1. Background
Migraine is a neurological, chronic, and often lifelong disease that is seen all over the world. It is estimated to affect over one billion people worldwide (1) and about 12% of the population. However, the prevalence of migraine is reported to be significantly higher (between 27.6% and 48.6%) by neurologists (2). The negative consequences of migraine affect different aspects of patients' lives, such as health, productivity, and quality of life (3, 4), and have profound effects on family, colleagues, and the community (5, 6). Also, migraines are the leading cause of disability in people under the age of 50 (especially women) worldwide (1). The social and economic aspects of migraines make up a significant portion of the costs incurred by the individual and society (7). Stress-related disorders such as depression and anxiety should not be overlooked (8). The effect of migraine on various aspects of the patients' socio-economic and personal life makes it necessary to use the best and most effective treatments. Although numerous pharmacological treatments have been proposed by experts for migraine, the results of a study showed that the common treatments do not comply with the current guidelines, especially for patients with severe symptoms (9). Also, a high percentage of people who take drugs for acute migraine are at high risk for drug-induced headaches (10). Therefore, scientists have suggested that efforts are needed to improve migraine management practices (11). A recent review showed that many complementary and integrated treatment options are useful for the management and prevention of migraine attacks (12). Understanding the effectiveness and potential risks of these methods can empower providers and patients (13, 14).
Researchers believe that connective tissue massage stimulates skin-visceral reflexes, regulates the autonomic nervous system, and reduces the dysfunction of damaged internal organs. It can be considered in the treatment of blood circulation problems, visceral disorders, sympathetic pain, hormonal disorders, and mental disorders (15). Some studies have considered the role of massage therapy (by therapists) with a variety of protocols in the prevention and management of migraine symptoms and attacks, and conflicting results have been reported (16-19). Family members of chronically ill patients are important, inexpensive, and available sources of support. It seems logical to utilize their competencies to promote patients' psychological adjustment, disease management, and outcomes. Family-based care, focused on family members' information and respecting patients' opinions, can improve quality of life at home and in the hospital by strengthening intrinsic motivation for self-care (20). Limited studies have considered the role of family in massage therapy in a migraine setting. This study, for the first time, has addressed the empowerment of family members of migraine patients through education and the use of massage therapy in managing migraine symptoms.
2. Objectives
The study aims to determine the effect of massage therapy by trained family members on headache and HIT in migraine patients.
3. Methods
3.1. Study Design
This double-blinded randomized controlled trial was designed to determine the effect of massage on headache and HIT in migraine patients in Bandar Abbas in the Hormozgan province, Iran.
3.2. Study Participation and Sampling
All migraine patients referred to the private offices of internal neurologists who met the inclusion criteria were included in the study. The sample size was calculated to be 90 dyads of migraine patients and family members (30 dyads for each group), according to a previous study (21) and the following formula with a significance level of 0.05 and power of 90%, a standard deviation of 1.2 for headache, and an effect size of 0.97 according to the between-groups minimum significant difference in mean changes of Visual Analog Scale (VAS) score for headache.
Sampling was initially purposeful and based on inclusion criteria. Then, the eligible samples were assigned into three groups—massage, touch, and control—through the random minimization method (22), based on gender classes (male and female) and length of disease (less than 5 years and more than 5 years) categories. Randomization units were included in the study individually. The first sample in each class in one of the study groups was allocated by random drawing through a sealed envelope. The entry of the next sample with the same class between the remaining two groups was also done by the lottery method. The third sample with the same characteristics was assigned to the last group in the same class. This process continued until reaching the desired sample size.
3.3. Inclusion Criteria
Inclusion criteria for patients included: Confirmation of migraine diagnosis (with or without aura) by a neurologist using the international index to diagnose headache for at least one year, headaches occurring at least four times a month, age > 18 years, absence of other neurological and severe physical disorders, no addiction (to drugs and alcohol), absence of skin lesions at head and neck areas, not taking anticoagulants, no cardiovascular disease, and not receiving complementary treatments at least during the last three months. Inclusion criteria for family members: Age > 18 years, living with the patient, having sufficient physical, mental, and cognitive ability to learn and apply the massage protocol, and no drug abuse.
