1. Background
Considering its incidence and prevalence in different societies, drug abuse has been a significant concern for governments, specialists, and families (1). Moreover, due to its physical and mental health implications, drug abuse is recognized as one of the twenty key factors impacting global mental health (2). According to collected data, for the first time in U.S. history, over 100,000 individuals lost their lives to narcotics overdose within a 12-month period (3). Globally, a 2015 report on narcotics revealed that approximately 450,000 people died due to drug-related causes, with 167,750 deaths directly attributed to drug abuse.
In Canada, evidence indicates a dramatic rise in overdoses involving fentanyl and methamphetamine in 2016 (4). The illegal use of amphetamines has been steadily increasing, with about 28.9 million people reportedly abusing these substances in 2017 (5). Similarly, in Iran, data from the research and training office of the anti-narcotics headquarters indicates that over the past decades, there have been approximately 4.4 million constant and non-constant drug abusers (6).
Effective addiction treatment strategies integrate both biological and psychological components. One of the most practical approaches currently used by therapists for withdrawal from narcotics and stimulants is Brief Intervention (BI) or the short cognitive-behavioral approach. A meta-analysis revealed that short cognitive-behavioral interventions are particularly effective in reducing drug abuse, enhancing patient motivation to quit, and significantly lowering relapse rates. Alongside maintenance treatments, psychological therapies play a crucial role in treating drug abuse (7).
Treatment with methadone is a widely used and effective approach for managing opioid addiction. However, it is crucial to incorporate interventions that address psychological and peripheral factors, as well as the social relationships of individuals with addiction. Among these interventions, group therapy is often the treatment of choice for certain cognitive disorders. Group therapy offers several advantages, such as saving time, teaching social skills to addicts, and improving their interpersonal relationships (8).
One of the most effective cognitive-behavioral approaches to combat drug abuse is relapse prevention training. The primary goal of this approach is to help clients develop self-control over behaviors related to drug use. Relapse prevention involves identifying high-risk situations, teaching clients decision-making strategies to handle these situations, encouraging changes to risky lifestyles, and helping clients learn from their mistakes (9).
In a study by Amiri et al., it was found that teaching life skills to individuals with narcotics addiction significantly contributed to relapse prevention and overall life improvement (10). These findings highlight the importance of comprehensive interventions that integrate both cognitive-behavioral strategies and skill-building to enhance the effectiveness of addiction treatment.
Sofuoglu et al., in a study on the effectiveness of cognitive intervention on relapse and general health of drug-dependent clients, found that cognitive intervention effectively prevented relapse and improved the general health of drug-dependent individuals (11). Similarly, Karami et al. reported that a cognitive rehabilitation program could be an appropriate approach for improving the response of male addicts in quitting heroin use, ultimately leading to heroin withdrawal without relapse (12).
Jafari et al., in an investigation of the effectiveness of BI on depression in addicts treated at Ahvaz centers for comprehensive health services, demonstrated that following the intervention, the experimental group had significantly lower mean depression scores than the control group (P < 0.001) (8). Sterling et al. found that BI reduced the likelihood of relapse into narcotics, marijuana, alcohol, and cigarette use among young adolescents and also decreased the chance of hospitalization (P < 0.05) (13).
In a systematic review and meta-analysis, Ray examined the effects of brief cognitive-behavioral treatment combined with therapeutic regimens for adolescents with alcohol and substance abuse. The findings indicated that using both brief cognitive-behavioral treatment and therapeutics was more effective than therapeutics alone (14).
These findings underscore the critical role of non-therapeutic interventions in the field of addiction treatment. They also highlight the essential need for psychotherapy programs in substance abuse treatment centers to enhance treatment outcomes.
2. Objectives
The present study aimed to compare the effect of BI on relapse prevention and withdrawal permanency in narcotics and stimulant abusers who referred to drop-in centers for addiction harm reduction in the city of Ahvaz, Iran.
