics, including frequency distribution, graphs, and measures of central tendency and dispersion, were used to describe the study variables. The Kolmogorov-Smirnov test was employed to test the normality of quantitative variables. Subsequently, the relationship between qualitative and quantitative variables with the treatment group was examined using the chi-square test, independent t-test, or non-parametric Mann-Whitney test. Due to repeated evaluations, the Repeated Measures test was also utilized. Data analysis was performed using SPSS software version 22, with a significance level set at 0.05.
4. Results
The total initial sample included 130 individuals with fear of disease progression. Of these, 54 participants (27 in the intervention group and 27 in the control group) met the study's inclusion criteria. Two individuals in the intervention group withdrew from the study due to unwillingness to continue. Ultimately, 25 participants in the intervention group and 27 in the control group were studied.
The two study groups did not differ significantly in demographics, including age, age of onset, duration of illness, education, marital status, economic status, employment, breastfeeding history, and treatment method (P > 0.05). Before the study, the two groups had similar mean scores for fear of disease progression (P > 0.05). However, immediately after the ten intervention sessions and four weeks later, the two study groups showed significant differences in mean scores of fear of disease progression, including its dimensions such as family, emotional response, independence, and employment (P < 0.001).
Only the intervention group showed significant intragroup changes in mean scores for fear of disease progression and all its dimensions (P < 0.001), while there were no significant intragroup changes in the control group (P > 0.05).
5. Discussion
Based on the findings (Table 1), the average age of women in the intervention group was 71.1 ± 66.42 years, while in the control group, it was 71.2 ± 66.44 years, indicating homogeneity in terms of age between the groups. The younger onset of this disease raises concerns about fertility, breastfeeding, and disease recurrence after pregnancy, which are more pronounced than concerns at non-fertile ages. Koch-Gallenkamp et al. reported that younger individuals and women reported greater fear (16).
| Variables | Intervention Group (N = 25) | Control Group (N = 27) | P-Value |
|---|---|---|---|
| Age (y) | 42.66 ± 1.71 | 44. 11 ± 2. 11 | 0.367 |
| Menarche age | 12.03 ± 0.37 | 12.66 ± 0.36 | 0.941 |
| Duration of illness (mo) | 8.77 ± 0.71 | 9.18 ± 4.15 | 0.706 |
| Educational attainment | 0.953 | ||
| Less than a diploma | 20 (74.1) | 21 (77.80) | |
| Diploma | 5 (18.5) | 4 (14.8) | |
| University degree | 2 (7.4) | 2 (7.4) | |
| Marital status | 0.294 | ||
| Single | 3 (11.1) | 6 (22.2) | |
| Married | 20 (74.1) | 15 (55.6) | |
| Other | 4 (14.8) | 6 (22.2) | |
| Economic situation | 0.699 | ||
| Poor | 5 (18.5) | 4 (14.8) | |
| Moderate | 15 (55.6) | 18 (66.7) | |
| Good | 7 (25.9) | 5 (18.5) | |
| Job | 0.551 | ||
| Housewife | 9 (33.3) | 7 (25.9) | |
| Employed | 18 (66.7) | 20 (74.1) | |
| Breastfeeding history | 0.340 | ||
| Yes | 22 (81.5) | 19 (70.4) | |
| No | 5 (18.5) | 8 (29.6) | |
| Treatment method | 0.45 | ||
| Single drug | 14 (51.8) | 12 (44.4) | |
| Multi drug | 13 (48.1) | 15 (55.6) |
Comparison of Demographic Factors of Subjects in Intervention and Control Groups a
The average age at menarche in the intervention group was 37.03 ± 12 years, and in the control group, it was 36.66 ± 12 years. The average duration of disease in the intervention group was 71.77 ± 8 years, and in the control group, it was 15.418 ± 0.09 years (31). Savard and Ivers found that fear of disease progression tends to be stable or slightly reduced in the first few months after diagnosis or during rehabilitation due to adaptation and alignment with the disease.
More than half of the participants had a history of breastfeeding and were married. The most important concerns for women with cancer are twofold: Fear for their family and future children, and fear that the disease would disrupt their marriage. In Sarkar et al.' study, results showed that married patients reported more fear of cancer recurrence (32). In Mehnert et al.'s study, having a child was linked to a fear of cancer recurrence (33).
