1. Background
Chronic kidney disease (CKD) is characterized by kidney damage or an estimated glomerular filtration rate (eGFR) of less than 60 mL/min/1.73 m2 that has persisted for three months or more, regardless of its cause (1-3). Hemodialysis (HD) is the most prevalent treatment for CKD (1, 4)). The frequency of HD patients in Iran has increased considerably over the years (5, 6). Despite many technological and technical advances in the field of HD, problems during and after dialysis remain significant (7, 8).
Intradialytic hypotension (IDH) during dialysis is the most common serious complication of HD (9, 10), occurring in 10% to 12% of HD treatments (11). Hypotension greatly increases the overall morbidity of patients and not only limits fluid withdrawal during dialysis but can also cause severe vascular effects such as cerebral infarction and cardiac or mesenteric ischemia (12, 13). The pathophysiology of hypotension is related to the decrease in blood volume in the patient's circulation following ultrafiltration (UF), which results from the decrease in the osmolality of the extracellular space following the active removal of particles, especially sodium (14).
One of the recently proposed methods to prevent low blood pressure is changing the sodium concentration of the dialysis solution and the rate of fluid withdrawal (15). In several studies, over time, the regulated sodium concentration of dialysis gradually increased from 126.5 mEq/L in the 1940s to about 140 mEq/L in the 1990s, but there is still no consensus on the optimized concentration of sodium for dialysis (16). It is reported that elevated serum sodium concentration above 135 mmol/L directly increases blood pressure by stiffening the blood vessel wall (8). According to Flythe and Mc Causland, the dialyzed sodium concentration should be lower than serum sodium to allow diffusion and decrease serum sodium. Using a higher dialysate sodium concentration leads to "sodium loading", activating the thirst center in the hypothalamus, causing the patient to drink more water and subsequent weight gain (17).
Although there is conflicting evidence, many studies have shown that higher sodium in the dialysis fluid is associated with greater interdialysis weight gain and higher blood pressure (18, 19).
2. Objectives
Considering the importance of dialysis sodium regulation in HD patients, we decided to conduct a study to investigate the effect of low sodium levels in dialysis fluid in chronic HD patients.
3. Methods
3.1. Study Design and Participants
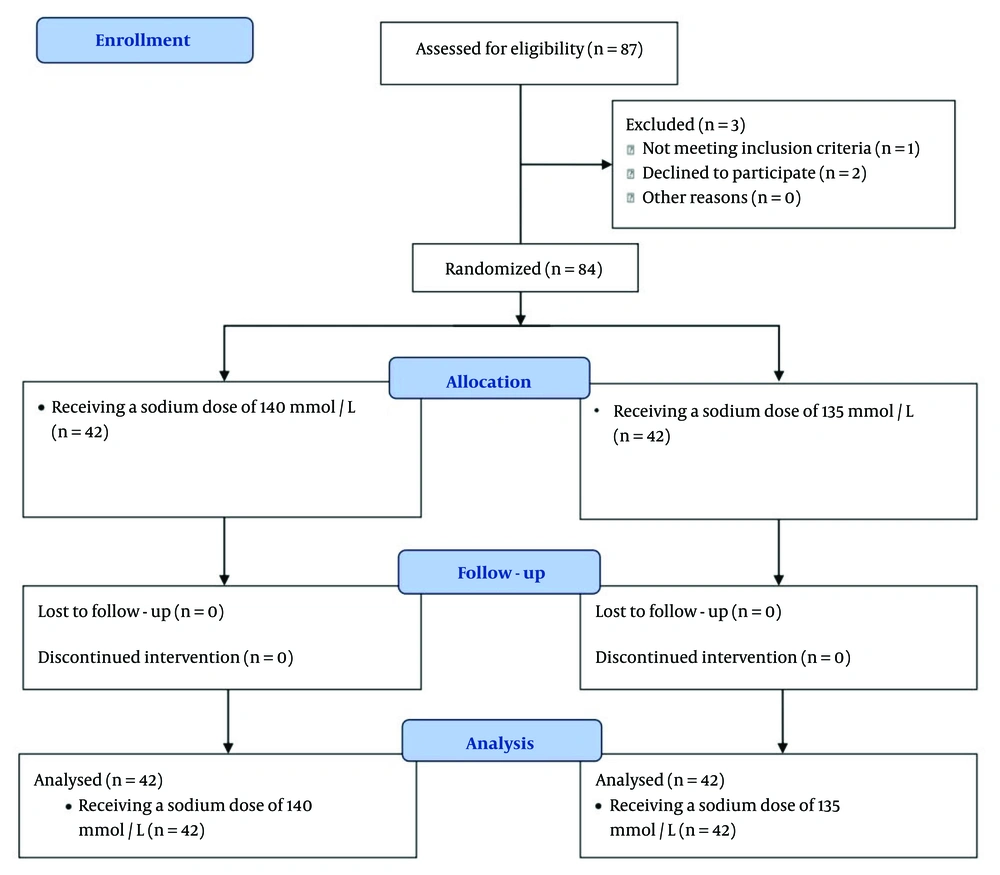
The current study is a double-blind randomized controlled clinical trial. Eighty-four patients who were referred to the dialysis centers of Golestan and Imam Khomeini Hospitals in Ahvaz, Iran, in 2023 were enrolled. Inclusion criteria included adults aged 18 to 75 years undergoing chronic HD for more than three months. Exclusion criteria included patients with active infection, the presence of ascites, uncontrolled underlying disease, frequent muscle cramps not attributable to low sodium, and sodium levels less than 130 mmol/L. The consolidated standards of reporting trials (CONSORT) flow diagram is shown in Figure 1, documenting the flow of participants through the different stages of the study.
