1. Background
Gestational diabetes mellitus (GDM) is a growing global health problem and one of the most common complications of pregnancy (1). According to the World Health Organization, high blood glucose levels during pregnancy, including elevated levels prior to pregnancy, are classified as GDM (2). The prevalence of GDM varies widely, with rates reported between 5 - 18% in the United States (3, 4) and 1.3 - 18.6% across different regions of Iran (5, 6). Recent global studies estimate that approximately 14% of pregnancies worldwide are affected by GDM, with increasing rates attributed to rising obesity and advancing maternal age. In developing countries, including Iran, rapid lifestyle changes, such as reduced physical activity and increased consumption of processed foods, have contributed to this upward trend (7).
The American Diabetes Association recommends fasting blood glucose testing for all pregnant women during their first prenatal visit (1, 5). The GDM is associated with various maternal and fetal complications. Maternal complications include preterm birth, infectious complications, polyhydramnios, and high blood pressure. Fetal complications involve intrauterine fetal death, congenital malformations, impaired fetal growth, macrosomia, intrauterine growth restriction, and respiratory distress syndrome, which may lead to early infant mortality (1). Although most mothers with GDM return to normal blood glucose levels shortly after delivery, they face an increased risk of recurrent GDM in subsequent pregnancies and are at higher risk of developing glucose intolerance and, eventually, type 2 diabetes in the future (7).
Pregnant women with GDM who are overweight or obese require special care and management to improve their own health and that of their fetus and to reduce the risk of complications during labor and for the fetus (1). The common treatment for GDM involves lifestyle interventions, with insulin prescribed if lifestyle changes prove ineffective (8). Lifestyle changes necessitate education and counseling, as patients often lack sufficient information about controlling blood glucose levels, as well as their nutritional and exercise needs. Therefore, healthcare providers and physicians should focus on enhancing self-care behaviors (9, 10).
Given the pivotal role of mothers in ensuring both maternal and fetal health and the paramount importance of self-care in women's overall well-being, mastering self-care techniques to manage common reproductive challenges is essential. This approach not only promotes women's health but also improves the health of families and society at large (11). Self-care is a key concept in promoting health (8) and serves as the first step in helping patients better manage their conditions (12). The primary goals of self-care in pregnant women at risk for diabetes are to maintain blood glucose levels within the normal range and reduce complications of the disease. These goals can be achieved through timely insulin administration, a healthy diet, regular exercise, recognizing symptoms of high blood glucose, adherence to prescribed medications, and lifestyle improvement (12, 13). Among these measures, physical activity is a top priority in self-care and lifestyle changes, as it can contribute to long-term weight loss (14).
Various studies have investigated the impact of education and counseling on successful self-care (14, 15). Education has proven to be an effective method for mitigating the adverse effects of stress on the behavior of patients with diabetes (16). A review study by Xie et al. examined the role of telemedicine in managing gestational diabetes and found that telemedicine, with its potential to reduce costs and improve access to modern medical care, plays a significant role in prenatal care and reducing complications of gestational diabetes (17). Similarly, another study concluded that telemedicine interventions could more effectively lower glycemic levels in patients with GDM and reduce the risk of maternal and neonatal/foetal complications (18). Despite the advantages of face-to-face training courses, such as personalized interaction, these methods face significant limitations, including time and location constraints for both trainers and patients. Recent advances in information and communication technology have led to the emergence of virtual platforms, including multimedia-based applications. Online education now enables the delivery of audio, visual, and concise educational content at any time, providing flexibility and accessibility.
Given the rising prevalence of GDM and the critical role of self-care in its management, innovative educational approaches are essential to optimize patient outcomes (19). However, despite the increasing integration of online education tools in healthcare, there is a lack of comprehensive evidence regarding the efficacy of WhatsApp-based interventions in promoting self-care behaviors and lifestyle modifications among overweight and obese pregnant women with GDM. While various studies have explored telemedicine applications and digital platforms for managing diabetes, most research has focused on general populations or other chronic conditions, with limited attention given to pregnant women, particularly those with GDM.
Moreover, although face-to-face education is a well-established method for managing GDM and improving outcomes such as blood glucose control, physical activity, and overall lifestyle, the comparative effectiveness of WhatsApp-based education remains underexplored. Few studies have examined whether WhatsApp can achieve similar or superior results in glycemic control, adherence to self-care practices, and lifestyle changes among high-risk pregnant women. Without sufficient evidence, the utility of WhatsApp as a viable alternative to traditional education methods remains uncertain.
2. Objectives
This study aimed to compare the impact of face-to-face and WhatsApp-based educational interventions on self-care behaviors and lifestyle among overweight and obese pregnant women with diabetes.