More than half of the participants were employed, and the fear of losing their job and future financial situation is higher in employed individuals. In Wagner et al.'s study, the fear of disease progression was higher in employed women (34). Additionally, over half had moderate economic status, fearing they might not afford their expenses and treatment costs. Over half had sub-diploma education, leading to fear due to less knowledge of the disease and its treatment. They needed training and information on awareness, symptoms, signs of recurrence, and risk-reduction strategies. The study by Aghdam et al. showed that patients with lower income and education levels reported a higher fear of disease progression (12).
Over half of the patients received combination therapy, fearing the drugs would harm their bodies and worrying about meeting doctors and tests. In Yang et al.'s study on breast cancer patients, those who received chemotherapy and radiotherapy reported higher fear of disease progression. The demographic and population characteristics of the two groups, intervention and control, showed no significant difference in any characteristics, including age, menarche age, marital status, disease duration, breastfeeding history, occupation, education, economic status, and treatment type (35).
Therefore, in this study, demographic and population characteristics cannot be considered as intervention variables. We could not find any study specifically assessing the effect of cognitive-behavioral stress management on fear of disease progression in women with breast cancer. The results of the present study indicate that stress management through cognitive-behavioral methods reduces the fear of disease progression in women with breast cancer (36). Javnbakht and Haghjo studied the effects of existential therapy on fear of disease progression and pain in breast cancer patients, finding significant reductions in both in the experimental group compared to the control group (37), which is consistent with the findings of the present study.
Cognitive-behavioral stress management also reduces women's self-perception of their family role in breast cancer patients. The study by Aghdam et al. and Hanprasertpong et al. on factors related to fear of disease progression in cancer patients found that participants' greatest fear was about their families, and their children's future and marriage (12, 38). The present study found that cognitive-behavioral stress management reduces emotional reactions in women with breast cancer. The study by Emami et al. showed that cognitive-behavioral therapy can increase resilience and hope in women with breast cancer, consistent with the present study. Cognitive-behavioral techniques help individuals learn to reduce negative emotions, find motivation, and use unpleasant events to pursue future goals. They also become aware of life's negative emotional effects (39).
The results of the present study indicate that stress management through cognitive-behavioral methods effectively reduces the score of the job stress domain in women with breast cancer. Financial security and not needing others are prerequisites for social health, and individuals need adaptation and alignment with changing conditions, which is achieved by using cognitive-behavioral stress management approaches (Table 2). The results also indicate that stress management through cognitive-behavioral methods effectively reduces the score of the independence domain in women with breast cancer.
| Variables | Intervention Group (N = 27) | Control Group (N = 27) | P-Value | P-Value |
|---|---|---|---|---|
| Total score of fear of disease progression | < 0.001 | |||
| Before intervention | 135.51 ± 8.18 | 130.03 ± 10.73 | 0.06 | |
| Immediately after intervention | 75.48 ± 7.91 | 135.66 ± 9.30 | < 0.001 | |
| Four weeks after intervention | 74.55 ± 8.17 | 135.92 ± 8.60 | < 0.001 | |
| P-value | < 0.001 | < 0.076 | - | |
| Effect size | < 0.606 | |||
| Family | < 0.001 | |||
| Before intervention | 27.96 ± 2.66 | 30.00 ± 3.16 | 0.013 | |
| Immediately after intervention | 13.00 ± 2.41 | 31.03 ± 2.94 | < 0.001 | |
| Four weeks after intervention | 12.44 ± 2.37 | 30.62 ± 2.97 | < 0.001 | |
| P-value | < 0.001 | 0.27 | - | |
| Effect size | < 735 | |||
| Emotional reaction | < 0.001 | |||
| Before intervention | 49.66 ± 7.14 | 46.40 ± 7.21 | 0.101 | |
| Immediately after intervention | 30.29 ± 5.51 | 48.96 ± 7.21 | < 0.001 | |
| Four weeks after intervention | 29.81 ± 5.51 | 48.18 ± 7.27 | < 0.001 | |
| P-value | < 0.001 | 0.221 | - | |
| Effect size | 0.821 | |||
| Employment | < 0.001 | |||
| Before intervention | 31.44 ± 3.38 | 29.29 ± 4.14 | 0.42 | |