3.4. Exclusion Criteria
Exclusion criteria include: The patient's or family's withdrawal, forgetting more than two massage sessions, change in medication regimen, and occurrence of critical conditions.
3.5. Intervention
All subjects received routine care (drug regimen prescribed by the neurologist, diets, lifestyles, etc.) which they followed for at least one month before entering the study. In the massage group, family members were taught (for 4 to 6 hours in two or three sessions) by a trained researcher in a private place. To ensure learning, family members repeated the massage protocol with the patient in the presence of the researcher, and an educational video was provided to them. A WhatsApp group was created to facilitate interactions, and a phone number was provided for necessary contacts.
The massage was performed in a quiet, private, and clean environment, with proper air conditioning and privacy. The patient wore comfortable clothing, with his/her shoulders and neck accessible, lying on a comfortable mattress, and family members sat above the patient. The therapists also wore comfortable, soft clothing so that they could perform the massage movements gently. The therapist ensured that his/her nails were short and did not wear a ring to avoid damaging the patient's skin. Hands were warmed and smeared with "Firooze" baby oil.
The massage was performed on the trapezius muscles using the roll technique (3 minutes by pulling the skin up with the thumb). It started from the midline of the spine and continued to the lateral end of the scapula to the armpit on both sides and from the shoulders near the scapula to the base of the neck.
Kneading technique (8 minutes) was performed for neck massage, in which deep and compressing pressure was applied to the underlying muscles. Patients were placed in a prone position, with the fingers of both hands extending from the back of the occiput to the neck as far as the neck and below the scapular area. Then the patient was placed in a lateral position and then supine, and the massage of the upper trapezius muscle attached to the neck was continued with the fingertips.
The occipitofrontalis muscle was massaged using the muscle stretching technique (2 minutes). The patient was placed in the supine position, with the palm of one hand on the forehead moving it down or towards the eyebrows, and the palm of the other hand under the sub-occipital muscle moving upwards at the same time, so that it felt like the scalp was moving forward and backward.
The scalp was massaged with three techniques: Effleurage (2 minutes), kneading (2 minutes), and vibration (2 minutes). The therapist placed the fingers of both hands on both sides of the patient's temporal area and skull and gently massaged in a circular manner. In the kneading technique, massage was performed on the whole skull and in the occipital frontal area and above the afferent massage area by the movements of all fingers. In the vibration technique, the palms of both hands were placed on the massage area (same as kneading), and back and forth movements were done in the form of vibration.
Forehead massage was performed using the kneading technique (2 minutes) and effleurage (2 minutes). The kneading method was executed using two, three, or four fingers, massaging from the midline of the forehead in the frontal and temporal direction. In the effleurage method, all the fingers of the hand were used, drawing from the midline in a curved way around and down. One minute was spent rotating the patient in each stage. The massage was performed with moderate pressure.
The intervention was conducted twice a week with a minimum interval of 48 hours between sessions, and each session lasted about 25 - 30 minutes over a period of 4 weeks. The subjects in the touch group received superficial touch with the same duration and locations as the massage group. The control group received no intervention. The massage and touch interventions were implemented according to the study protocol without considering the migraine attacks.
3.6. Data Collection Tool and Technique
Data collection tools included the patient and family member’s demographic characteristics, as well as the VAS for headache intensity as the primary outcome and the headache impact test-6 (HIT-6) as the secondary outcome. Patients were asked to recall the average intensity of headache by choosing a point between zero and ten. Then the pain score was determined and recorded for them using a ten-point ruler. The number zero means "no headache", and the number ten means "the most severe headache imaginable".
