1. Background
According to the World Health Organization, suicide is one of the leading causes of death, with an estimated 800 000 people dying by suicide each year (1). The number of suicide attempts is significantly higher (2), and 90% of individuals who die by suicide have a history of mental illness, primarily depression (1, 3). Many people do not seek help due to the stigma associated with suicide or mental illness (1, 4).
In the past, rituals such as mutilating the corpses of those who died by suicide (to prevent the release of evil spirits), expelling their families from society, and confiscating the family’s property contributed to the stigma surrounding suicide (5, 6). While such practices no longer exist in Western countries, remnants of this stigma persist, such as some insurance policies that do not cover death by suicide (7).
Stigma is often subtle, manifesting in overt or omitted actions, informal social disapproval, isolation, and avoidance. It acts as a powerful force for rejection, negatively affecting the lives of individuals with severe mental disorders and their families (8, 9). People frequently avoid seeking the support and care they need out of fear of being negatively labeled by relatives or friends (10, 11).
The internalization of feelings of worthlessness and marginalization directly increases distress and confusion (12). This internal stigma lowers self-esteem, reinforces negative self-perceptions (13), and triggers shame and withdrawal, which further hinders access to care and worsens quality of life. One of the primary barriers to identifying and treating suicidal thoughts and behaviors is the negative attitude toward mental disorders and their treatment (14). People who have attempted suicide often face stigma as well (15), with many reporting feelings of shame (16).
There was no instrument for measuring suicide stigma until Scocco et al. (17) developed a 13-item scale in 2012 to measure stigma related to suicide attempts, which can be used by the general population, psychiatric patients, and individuals who have attempted suicide. Scocco et al. (17) demonstrated that the Stigma of Suicide Attempt (STOSA) Scale has good psychometric properties. The scale measures two factors: Caring, respectful, and supportive attitudes, and stigmatizing beliefs and attitudes (17).
Among other tools in the field of suicide stigma, the Suicide Stigma Scale (SOSS) was developed by Batterham et al. (18). This 16-item scale consists of three subscales: Glorification/normalization, stigma, and isolation/depression, all of which have demonstrated good psychometric properties (18). Additionally, the Personal Suicide Stigma Questionnaire (PSSQ) was created to measure personal suicide-related stigma (19). This 16-item scale contains three subscales: Self-blame, rejection, and minimization, which also show good psychometric properties (19). However, the STOSA Scale has fewer items and has been more strongly supported in the research literature for its psychometric properties, having been used in more studies.
Individuals with higher levels of stigma toward mental illness or suicide may be at greater risk for recurrence or further suicide attempts. Therefore, assessing the level of suicide-related stigma and developing strategies to reduce it is crucial (20). Measuring stigma at the individual level can help provide supportive and targeted interventions, while population-level assessments can track changes in public attitudes and beliefs. In Iran, there is currently no reliable scale to measure suicide stigma, and the absence of such a tool is evident. Additionally, examining the psychometric properties of scales in different cultural contexts can enhance the external validity of these tools.
2. Objectives
The present study was conducted to investigate the psychometric properties of the Persian version of the STOSA Scale.
3. Methods
3.1. Participants and Sampling
The statistical population of this study included all students at Ahvaz University of Medical Sciences during the 2021 - 2022 academic year. From this population, 291 individuals were selected using a convenience sampling method. According to Kline (21), the recommended sample size for confirmatory factor analysis (CFA) is approximately 200 participants, with greater accuracy achieved when the sample size exceeds 250 people (22). The inclusion criteria were: Being a student, proficiency in the Persian language, and being over 18 years old. The exclusion criterion was an unwillingness to participate. Due to the COVID-19 pandemic and its high transmission rate, data collection was conducted online through WhatsApp, Telegram virtual networks, and Skyroom, an online classroom platform. The study was conducted with the approval of the authorities at Ahvaz University of Medical Sciences, and ethical clearance was obtained.
The data were gathered using self-report scales. Participants were informed that all information collected would remain confidential, and they were free to withdraw from the study at any time. Participation did not entail any costs for the respondents. The data were analyzed using SPSS version 20 and LISREL version 8.80.