3. Methods
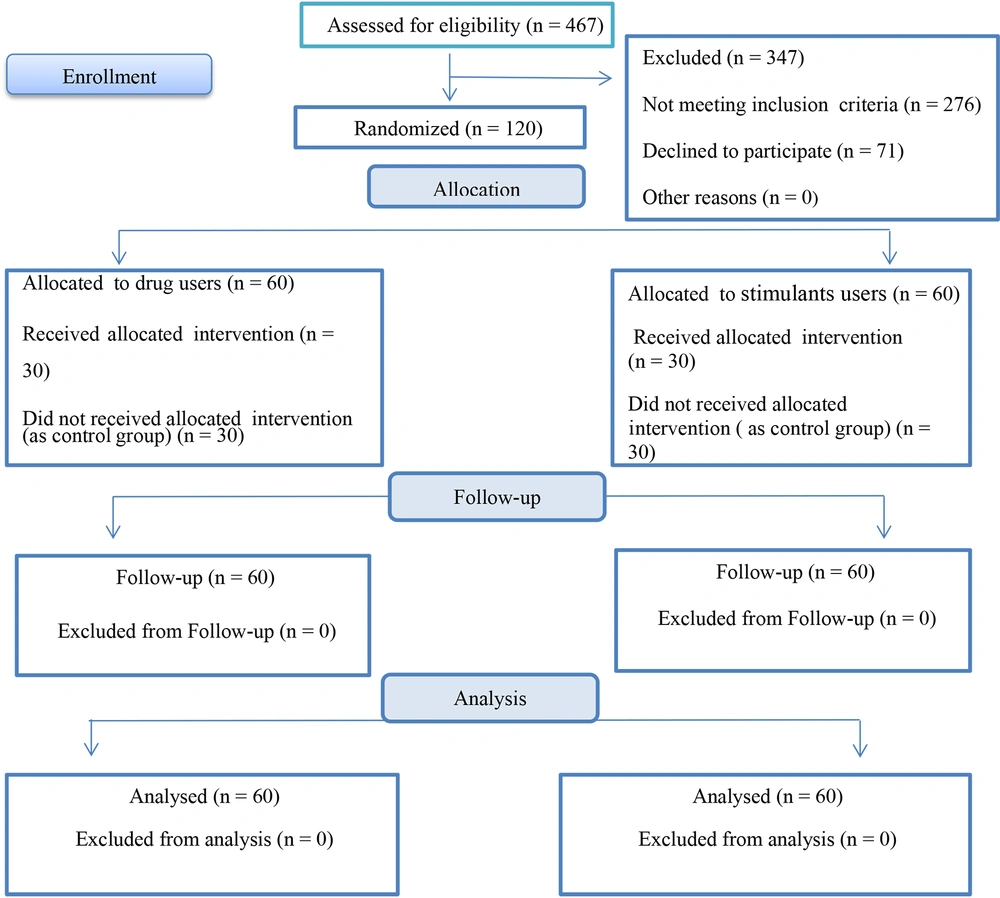
Our study was quasi-experimental and included two experimental groups and two control groups: One experimental group and one control group for narcotics abusers, and the same for stimulant abusers. The study was conducted in three stages: (1) Pre-test, (2) post-test, and (3) follow-up. The statistical universe of this inquiry comprised all addicts covered by Ahvaz centers for reducing addiction harm in 2023. At the time of the study, the total number of individuals covered included 98% male and 2% female addicts or stimulant abusers with current files in harm reduction centers.
Based on Cohen's table (1988), 120 individuals meeting the substance dependence criteria according to the DSM-5, as diagnosed by the centers’ psychiatrists, were randomly assigned to two experimental and two control groups, each consisting of 30 participants.
3.1. Research Tools
3.1.1. Morphine and Amphetamines Diagnostic Tests
To monitor opioids (morphine) and stimulants (amphetamine and methamphetamine) in the urine of addicts and drug abusers, fast test kits produced by Vira Novin Teb Zagros in Tehran were used. Screening tests were conducted by nurses at addiction harm reduction centers in Ahvaz, following laboratory diagnostic standards set by the Ministry of Health and Medical Education of Iran. Test results were recorded and provided to the researchers for analysis.
3.2. Methodology
After obtaining permission from the Deputy of Health at Jundishapur University of Medical Sciences in Ahvaz, the researchers visited addiction harm reduction centers in the city. The sample size, estimated to be 120 individuals based on Cohen's table (1988), was randomly divided into four groups: Two test groups and two control groups, with 30 participants each.