3. Methods
This research was a clinical trial conducted on overweight and obese pregnant women with diabetes at health centers in Ahvaz during 2023, over a ten-week period. The inclusion criteria included pregnant women aged 24 - 28 weeks, diagnosed with gestational diabetes based on a two-hour postprandial blood glucose test. Participants were required to be literate, overweight or obese (as determined by BMI at the first care visit), own a personal smartphone with WhatsApp, and be able to attend and participate in face-to-face meetings.
Exclusion criteria included the occurrence of severe complications related to diabetes, failure to adhere to the study protocols, or voluntary withdrawal by the participant. To determine the sample size, a previous study (20) was referenced, with statistical parameters set at a power of 80% (β = 0.2) and a significance level of α = 0.05. The effect sizes were estimated with standard deviations (s1 = s2 = 1.26), and (d = 0.8), with a minimal clinically significant difference (d) of 0.8. The minimum sample size was calculated using the following formula:
The calculation resulted in a minimum sample size of (n = 78). To account for a potential dropout rate of 10%, the adjusted sample size was increased to 88 participants, with 44 assigned to the intervention group and 44 to the control group. Participants were selected using purposive sampling from all health centers in the east and west of Ahvaz, ensuring they met the inclusion criteria and did not meet any exclusion criteria.
This study recruited overweight and obese pregnant women with gestational diabetes from healthcare centers in Ahvaz, Iran. Potential participants who met the inclusion criteria were identified during their visits to the healthcare centers. The lead researcher provided a comprehensive explanation of the study procedures and ensured participants understood that their data would remain confidential. After obtaining written informed consent, participants were randomly assigned to one of two groups, each consisting of 44 individuals.
A block randomization method was employed to achieve balanced group sizes and minimize selection bias. Blocks of a predetermined size (8 participants per block) were created to facilitate an equal distribution of participants between the two groups. A random number generator was used to assign participants to either the control group, which received routine prenatal care, or the intervention group, which received both routine prenatal care and an educational program delivered via a mobile application. Each block was randomized independently to maintain the integrity of the random assignment throughout the recruitment process.
At baseline (between 24 and 28 weeks of gestation), a checklist of blood glucose tests (fasting blood sugar and 2-hour postprandial blood glucose) was completed for all participants. Blood glucose levels were measured and interpreted before and after the intervention based on the American Diabetes Association's criteria as of January 1, 2021. These criteria included fasting blood glucose levels of 92 mg/dL or higher, blood glucose levels of 180 mg/dL or higher one hour after consuming 75 grams of glucose, and blood glucose levels of 153 mg/dL or higher two hours after an oral glucose tolerance test (OGTT) with 75 grams of glucose (21). Additionally, demographic data and questionnaires assessing physical activity, lifestyle, and self-care behaviors were collected.
Subsequently, women in both groups received routine care provided by the health centers until delivery. In addition to the face-to-face education offered by the health center's midwife as part of routine prenatal care, the intervention group received additional education via a software application. A WhatsApp group was created for the intervention group, where participants received two educational messages daily (on even-numbered days) over a 10-week period. These messages included text, images, and videos, with content aligned with the in-person educational sessions. Both the in-person and online education covered topics such as gestational diabetes, its complications, self-care strategies, nutrition (including dietary restrictions and portion sizes), physical activity, and insulin administration. Recommended exercises included walking, rhythmic movements, stretching, Pilates, and prenatal classes.
To monitor the effectiveness of the educational intervention, participants were contacted by telephone throughout the study and informed that they could reach out to the researcher for additional support. At 38 weeks of gestation, all participants underwent an OGTT and FBS test. The results were recorded, and participants completed follow-up questionnaires on physical activity, lifestyle, and self-care behaviors. Weight changes were also assessed.
Data were collected using a demographic questionnaire, a blood glucose test checklist, maternal weight measurements, and weight change recordings, along with the International Physical Activity Questionnaire (short form), a lifestyle questionnaire, and the Diabetes Self-Care Activities Scale. The demographic questionnaire consisted of two sections: Sociodemographic characteristics (e.g., age, education, occupation) and obstetric history (e.g., number of pregnancies, gestational age, miscarriages).