3.2. Measures
3.2.1. The Stigma of Suicide Attempt Scale
Scocco et al. (17) developed a 13-item scale to measure stigma related to suicide attempts among the general population, psychiatric patients, and those who have attempted suicide. The scale was standardized on 282 people from the general population, 113 psychiatric patients, 57 individuals who had attempted suicide, and 75 people who had lost a significant other to suicide. The STOSA Scale has a two-factor structure: One factor represents caring, respectful, and supportive attitudes, and the other relates to stigmatizing beliefs and attitudes. Responses are scored on a Likert Scale from "strongly agree" (4) to "strongly disagree" (1), with items 1, 2, 3, 4, 8, and 10 reverse-scored. A higher score indicates a greater level of stigma. Cronbach's alpha for this scale was reported to be 0.76 for the general and clinical populations, 0.76 for the clinical population, and 0.80 for the population who had attempted suicide (17).
The STOSA Scale was developed following guidelines for the intercultural adaptation of instruments (23). Initially, the original version of the STOSA Scale was translated from English into Persian by four clinical psychology professors. Any differences in translations were resolved through consensus. In the next step, two mental health professionals fluent in both Persian and English back-translated the Persian version into English. The final translation was reviewed by the authors. The Persian version of the STOSA Scale was then piloted on a sample of 20 individuals, and any issues were addressed to finalize the scale for implementation on the study sample.
3.2.2. Self-Compassion Scale (Short Form)
This 12-item scale asks participants to rate their responses on a 5-point Likert Scale ranging from 1 (almost never) to 5 (almost always). The short form assesses three bipolar components: Self-kindness vs. self-judgment, over-identification vs. mindfulness, and isolation vs. common humanity. The test-retest reliability of this scale has been reported as 0.92 (24). In a sample of Iranian students, Cronbach's alpha coefficient was 0.78 (25).
3.2.3. The Other as Shamer Scale-2
The Other as Shamer Scale-2 (OAS-2) contains 8 items used to measure external shame (26). Responses are scored from 0 (never) to 4 (always). This scale was standardized on a sample of 690 people, and its one-factor structure was confirmed. It demonstrated good convergent validity with other measures of shame, showing a high correlation (0.91) with the long form of external shame. It also showed a positive correlation with the Depression Anxiety Stress Scale (DASS-21) (26). The Cronbach's alpha coefficient for this scale is 0.82 (26).
3.2.4. The Stigma of Suicide Scale
This 16-item scale is designed to assess community members' stigmatic attitudes toward individuals who attempt suicide. Each item provides a one-word description of a person who dies by suicide. Responses are rated on a 5-point Likert Scale, ranging from (1) strongly disagree to (5) strongly agree. Higher scores indicate greater levels of stigma toward individuals who die by suicide. The scale has three subscales: Isolation/Depression, Stigma, and Glorification/Normalization. The overall internal consistency of the scale is 0.70 (18, 27).
3.3. Ethics Code
This study is derived from a project conducted at Ahvaz Jundishapur University of Medical Sciences, with the ethical approval code IR.AJUMS.HGOLESTAN.REC.1400.128.
3.4. Statistical Analysis
The data were cleaned and screened, with missing data accounting for less than 5% of the dataset. The construct validity of the STOSA Scale was examined using CFA, along with convergent and divergent validity assessments. Divergent and convergent validity were explored by calculating Pearson correlations between the STOSA Scale scores and those of the SCS-SF, OAS-2, and SOSS. Internal consistency was used to assess the reliability of the STOSA Scale, with Cronbach’s alpha employed to calculate this measure.
The fit of the two-factor model of the STOSA Scale was evaluated using several indices: Comparative Fit Index (CFI), Normed Fit Index (NFI), Non-normed Fit Index (NNFI), Goodness of Fit Index (GFI), Incremental Fit Index (IFI), root mean square error of approximation (RMSEA), Adjusted Goodness of Fit Index (AGFI), standardized root mean square residual (SRMR), and the X²/df Index. A value of X²/df less than 3 indicates a good fit, and for NFI, NNFI, CFI, RFI, IFI, and GFI, values above 0.90 indicate an acceptable model fit (28).