The HIT-6 asked the patient to answer six 5-point questions about the impact of headaches on quality of life as "never", "rarely", "sometimes", "often", and "always", graded with 6, 8, 10, 11, and 13 points, respectively. The total number of scores ranged between 36 and 78. A score of less than 49 indicated "no or little effect", a score of 50 - 55 indicated "relative impact", a score of 56 to 59 indicated "significant impact", and a score of 60 or higher indicated a "severe effect". The reliability of this tool has been confirmed with a Cronbach's alpha coefficient of 0.75 - 0.95. Also, HIT-6 was strongly correlated (-0.86 to -0.59) with the Migraine-Specific Quality-of-Life Questionnaire (23).
Measurements were performed at three times (baseline, immediately, and one month after completing the intervention). Data collection was done by the researcher's colleague, who was blind to the allocation of samples in the study groups, through face-to-face interviews at baseline and telephone interviews at the two other measurements. The data analyzer was also blinded.
3.7. Ethical Consideration
The project was approved by the research council and ethics committee in biomedical research of Rafsanjan University of Medical Sciences with the code of ethics: IR.RUMS.REC.1399.176, and registered at the Iranian Clinical Trial registry with the code: IRCT20201116049403N1, while respecting confidentiality. Informed and written consent was obtained from patients. Patients were assured that participation in the study would not affect their routine quality of care.
3.8. Statistical Analysis
Data analysis was performed using SPSS software V.22 (by IBM Company, USA) employing the Shapiro-Wilk test, chi-square test, repeated measures ANOVA, and statistical modeling at a significance level of 0.05.
4. Results
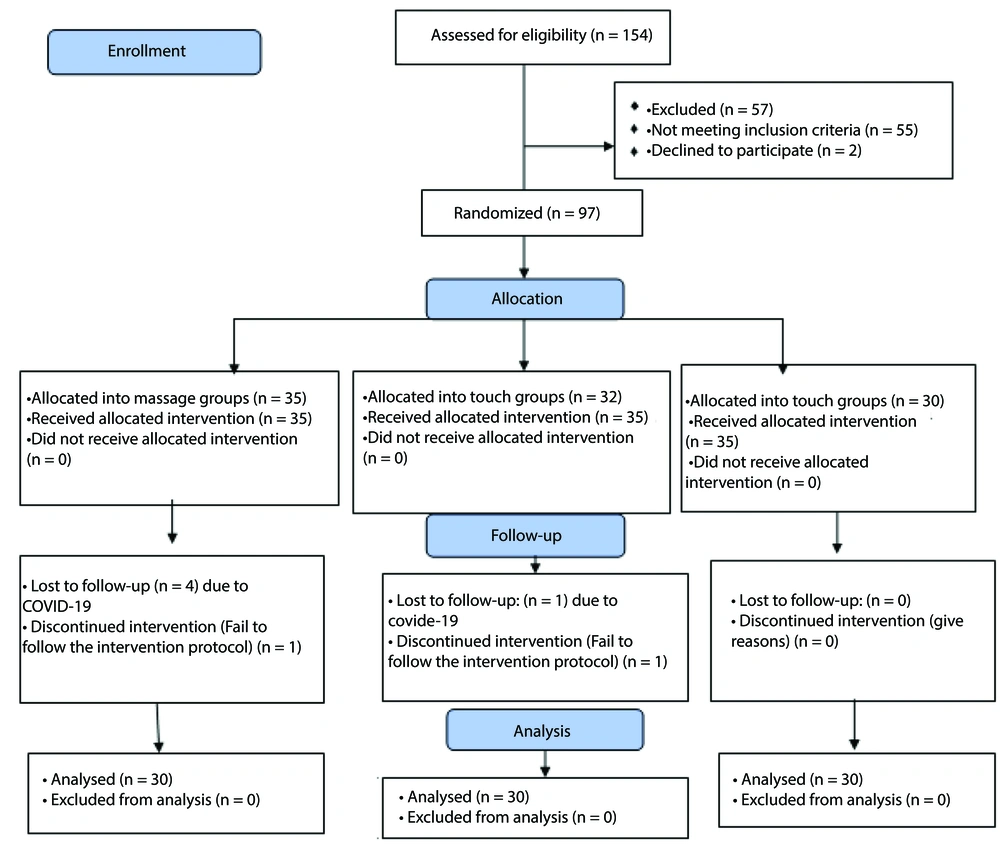
Finally, the data from 90 dyads (30 in each group) were analyzed. The details of the sampling are shown in Figure 1.