The first group was treated with HD using a sodium concentration of 140 mmol/L, and the second group was treated with a sodium concentration of 135 mmol/L. Patients underwent HD sessions three times a week for 3 to 4 hours. During the study, one type of strainer was used in all sessions. In this double-blind study, both participants and data analysts were unaware of which dose of sodium was administered, helping to eliminate bias and ensure more reliable results.
At the beginning of the study, patients' weight, presence or absence of edema, sodium level, potassium level, and calcium electrolytes were checked. Sodium, potassium, and calcium levels in the patients' serum were checked monthly. Patients were evaluated by a nurse or physician for UF amount, mean arterial blood pressure before and after dialysis, weight changes, need for antihypertensive drugs, muscle cramps, and hypotension. The reduction in blood pressure, need for blood pressure medications, need for midodrine before dialysis, and reduction in UF were also investigated.
Before starting the study, patients' weight, systolic blood pressure (SBP), and diastolic blood pressure (DBP) were evaluated. At the end of the study (after three months), these parameters were checked again. All patients were followed up by the same nephrologist at predetermined times: Prior to treatment initiation and three months after treatment initiation. In this study, all members of the research team and patients were blinded to the treatment groups.
A simple randomization method was utilized. Each participant had an equal chance of joining any group. A random number generator or random number table was employed. We selected numbers from the random number chart. Group one (liquid sodium 140 mmol/L) was labeled 1 - 42, while group two (liquid sodium 135 mmol/L) was assigned numbers 43 - 84. We began at a certain spot in the random number chart, placing participants in the first group if the number fell within 1 - 42 and in the second group if it fell within 43 - 84. Any numbers outside of these ranges were disregarded as we continued assigning all participants.
3.2. Statistical Analysis
Statistical analysis was performed using SPSS software version 22. Quantitative variables were expressed as mean ± SD, while qualitative variables were presented as numbers (percentages). The Kolmogorov-Smirnov and Shapiro-Wilk tests were used to assess the normality of data distribution, and all data were found to be normally distributed. Intra-group comparisons were conducted using the paired t-test, while between-group comparisons were performed using the independent t-test. A P-value < 0.05 was considered statistically significant.