4. Results
In this study, 291 students aged between 18 and 51 years participated, with a mean age of 24.86 ± 5.76. Among the participants, 105 were male (36.1%) and 186 were female (63.9%). In terms of marital status, 181 participants (62.2%) were single, and 110 were married (37.8%). Regarding educational status, 21 students (7.2%) were master's degree holders, 143 students (49.1%) had a bachelor's degree, 80 students (27.5%) were pursuing a master's degree, and 47 students (16.2%) were pursuing a doctoral degree. Of the participants, 16 students (5.5%) reported a history of psychiatric disorders, while 275 students (94.5%) had no such history.
The results of the independent t-test showed a significant difference between men and women in the stigma of suicide attempt, with men displaying higher stigma levels than women (P < 0.05). Across the 291 individuals, the total STOSA scores ranged from a minimum of 19 to a maximum of 51. No participants scored the lowest possible score of 13 or the highest possible score of 52.
The correlation between the subscales and the overall scale was strong (Table 1). Additionally, the item-total correlation for the scale ranged from 0.33 to 0.73 (Table 2).
| Variables | Mean (Standard Deviation) | 1 | 2 | 3 |
|---|---|---|---|---|
| STOSA Scale | 35.64 (5.28) | 1 | 0.80 ** | 0.84 ** |
| Supportive attitudes | 16.98 (2.85) | 1 | 0.39 ** | |
| Stigmatizing beliefs and attitudes | 15.90 (2.95) | 1 |
Abbreviation: STOSA, Stigma of Suicide Attempt Scale.
a **: Correlation is significant at 0.01 level.
| Variable | A1 | A2 | A3 | A4 | A5 | A6 | A7 | A8 | A9 | A10 | A11 | A12 | A13 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| STOSA Scale | 0.35 ** | 0.50 ** | 0.560 ** | 0.58 ** | 0.33 ** | 0.56 ** | 0.67 ** | 0.51 ** | 0.51 ** | 0.53 ** | 0.63 ** | 0.73 ** | 0.58 ** |
Abbreviation: STOSA, Stigma of Suicide Attempt Scale.
a **: Correlation is significant at 0.01 level. The correlation of all items with the total scale is significant at the 0.01 level.
4.1. Internal Consistency
Cronbach's alpha coefficient for the overall scale and the dimensions of caring attitudes, respectful and supportive attitudes, and stigmatizing beliefs and attitudes were 0.81, 0.77, and 0.63, respectively.
4.2. Validity of the Stigma of Suicide Attempt Scale
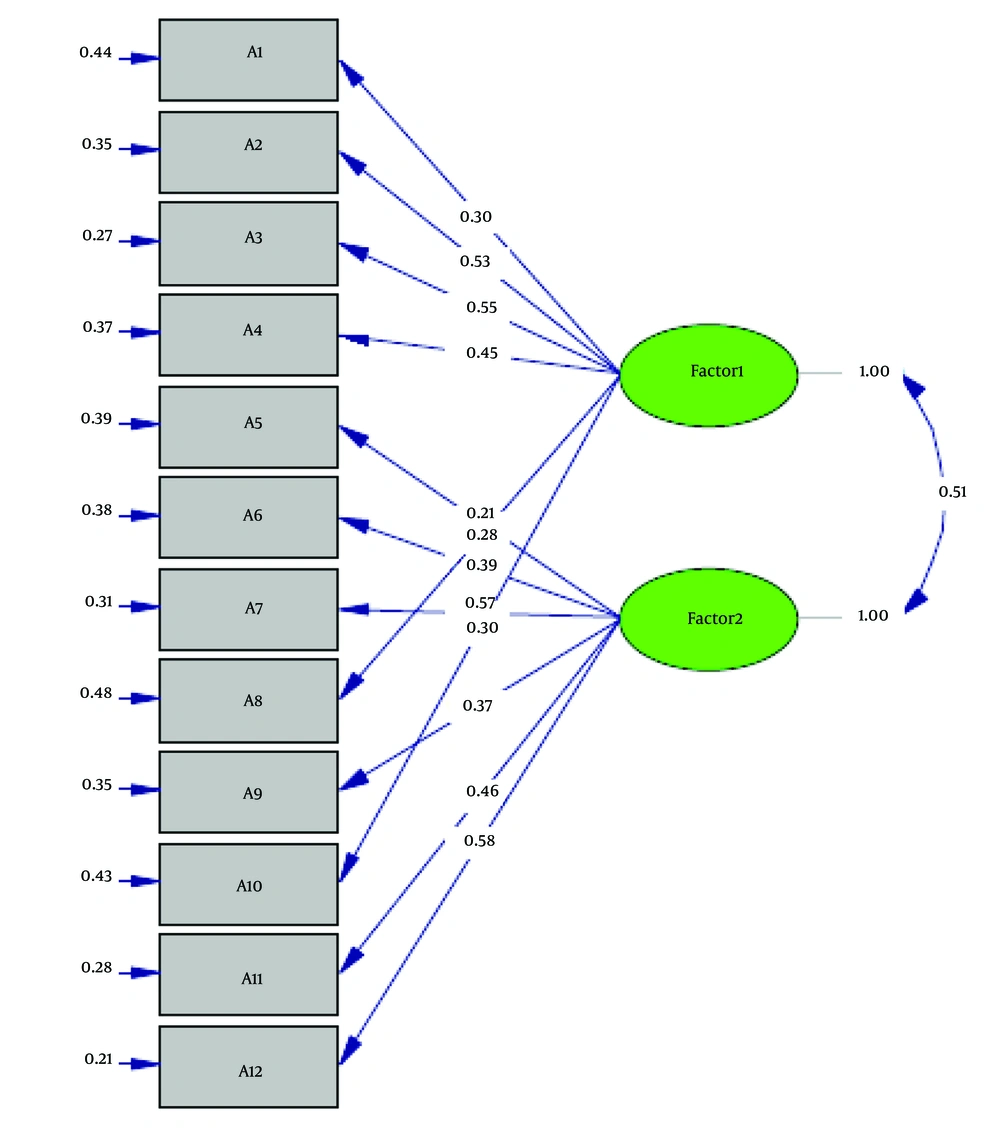