Based on the Shapiro-Wilk test results, the distribution of quantitative variables was normal. The results of data analysis showed that the mean ± SD of the patient's age was 35.23 ± 8.08, with a minimum of 19 and a maximum of 59 years. The gender distribution was 32 (33.7%) male and 57 (63.3%) female patients. The mean ± SD of the family member's age was 35.62 ± 9.25, with a minimum age of 18 and a maximum of 66 years. The highest frequency of family relationship was for spouses at 37 (41.1%), and the lowest was for fathers at 1 (1.1%). There was no statistically significant difference between the studied groups in terms of demographic characteristics such as patient's age, gender, education, marital status, and job (Table 1).
| Variables | Groups (N = 30) | P-Value | |||
|---|---|---|---|---|---|
| Massage | Touch | Control | Pearson Chi-Square Test | One-Way ANOVA | |
| Gender | 1.000 | - | |||
| Male | 11 (36.7) | 11 (36.7) | 11 (36.7) | ||
| Female | 19 (63.3) | 19 (63.3) | 19 (63.3) | ||
| Education | 0.336 | - | |||
| Diploma and under diploma | 9 (30) | 8 (26.7) | 14 (46.7) | ||
| BSc. | 15 (50) | 18 (60) | 14 (46.7) | ||
| MSc. and PhD. | 6 (20) | 4 (13.3) | 2 (6.7) | ||
| Marital status | 1.000 | - | |||
| Single | 9 (30) | 9 (30) | 9 (30) | ||
| Married | 21 (70) | 21 (70) | 21 (70) | ||
| Job | 0.185 | - | |||
| Employed | 13 (43.3) | 9 (30) | 16 (53.3) | ||
| Unemployed | 17 (56.7) | 21 (70) | 14 (46.7) | ||
| Age (mean ± SD) | 37.10 ± 7.59 | 36.30 ± 8.47 | 32.30 ± 7.56 | - | 0.046 b |
Comparison of Demographic Characteristics of the Patients Between the Study Groups a
The results of Mauchly’s Sphericity test showed that the correlation coefficients of pain and HIT-6 scores at three consecutive measurements were significantly different (P = 0.001). Therefore, the precondition for the correlation equation was not accepted, and the Greenhouse-Geisser correction coefficient was used to report P-values. The results of the multivariate test for the examination of time, group, and the interaction between time and group effects showed a statistically significant difference, prompting the application of statistical modeling. The results of the multivariate test are shown in Table 2.
| Variables | Group (N = 30) | P-Value a | ||||
|---|---|---|---|---|---|---|
| Massage | Touch Group | Control Group | Time Effect | Time × Group Effect | Group Effect | |
| Pain score | 0.001 | 0.001 | 0.001 | |||
| Before intervention | 7.27 ± 1.17 | 7.30 ± 0.98 | 7.37 ± 1.03 | |||
| After intervention | 4.60 ± 1.58 | 6.63 ± 1.15 | 7.17 ± 0.95 | |||
| One month after intervention | 6.80 ± 1.18 | 7.17 ± 1.11 | 7.07 ± 1.23 | |||
| HIT score | 0.001 | 0.001 | 0.001 | |||
| Before intervention | 55.63 ± 4.51 | 57.47 ± 3.13 | 55.97 ± 4.08 | |||
| After intervention | 49.03 ± 5.06 | 55.67 ± 3.27 | 55.93 ± 4.27 | |||
| One month after intervention | 53.27 ± 3.82 | 56.8 ± 3.22 | 55.70 ± 4.60 | |||
The Mean and Standard Deviation of Pain and Headache Impact Test Scores Changes Across the Study Groups at Three Times of Measurement
4.1. Within Group Comparison
Evaluation of the pain and HIT-6 score changes within each group showed that, in the massage group, the pain and HIT-6 scores after completing the intervention decreased significantly compared to the baseline (P = 0.001) and one month after completing the intervention (P = 0.002, P = 0.001, respectively). The pain and HIT-6 scores one month after the end of the intervention were significantly lower than after the intervention (P = 0.001).