| Immediately after intervention | 15.07 ± .43 | 30.03 ± 2.62 | < 0.001 | |
| Four weeks after intervention | 14.55 ± 2.56 | 29.33 ± 2.38 | < 0.001 | |
| P-value | < 0.001 | 0.52 | - | |
| Effect size | 0.632 | |||
| Independence | < 0.001 | |||
| Before intervention | 26.44 ± 3.82 | 24.33 ± 4.06 | 0.055 | |
| Immediately after intervention | 17.11 ± 3.25 | 25.62 ± 3.59 | < 0.001 | |
| Four weeks after intervention | 16...48 ± 3.05 | 24.77 ± 3.83 | < 0.001 | |
| P-value | < 0.001 | 0. 25 | - | |
| Effect size | 0.725 | |||
The Scores of Fear of Disease Progression and Its Dimensions in the Two Groups of Intervention and Control Before Intervention, and Immediately After Intervention and 4 Weeks Thereafter a
The study indicates the effectiveness of cognitive-behavioral stress management in reducing the fear of disease progression in women with breast cancer. This treatment helps patients accept these chronic conditions and work on improving their physical health. Patients often view their emotions, thoughts, and behaviors negatively, and negative thoughts can keep them in an unhealthy cycle. Cognitive-behavioral intervention breaks this cycle by teaching individuals how to change negative thinking patterns and behaviors, turning them into behaviors that can improve mental emotions. Cognitive-behavioral therapy focuses on current life problems rather than past issues, helping patients deal with the disease by accepting it to prevent negative reactions to disease progression and the fear it causes (27).
Correcting cognitive assessments, improving coping skills, and integrating learned techniques with stressful situations in life could lead to a reduction in the fear of disease progression. Cognitive-behavioral therapy helps by teaching techniques such as active activity review, structuring daily activities, and increasing the amount of enjoyable and successful activities. Since patients' behavioral responses to the fear of breast cancer progression result from ineffective or incorrect beliefs about the disease and its treatment, these beliefs are identified and evaluated by teaching self-assessment, identifying common cognitive errors about the fear of disease progression, and teaching responses to self-assessment and modifying their changes, thus decreasing the fear of breast cancer progression.
This treatment can play a useful role in improving the relationship between the doctor and the patient (40). Cancer has psychological and cognitive dimensions. Providing such services to breast cancer patients and other cancer patients not only effectively improves their psychological and psychiatric symptoms but also leads to the creation of supportive, coping, and empowering programs and actions, increasing the quality of medical treatments, and enhancing adherence to treatment guidelines by the patient and their cooperation and collaboration with their family. As a result, it helps surpass the disease.
5.1. Limitations and Strengths
The limitation of this study was related to the timing of its conduct, which coincided with the COVID-19 pandemic, necessitating more time to implement interventions properly. To address this issue, we minimized the risk of virus transmission by using spacious classrooms for educational sessions, maintaining appropriate distancing, providing masks to participants, and ensuring proper ventilation. Data collection was conducted during the COVID-19 pandemic, which may have caused fear and anxiety, potentially affecting the psychological status of the patients. The current research was the first randomized clinical trial to investigate the effectiveness of cognitive-behavioral stress management on fear of disease progression in women with breast cancer in Iran.
5.2. Suggestions
Based on the experience gained in this study, it is suggested that in similar circumstances, appropriate treatment packages for virtual interventions be developed under the title "Investigating the Effectiveness of Virtual Cognitive-Behavioral Stress Management on Fear of Disease Progression in Women with Breast Cancer". Conducting the majority of interventions virtually can offer patients several advantages, including ease of learning, elimination of the need for physical displacement, and prevention of secondary diseases.
5.3. Conclusions
Considering the findings of this research, it can be stated that the application of cognitive-behavioral stress management in cancer treatment centers can be effectively considered as a complementary therapy alongside medical treatments. This approach can help address the psychological and emotional challenges faced by patients, thereby enhancing their overall well-being and potentially improving treatment outcomes.