The validity of the STOSA scale was assessed using two methods: Confirmatory factor analysis. The fit of the two-factor structure of the STOSA scale was evaluated using several fit indices, including CFI, NFI, NNFI, GFI, AGFI, IFI, RMSEA, and SRMR. The results, shown in Table 3, support the fit of the two-factor model. The fit indices confirm the model’s adequacy, as demonstrated in Table 3 and Figure 1.
| Fit Indices | X2 | df | X2/df | SRMR | GFI | IFI | CFI | AGFI | NNFI | NFI | RMSEA |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Two-factor | 187.55 | 53 | 3.88 | 0.08 | 0.90 | 0.92 | 0.92 | 0.86 | 0.90 | 0.89 | 0.08 |
Abbreviations: NFI, Normed Fit Index; NNFI, Non-normed Fit Index; GFI, Goodness of Fit Index; IFI, Incremental Fit Index; RMSEA, root mean square error of approximation; AGFI, Adjusted Goodness of Fit Index.
4.3. Convergent and Divergent Validity
As shown in Table 4, the STOSA scale has a positive and significant correlation with the Suicide Stigma Scale and a negative and significant correlation with the SCS-SF. It also showed a positive but non-significant correlation with the External Shame Scale.
| Variables | SOSS | OAS-2 | SCS-SF |
|---|---|---|---|
| STOSA Scale | 0.21 ** | 0.06 | -0.11 |
| Supportive attitudes | 0.13 * | 0.02 | -0.05 |
| Stigmatizing beliefs and attitudes | 0.18 ** | 0.12 * | -0.13 * |
Abbreviations: STOSA, Stigma of Suicide Attempt Scale; SOSS, Stigma of Suicide Scale; OAS-2, Other as Shamer Scale-2; SCS-SF, Self-Compassion Scale (short form).
a **: Correlation is significant at 0.01 level. *: Correlation is significant at 0.05 level.
5. Discussion
The stigma associated with suicide is a major obstacle to suicide prevention, as it discourages individuals from seeking psychological help (29). Suicide is a complex phenomenon, influenced by various cultural, demographic, social, psychological, and environmental factors (30). Key objectives of suicide prevention programs include improving suicide literacy and reducing the stigma surrounding suicide (31). Stigma can undermine social cohesion, increase the likelihood of social isolation for key groups, and prevent individuals from seeking emergency health care. It can also deter them from adopting healthy behaviors. Although stigma is recognized globally, its experience and the discrimination associated with it vary from country to country, and even from city to city (32, 33).