4. Results
The mean age of the 84 patients was 53.99 ± 14.61 years, with ages ranging from 23 to 75 years. Of all patients, 64% were female (54 patients). The mean duration of dialysis was 7.95 ± 3.45 years. Table 1 shows the descriptive characteristics of the studied patients.
| Variables | Result |
|---|---|
| Age (y) | 53.99 ± 14.61 |
| Gender | |
| Female | 54 (64) |
| Male | 30 (36) |
| Dialysis duration (y) | 7.95 ± 3.45 |
a Values are expressed as mean ± SD or No. (%).
Before dialysis, the SBP in patients receiving sodium doses of 135 and 140 mmol/L was 130.51 ± 6.92 mm Hg and 129.95 ± 7.45 mm Hg, respectively, with no significant difference observed between the two groups (P = 0.72). After dialysis, the SBP in patients receiving sodium doses of 135 and 140 mmol/L was 122.73 ± 7.01 mm Hg and 122.90 ± 6.97 mm Hg, respectively, which was not statistically significantly different (P = 0.91).
Before dialysis, there was no considerable difference in DBP between patients receiving sodium doses of 135 and 140 mmol/L (P = 0.56). After dialysis, the DBP in patients receiving sodium doses of 135 and 140 mmol/L was 74.94 ± 3.74 mm Hg and 75.51 ± 2.78 mm Hg, respectively, with no remarkable difference between the two doses (P = 0.42). More details are provided in Table 2.
| Variables and Dose of Sodium Intakes | Mean ± SD | P-Value |
|---|---|---|
| SBP before dialysis (mm/Hg) | 0.72 | |
| 135 mmol/L | 130.51 ± 6.92 | |
| 140 mmol/L | 129.95 ± 7.45 | |
| SBP after dialysis (mm/Hg) | 0.91 | |
| 135 mmol/L | 122.73 ± 7.01 | |
| 140 mmol/L | 122.90 ± 6.97 | |
| DBP before dialysis (mm/Hg) | 0.56 | |
| 135 mmol/L | 79.69 ± 3.77 | |
| 140 mmol/L | 80.09 ± 2.51 | |
| DBP after dialysis (mm/Hg) | 0.42 | |
| 135 mmol/L | 74.94 ± 3.74 | |
| 140 mmol/L | 75.51 ± 2.78 |
Abbreviations: SBP, systolic blood pressure; DBP, diastolic blood pressure.
Based on Table 3, before dialysis, the weight of patients receiving sodium doses of 135 and 140 mmol/L was 66.41 ± 14.08 kg and 71.96 ± 14.82 kg, respectively, with no significant difference observed between the two groups (P = 0.08). After dialysis, the weight of patients receiving sodium doses of 135 and 140 mmol/L was 63.99 ± 14.16 kg and 69.91 ± 14.69 kg, respectively, with no remarkable difference between the two groups (P = 0.06).
| Variables and Dose of Sodium Intakes | Mean ± SD | P-Value |
|---|---|---|
| Weight before dialysis (kg) | 0.08 | |
| 135 mmol/L | 66.41 ± 14.08 | |
| 140 mmol/L | 71.96 ± 14.82 | |
| Weight after dialysis(kg) | 0.06 | |
| 135 mmol/L | 63.99 ± 14.16 | |
| 140 mmol/L | 69.91 ± 14.69 |
Based on Table 4, the mean UF rate for sodium doses of 135 and 140 mmol/L was 1.87 ± 0.44 and 1.99 ± 0.40, respectively. There was no significant difference in the UF rate between the different sodium doses (P = 0.20).
| Variables and Dose of Sodium Intake | Mean ± SD | P-Value |
|---|---|---|
| UF rate | 0.20 | |
| 135 mmol/L | 1.87 ± 0.44 | |
| 140 mmol/L | 1.99 ± 0.40 |
Abbreviation: UF, ultrafiltration.