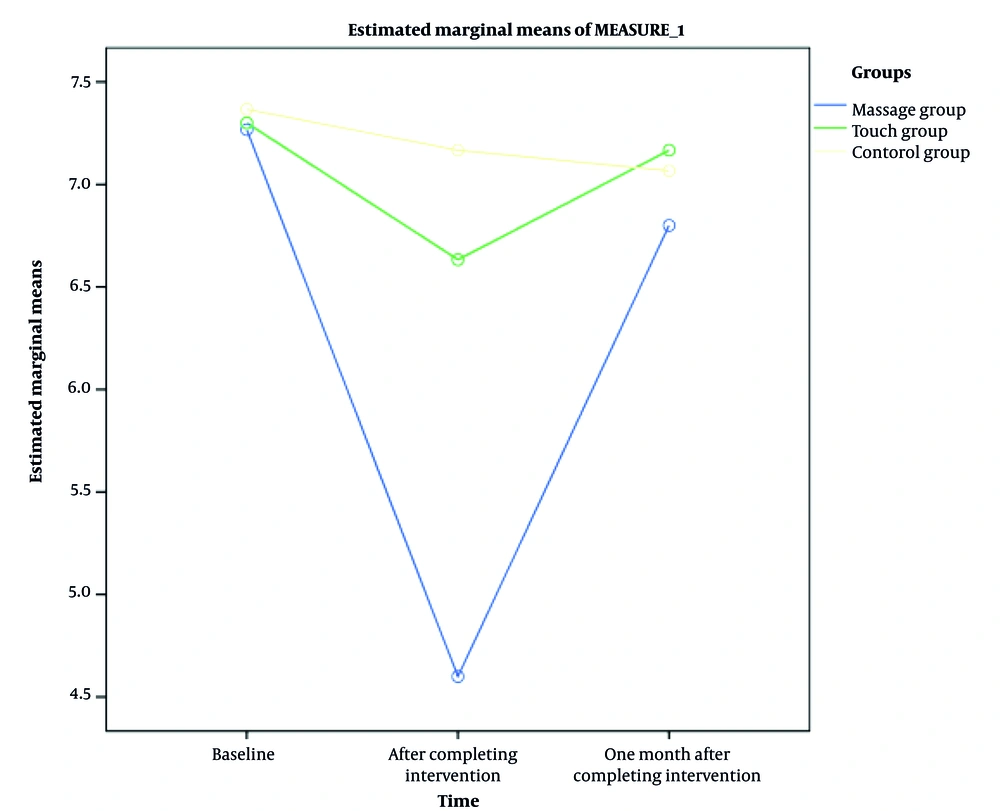
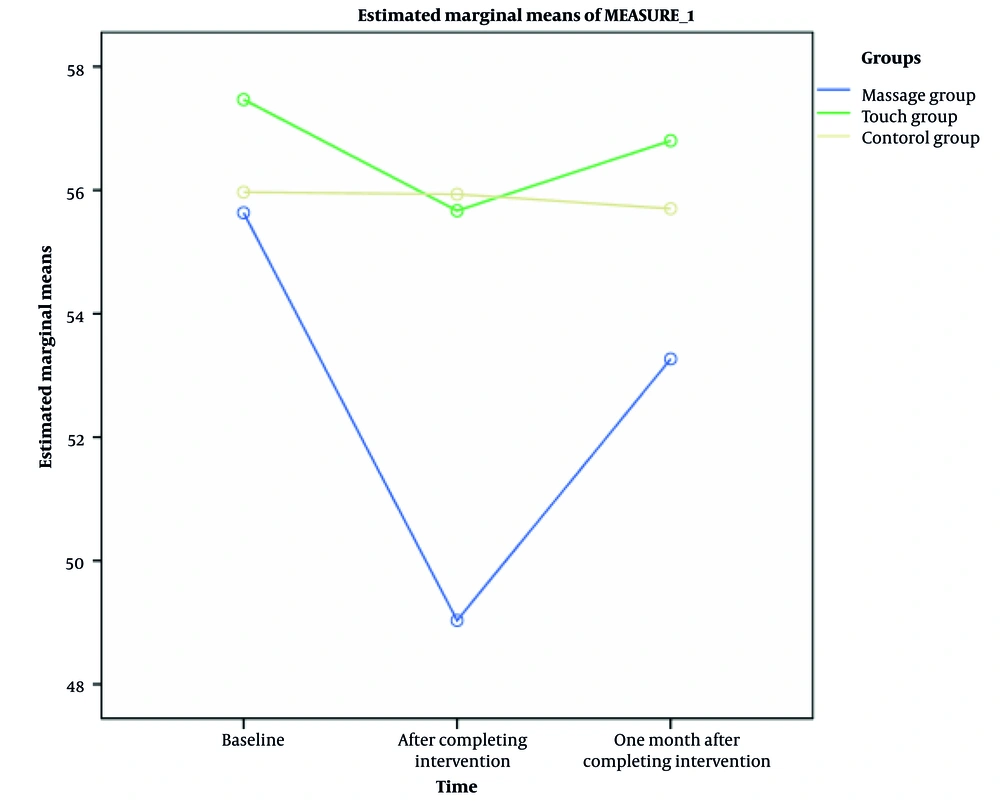
In the touch group, the pain and HIT scores after completing the intervention decreased significantly compared to baseline (P = 0.006, P = 0.002, respectively), but there was no difference between the pain and HIT-6 scores after the intervention (P = 0.973, P = 0.141). Moreover, the pain and HIT-6 scores one month after completing the intervention were significantly lower than the baseline (P = 0.041, P = 0.033, respectively). In the control group, pain did not show a significant change in three consecutive measurements (Tables 3 and 4), (Figures 2 and 3).
| Time of Measurement | Massage Group | Touch Group | Control Group | |||
|---|---|---|---|---|---|---|
| Mean ± SE | P-Value | Mean ± SE | P-Value | Mean ± SE | P-Value | |
| Baseline | ||||||
| After completing the intervention | 2.660 ± 0.209 | 0.001 | 0.667 ± 0.209 | 0.006 | 0.200 ± 0.209 | 1.000 |
| One month after completing intervention | 0.467 ± 0.135 | 0.002 | 0.133 ± 0.135 | 0.973 | 0.300 ± 0.135 | 0.085 |
| After completing the intervention | ||||||
| Baseline | -2.660 ± 0.209 | 0.001 | -0.667 ± 0.209 | 0.006 | -0.200 ± 0.209 | 1.000 |
| One month after completing intervention | -2.200 ± 0.212 | 0.001 | -0.533 ± 0.212 | 0.041 | 0.100 ± 0.212 | 1.000 |
| One month after completing intervention | ||||||
| Baseline | -0.467 ± 0.135 | 0.002 | -0.133 ± 0.135 | 0.973 | -0.300 ± 0.135 | 0.085 |
| After completing the intervention | 2.200 ± 0.212 | 0.001 | 0.533 ± 0.212 | 0.041 | -0.100 ± 0.212 | 1.000 |
Within Groups Pairwise Comparison of Pain Score's Mean Changes at Three Times of Measurements
| Time of Measurement | Massage Group | Touch Group | Control Group | |||
|---|---|---|---|---|---|---|
| Mean ± SE | P-Value | Mean ± SE | P-Value | Mean ± SE | P-Value | |
| Baseline | ||||||
| After completing the intervention | 6.600 ± 0.509 | 0.001 | 1.800 ± 0.509 | 0.002 | 0.033 ± 0.509 | 1.000 |
| One month after completing intervention | 2.367 ± 0.331 | 0.001 | 0.667 ± 0.331 | 0.141 | 0.267 ± 0.331 | 1.000 |
| After completing the intervention | ||||||
| Baseline | -6.600 ± 0.509 | 0.001 | -1.800 ± 0.509 | 0.002 | -0.033 ± 0.509 | 1.000 |
| One month after completing intervention | -4.233 ± 0.437 | 0.001 | -1.133 ± 0.437 | 0.033 | 0.233 ± 0.437 | 1.000 |
| One month after completing intervention | ||||||