The study consisted of three stages. In stage I, pre-intervention, all participants in the test and control groups were evaluated and interviewed. Study aims were explained, and consent forms were collected. Baseline urine tests for morphine and amphetamines were conducted. In stage II, the test groups received BI sessions conducted by the researchers, following protocols from the Ministry of Health and Medical Education of Iran (2017). Two specific BI protocols were applied: (1) one tailored for narcotics addicts, and (2) the other for stimulant users. Each test group attended four 60-minute sessions, and participants signed official consent papers for participation. Control groups did not receive any intervention during this stage. In stage III, post-intervention, urine tests for morphine and amphetamines were repeated for all groups. To evaluate the permanency of drug abstinence, follow-up urine tests were conducted one month after the end of the intervention (Figure 1).
3.3. Brief Intervention Sessions
Brief intervention in substance use is a valuable tool for treatment and motivation to change behavior in cases of risky substance use. Brief intervention is a short-term cognitive behavioral intervention designed by Baker et al. (2003). This approach is based on the principles of motivational interviewing, where the responsibility for changing behavior is placed on the patient. Key components of this intervention include feedback, responsibility, advice, a menu of alternative change options, empathy, and self-efficacy. Brief intervention Protocol 1 specific to substance abusers (ministry of health and medical education, 2017): (Ministry of Health and Medical Education, 2017)
- Session 1: Behavioral change model #1
- Topic: The addict does not consider change (precontemplation) or begins thinking about reducing substance use or quitting (contemplation).
- Session 2: Behavioral change model #2
- Topic: Taking action to change behavior (intervention) and persisting in strict behavior modifications (maintenance).
- Session 3: Brief Intervention components
- Topic: Following the FRAMES model, focusing on feedback, responsibility, advice, a menu of change options, and self-efficacy.
- Session 4: ASSIST screening
- Topic: Providing feedback based on ASSIST (Alcohol, Smoking, and Substance Involvement Screening Test) points, categorized into three risk levels: (1) Low risk, (2) moderate risk, (3) high risk.
3.4. Data Analysis
To analyze the collected data, descriptive statistical methods such as standard deviation, frequency, and mean were employed. For testing the assumptions of normality of frequency distribution, equality of variances, and other covariance-related presumptions, the Shapiro-Wilks, Levene’s, and Kolmogorov-Smirnov tests were used. For comparing group means, analysis of variance (ANOVA) with repeated measures was applied.
3.5. Moral Considerations
This study was approved by the Ethics Committee of Shahid Chamran University, with the ethical code number IR.SCU.REC.1402.083. In this section, descriptive statistics on relapse prevention in addicts covered by the centers for reducing addiction harm are presented.
4. Results
The results presented in Table 1 indicate that the mean relapse prevention scores in the post-test stage and follow-up after BI differ significantly between the experimental and control groups of narcotics users. The means demonstrate that relapse rates in the addicts group who received BI were reduced compared to the control group in both the post-test stage and follow-up.
| Variable and Groups | Pre-test | Post-test | Follow-up |
|---|---|---|---|
| Addiction diagnostic test | |||
| BI in narcotics users | 37.90 ± 18.66 | 26.11 ± 6.31 | 26.89 ± 4.7 |
| Control | 43.07 ± 18.61 | 43.01 ± 18.18 | 42.71 ± 18.09 |
Abbreviation: BI, Brief Intervention.
a Values are presented as mean ± SD.
Table 2 shows that the mean relapse prevention scores in stimulant users who underwent BI did not differ significantly compared to the control groups. Before conducting repeated measures ANOVA, the assumptions for the test were reviewed and confirmed.
| Variable and Groups | Pre-test | Post-test | Follow-up |
|---|---|---|---|
| Addiction diagnostic test | |||
| Intervention in stimulant users | 39.01 ± 3.18 | 38.02 ± 3.55 | 37.83 ± 3.71 |
| Control | 42.26 ± 3.22 | 40.41 ± 3.15 | 40.12 ± 3.98 |
Table 3 shows that BI was effective in ensuring withdrawal permanency and relapse prevention among narcotics addicts at both the post-intervention and follow-up stages. The intervention accounted for 45% of the variance in relapse prevention scores after the intervention (P < 0.001).