5. Discussion
The present study aimed to investigate the effect of low sodium levels in dialysis fluid on the hemodynamics of patients undergoing chronic HD. Our findings showed no substantial difference in patients' weight, systolic, and DBP after dialysis with sodium doses of 135 and 140 mmol/L (P > 0.05).
In the study by Manji et al., which aimed to investigate the effect of lower dialysis sodium concentration on weight loss or gain between dialysis sessions, one group of patients received a dialysis sodium concentration of 137 mEq/L and the other group received 140 mEq/L. There was no remarkable difference in weight gain between the two groups, and the mean systolic and DBP s were not statistically significant (20). The findings of this study are consistent with our results.
Similarly, Beduschi et al. showed no correlation between dialysate sodium concentration and interdialysis weight gain. They found no significant differences in interdialysis weight gain or blood pressure when comparing doses of 135 and 138 mmol/L (16). In the study by Thein et al., there was no significant difference in interdialysis weight gain between 141 and 138 mmol/L dialysate sodium; however, there was a significant reduction in blood pressure with less dialysate sodium used (21).
Contrary to our findings, the study by Mariani et al. reported that low dialysate sodium concentration reduces interdialytic weight gain (IDWG) in patients undergoing chronic HD (22). In a study conducted by Akdag et al. to investigate the effect of low sodium dialysis on ambulatory blood pressure measurement parameters in HD patients, the results showed no significant decrease in both groups in terms of 24-hour DBP and daily DBP. However, weight gain during dialysis decreased significantly after 6 months in the low sodium dialysis group (23). The findings of this study in terms of blood pressure align with our results, although the findings regarding weight gain during dialysis are inconsistent with ours. The difference in sample size may account for this discrepancy.
Aybal Kutlugün et al. demonstrated that lowering dialysate sodium concentration reduces endothelial dysfunction and provides better control of IDWG and blood pressure, but increases dialysis-related symptoms. The sodium concentrations investigated in the study by Aybal Kutlugün et al. were 143 mEq/L and 137 mEq/L (24). These findings contrast with our results. The differences in dialysis duration and sodium doses may account for this discrepancy.
There is a theory that each person has an individual osmolar adjustment point based on parameters such as dietary salt consumption, sodium excretion through urine, tissue sodium reserves, and the body's physiological response to sodium. For this reason, changes in dialysate sodium concentration may not significantly affect interdialysis weight gain and blood pressure unless sodium levels are individually determined (25).
Contrary to our findings, Kim et al.'s study showed that a low sodium dose of 135 mmol/L compared with a dose of 140 mmol/L resulted in a significant reduction in IDWG and a reduction in systolic and DBP (26). Moreover, the main findings of Dunlop et al.'s study indicated that low sodium in the dialysis fluid improved blood pressure and reduced salt and water loss between dialysis treatments but increased the number of cramps (8).
The different sample sizes, sodium doses, duration of the effect of low sodium levels in dialysis fluid, and various study designs in existing studies differ from our study, and these differences may explain the discrepancies. It is not certain that low sodium in dialysis fluid improves the condition of patients undergoing HD, as there is a combination of possible beneficial and adverse effects, and the available research studies are not sufficient. Several reports have emphasized the need for a large, crossover, well-designed study to demonstrate a clear causal relationship.
The limitations of this study include the small sample size and short follow-up period, as it takes time for the sodium-reducing effects of dialysis to decrease extracellular volume and affect blood pressure reduction.
5.1. Conclusion
There was no significant difference in weight, systolic, and DBP before and after dialysis between the two groups receiving sodium concentrations of 135 and 140 mEq/L. Based on our findings, the use of lower dialysate sodium concentrations does not appear to be beneficial in altering weight gain or blood pressure. However, further studies with larger sample sizes, considering residual renal function and a longer duration of effect on blood pressure, are warranted.