| Baseline | -2.367 ± 0.331 | 0.001 | -0.667 ± 0.331 | 0.141 | -0.267 ± 0.331 | 1.000 |
| After completing the intervention | 4.233 ± 0.437 | 0.001 | 1.133 ± 0.437 | 0.033 | 0.233 ± 0.437 | 1.000 |
Within Groups Pairwise Comparison of Mean Difference of Headache Impact Test Score at Three Times of Measurements
4.2. Between Group Comparisons
There was no significant difference in between-groups pairwise comparison in terms of pain and HIT score at baseline (P > 0.05). After completing the intervention, the mean pain score in the massage group was significantly lower than in the touch (P = 0.045) and control groups (P = 0.001), and in the touch group, it was lower than in the control group (P = 0.003). Also, after completing the intervention, the HIT-6 score in the massage group was significantly lower than in the touch and control groups (P = 0.001). There was no significant difference between the touch and control groups (P = 1.000).
At one month after completing the intervention, the massage group had significantly lower HIT-6 scores compared to the touch group (P = 0.002). However, at this stage, no statistically significant difference was observed between the scores of the massage and control groups (P = 0.055) and the touch and control groups (P = 0.841) (Tables 5 and 6), (Figures 1 and 2).
| Groups | Baseline | After Completing Intervention | One Month After Completing Intervention | |||
|---|---|---|---|---|---|---|
| Mean ± SE | P-Value | Mean ± SE | P-Value | Mean ± SE | P-Value | |
| Massage group | ||||||
| Touch group | -0.033 ± 0.276 | 1.000 | -2.033 ± 0.326 | 0.001 | -0.367 ± 0.304 | 0.694 |
| Control group | -0.100 ± 0.276 | 1.000 | -2.567 ± 0.326 | 0.001 | -0.267 ± 0.304 | 1.000 |
| Touch group | ||||||
| Massage group | 0.033 ± 0.276 | 1.000 | 2.033 ± 0.326 | 0.001 | 0.367 ± 0.304 | 0.694 |
| Control group | 0.67 ± 0.276 | 1.000 | -0.533 ± 0.326 | 0.315 | 0.100 ± 0.304 | 0.1000 |
| Control group | ||||||
| Massage group | 0.100 ± 0.276 | 1.000 | 2.657 ± 0.326 | 0.001 | 0.267 ± 0.304 | 1.000 |
| Touch group | 0.067 ± 0.276 | 1.000 | 0.533 ± 0.326 | 0.315 | -0.100 ± 0.304 | 1.000 |
Between Groups Pairwise Comparison of Mean Difference of Pain Score
| Groups | Baseline | After Completing Intervention | One Month After Completing Intervention | |||
|---|---|---|---|---|---|---|
| Mean ± SE | P-Value | Mean ± SE | P-Value | Mean ± SE | P-Value | |