The STOSA Scale provides a valuable tool for measuring stigma related to suicide attempts in the general population, psychiatric patients, and those who have attempted suicide. The aim of the present study was to investigate the psychometric properties of the Persian version of the STOSA Scale.
The results of our study support the two-factor structure of the STOSA Scale in a non-clinical sample. Our findings regarding the factor structure are consistent with the research conducted by Scocco et al. (17). In their study, Scocco et al. standardized the stigma scale on 282 people from the general population, 113 individuals with mental illness, 57 individuals who had attempted suicide, and 75 people who had lost a significant person to suicide. They also identified the same two-factor structure (17).
In this study, a significant difference was observed between the two sexes, with men scoring higher in stigma than women, which contrasts with the findings of Scocco et al. (17). The STOSA Scale demonstrated good internal consistency, consistent with the research by Scocco et al. (17). Scocco et al. found the internal consistency of the STOSA scale to be 0.76 in both the general and clinical populations, 0.76 in the clinical population, and 0.80 in the suicide attempt population (17). In our study, the correlation between items and the total score ranged from 0.33 to 0.73, while in Scocco et al.'s research, it ranged from 0.25 to 0.50, with items 5 and 6 falling below 0.30.
Our results also showed that the STOSA Scale has a positive and significant correlation with the Suicide Stigma Scale and correlates with shame, though this latter relationship was not statistically significant. These findings align with other research (17, 32, 34-36). Feelings of shame are frequently reported by individuals who have attempted suicide (16) and by those experiencing suicidal ideation (36). Shame and embarrassment may be linked to the anticipated experience of stigma.
Stigma can have severe consequences for individuals. Available data on shame suggest that shame may be considered the emotional counterpart of stigma, as it is associated with viewing oneself as inferior and inadequate (28). Our study also found that the STOSA Scale has a negative correlation with self-compassion, which is consistent with other studies (37-39). Self-compassion, defined as treating oneself with kindness and refraining from self-judgment, is a potential protective factor against stigma. Heath et al. (37) found that individuals with higher self-compassion reported less perceived self-stigma compared to those with lower self-compassion. This suggests that self-compassion may buffer the negative effects of perceived general stigma on predicted self-stigma by fostering psychological resilience.
Scocco et al. (17) demonstrated that the suicide attempt stigma scale can serve as a predictor of outcomes in therapeutic interventions. Considering that the transition from suicidal ideation to action is influenced by various traits or state characteristics, such as hopelessness, aggression, or impulsivity, stigmatizing suicide is unlikely to deter a depressed, desperate, or impulsive individual from acting on their thoughts (17). Given the absence of a tool in Iran to measure the stigma surrounding suicide attempts, this scale can facilitate increased research in this area. Reducing stigma (which does not mean trivializing or glorifying suicide) may enhance the relationship between suicidal individuals (whether contemplating or attempting suicide) and those they interact with, allowing for better communication and appropriate intervention. Since cultural and socio-economic factors shape societal views on suicide stigma (40), understanding stigma levels in each country is crucial to designing and implementing effective prevention strategies.
This study had several limitations. The sample was composed primarily of young, educated women from southwestern Iran, which may affect the findings and limit generalizability. Broader studies with populations from different age groups and geographic areas are recommended to provide further evidence of the scale's utility across diverse communities. Additionally, the study relied solely on self-report tools, and factors like social desirability bias, recall errors, and self-report inaccuracies may have influenced the results. Future research should consider incorporating more objective measures to assess individual experiences of stigma. The cross-sectional study design also precluded drawing causal conclusions. Furthermore, this study did not examine test-retest reliability, and future studies should focus on assessing this aspect. The use of convenience sampling may have limited the representativeness of the sample, and the relatively small sample size suggests that future studies should use larger samples to enhance the robustness of the findings. Future research could also focus on specific populations, such as individuals with particular mental health conditions or healthcare workers.
5.1. Conclusions
Identifying stigma is crucial, as it can have serious consequences. Measuring stigma is essential for developing targeted and supportive interventions and for tracking changes in public beliefs and attitudes. Suicide stigma had not been extensively studied in Iran, and the need for a tool to measure it was evident. This psychometric study contributes to the intercultural literature on the STOSA Scale and provides a reliable tool for both research and clinical use. The STOSA Scale demonstrates good validity and reliability within a non-clinical population sample.