| Trace and Coefficient | Value | Hypothesis (df) | Error (df) | F | P | Eta | Test Power |
|---|---|---|---|---|---|---|---|
| Group | |||||||
| Pillai′s trace | 0.987 | 12 | 172 | 3.221 | 0.001 | 0.45 | 0.73 |
| Wilks lambda | 0.469 | 12 | 131 | 4.520 | 0.001 | 0.45 | 0.73 |
| Hotelling′s trace | 1.07 | 12 | 150 | 4.118 | 0.001 | 0.45 | 0.73 |
| Roy′s largest root | 1.01 | 12 | 78 | 11.833 | 0.001 | 0.45 | 0.73 |
Table 4 shows that BI was not effective in ensuring withdrawal permanency and relapse prevention among stimulant users at both the post-intervention and follow-up stages (P < 0.331).
| Trace and Coefficient | Value | Hypothesis dF | Error dF | F | P | Eta | Test Power |
|---|---|---|---|---|---|---|---|
| Group | |||||||
| Pillai′s trace | 0.754 | 12 | 185 | 4.255 | 0.331 | 0.12 | 0.35 |
| Wilks lambda | 0.549 | 12 | 127 | 4.762 | 0.331 | 0.12 | 0.35 |
| Hotelling′s trace | 1.09 | 12 | 162 | 4.012 | 0.331 | 0.12 | 0.35 |
| Roy′s largest root | 1.12 | 12 | 65 | 10.921 | 0.331 | 0.12 | 0.35 |
5. Discussion
The aim of the present study was to compare the effects of BI on withdrawal permanency and relapse prevention in narcotics addicts and stimulant abusers who referred to Ahvaz addiction harm reduction DIC. The results showed that BI was effective at post-test and follow-up stages in narcotics abusers. However, it was not as effective in achieving withdrawal permanency and relapse prevention at post-test and follow-up stages in amphetamine abusers. These findings align with the studies of Amiri et al., Sterling et al., and Aldridge (10, 13, 15), but are not consistent with the results of D’Amico et al. (16).
5.1. Limitations of the Study
The following limitations should be considered when interpreting and generalizing the results of this study: (1) the study was limited to individuals who referred to drop-in addiction harm reduction centers in Ahvaz, Iran; (2) due to an insufficient number of female participants, all subjects in this study were male; (3) the study focused solely on narcotics addicts and stimulant abusers, without evaluating the effects of BI on individuals who use both stimulants and narcotics. We recommend that future studies explore the causal relationships between variables to better identify the factors influencing relapse prevention and withdrawal permanency. Additionally, future research should include mixed stimulant-narcotics users to provide a broader understanding of the effectiveness of BI in diverse populations.
5.2. Conclusions
Our findings highlight the necessity for therapists to place strict emphasis on teaching essential skills to addicts, enabling them to handle high-risk situations effectively, in conjunction with pharmacotherapy. Consulting services and relapse prevention are, in fact, inseparable components of successful addiction treatment.
The study by Mousali et al. demonstrated that narcotics addicts and stimulant users frequently experience relapse, with varying relapse patterns observed. This underscores the critical role of relapse prevention in addiction treatment. Understanding the chronological pathways of substance relapse provides therapists with valuable opportunities to tailor and adapt relapse prevention interventions effectively (6).
Regarding the comparison between cognitive behavioral therapy (CBT) and BI in drug users, it can be said that BI operates on the assumption that the responsibility and ability to change lie within the client. The therapist’s role is to establish conditions that enhance the client’s motivation and commitment to change. Most primary processes of change occur internally, as the individual realizes that success in quitting addictive behaviors depends on their own efforts (17).
On the other hand, CBT, with its structured and goal-oriented approach, focuses on the control and regulation of emotions, feelings, and psychological pressures (18). It helps individuals gain mastery over behavioral symptoms, understand the causes of their behavior, cope with negative thoughts, and develop problem-solving skills.
In summary, while CBT emphasizes cognitive processes and learning as key components in changing addictive behaviors, BI focuses on fostering the individual's intrinsic motivation to drive the change process. Both approaches offer unique strengths in addressing addictive behaviors and can be selected or combined based on the needs of the individual.