| Massage plus usual care group | ||||||
| Touch plus usual care group | -1.833 ± 1.021 | 0.228 | -6.633 ± 1.102 | 0.001 | -3.533 ± 1.013 | 0.002 |
| Usual care only group | -0.333 ± 1.021 | 1.000 | -6.900 ± 1.102 | 0.001 | -2.433 ± 1.013 | 0.055 |
| Touch plus usual care group | ||||||
| Massage plus usual care group | 1.833 ± 1.021 | 0.228 | 6.633 ± 1.102 | 0.001 | 3.533 ± 1.013 | 0.002 |
| Usual care only group | 1.500 ± 1.021 | 0.437 | -0.267 ± 1.102 | 1.000 | 1.100 ± 1.013 | 0.841 |
| Usual care only group | ||||||
| Massage plus usual care group | 0.033 ± 1.021 | 1.000 | 6.900 ± 1.102 | 0.001 | 2.433 ± 1.013 | 0.055 |
| Touch plus usual care group | 1.500 ± 1.021- | 0.437 | 0.267 ± 1.102 | 1.000 | -1.100 ± 1.013 | 0.841 |
Between Groups Pairwise Comparison of Mean Difference of Headache Impact Test
5. Discussion
In summary, the results of this study showed that massage therapy by family members in migraine patients could improve pain and HIT scores in the short term. In the long term (after one month), this effect on pain was not permanent, but its significant effect was visible on HIT. Although the literature shows the wide use of complementary medicine by migraine patients (12, 13, 24, 25), and massage therapy is introduced as the most used body-based practice (26), it seems that family-centered massage therapy is less respected by researchers, with most studies focusing on therapists, medical centers, and migraine prevention (13, 27) and treatment (12).
Although researchers haven't reported any biological markers or clinical characteristics predictive of response to specific migraine preventive drugs (28), they believe that many complementary and integrated treatment options may be useful and can empower patients (24). Results of a recent RCT showed that massage therapy alone and in combination with mobilization had a positive effect on headache-induced disability (18). Regardless of the similarity with the results of the present study, it should be acknowledged that their massage protocols were different. Similarly, Gupta and Kanase, in 2021, showed that deep neck muscle activation effectively reduced HIT, headache frequency, and intensity experienced by students (26). These results can be justified by common pathophysiological approaches (29) that researchers have introduced between migraine and cervicogenic headache.
Although these researchers have claimed some limitations due to the lack of a control group for comparison and the small sample size, it should be mentioned that part of the pain relief should be attributed to the effects of skin stimulation and placebo effects, which occur due to the reduction of stress hormone levels and muscle stretching (30). Also, the massage protocol is an important factor. Toprak Celenay et al. showed that connective tissue massage with education had a significant change in pain, associated symptoms (except vomiting), medication use, HIT-6, and migraine disability assessment scale compared to the control group (31). In contrast, Rostron, in the results of a case report, found a negative effect of Swedish massage on headache disability in a migraine patient with cervical spondylitis (16). However, the limitation in generalizing the results of case reports should not be overlooked.
The positive clinical impact of this intervention on patients' quality of life and headache management was evident throughout the study; however, this study did not confirm the long-term pain-relieving effects of massage. Few studies have investigated the long-term effects of regularly recurring massage therapy on migraine headaches. The researchers suggest that further studies are needed to determine the durability of integrative approaches in pain management.
5.1. Limitation and Recommendations
In this study, researchers tried to obtain rigorous results through scientific design, but some limitations, such as the small sample size and the effect of patients' lifestyles that could affect the migraine episode and its pattern, were beyond our precise control and cannot be ignored. It is necessary in future research to clearly determine in which patients and at what stage of the disease this method can be used therapeutically. Therefore, more research with long-term follow-up or the use of objective outcome measures is recommended.
5.2. Conclusions
The results of this study showed that massage therapy by trained family members as a complementary therapy can be useful in the management of headaches in the short term and HIT in both the short and long term in migraine patients. This means that healthcare professionals can empower the family members of migraine patients to manage migraines in an easy, accessible, low-cost, uncomplicated method within their natural living environment.