The Diabetes Self-Care Activities Scale, developed by Toobert et al., was used to assess self-care behaviors in individuals with diabetes. This 15-item scale evaluates self-care behaviors across four domains (diet, exercise, blood glucose monitoring, and insulin injection) in its original version, and five domains (diet, exercise, blood glucose monitoring, foot care, and smoking) in a later version. The scale employs a 7-point Likert scale, ranging from 0 (no self-care activities in the past seven days) to 7 (performed all self-care activities in the past seven days). For instance, smoking is scored as 0 if the participant smoked and 7 if they did not. The maximum possible score is 78, with higher scores reflecting better self-care (22). The Bahasa Indonesia version of the Summary of Diabetes Self-Care Activities (SDSCA) demonstrated excellent content validity (CVI = 0.98) and acceptable reliability (Cronbach's alpha = 0.72) (23). Nouhi et al. adapted and validated this scale in Iran, showing good content validity and reliability (Cronbach's alpha = 0.89) (24).
The International Physical Activity Questionnaire (IPAQ) is a globally recognized instrument for assessing physical activity levels. It includes questions about an individual's work-related physical activity, transportation, housework, and leisure activities over the previous seven days. Developed in 1998 by the World Health Organization and the Centers for Disease Control and Prevention for individuals aged 15 - 69, the IPAQ utilizes a 27-item self-report format with four sections: Job-related activity (7 items), transportation (6 items), leisure-time activities (6 items), and time spent sitting (8 items). It assesses light, moderate, and vigorous physical activity levels and walking over the past week. A scoring protocol converts this information into MET-minutes/week, a unit used to estimate energy expenditure during physical activity. One MET corresponds roughly to the energy expenditure of a person at rest. The short form of this questionnaire was used in the present study.
In this study, physical activity levels were categorized as follows:
- Intense physical activity: Engaging in any combination of light, moderate, or walking activities for at least seven days a week, totaling a minimum of 3000 MET-minutes per week.
- Moderate physical activity: A combination of walking, moderate, or light activities for at least five days a week, amounting to at least 600 MET-minutes per week.
- Light physical activity: Reporting no physical activity or engaging in activities that did not meet the criteria for moderate or vigorous activity (25).
The IPAQ has been widely validated across various populations, demonstrating good test-retest reliability [(rw = 0.74)] and moderate concurrent validity [(rw = 0.72)] (26). The validity of the questionnaire was further confirmed by Vaghani-Farahani, who reported a reliability coefficient of 0.83 (27).
The lifestyle questionnaire used in this study comprised 70 items designed to assess various lifestyle dimensions, including physical health, exercise and fitness, weight control and nutrition, disease prevention, mental health, spiritual health, social health, medication and substance abuse avoidance, accident prevention, and environmental health. It utilized a Likert scale response format across ten dimensions. To calculate a score for each dimension, the corresponding question scores were summed, and the overall questionnaire score was derived by summing the scores from all questions. The possible scores ranged from 42 (lowest) to 211 (highest). Based on this scoring system, three lifestyle levels were designated: Unfavorable (48 - 98), moderate (99 - 155), and favorable (156 - 211).
The study by Eshaghi et al. demonstrated the questionnaire's reliability (Cronbach’s alpha = 0.76) and its effectiveness for assessing healthy lifestyle patterns among the Iranian elderly (28). Additionally, Lali et al. validated the construct validity of the lifestyle questionnaire as a multidimensional tool for assessing lifestyle using factor analysis. The questionnaire's reliability was further confirmed with a Cronbach's alpha coefficient of 0.78 (29).
Following the completion of the initial questionnaires, a needs assessment was conducted. Educational content and a training package, including videos, photos, and texts, were developed and tailored based on the identified needs. Data analysis for the study was performed using SPSS version 22. A chi-squared test was utilized to assess the homogeneity of the two groups concerning categorical demographic variables. Before conducting parametric tests, the assumption of normality was verified using the Kolmogorov-Smirnov test, and the assumption of homogeneity of variances was examined using Levene's test. After confirming these assumptions, an independent samples t-test was conducted to examine between-group differences, while a paired samples t-test was used to investigate within-group differences at pre- and post-intervention stages. The significance level was set at 0.05.
4. Results
The Kolmogorov-Smirnov test was initially conducted to assess the normality of the data. Descriptive statistics (mean ± standard deviation) were used to summarize baseline characteristics and outcome variables. For between-group comparisons of normally distributed data, independent t-tests were employed, while paired t-tests were used for within-group comparisons (pre- and post-intervention). For non-normally distributed variables, non-parametric tests, such as the Mann-Whitney U test, were applied.
To account for potential confounders, such as age, BMI, and baseline differences in physical activity and self-care behaviors, analysis of covariance (ANCOVA) was performed when comparing post-intervention outcomes between the control and intervention groups. This adjustment allowed for the isolation of the effect of the educational intervention on outcomes such as blood glucose levels, physical activity, and self-care practices while controlling for these potential confounders.
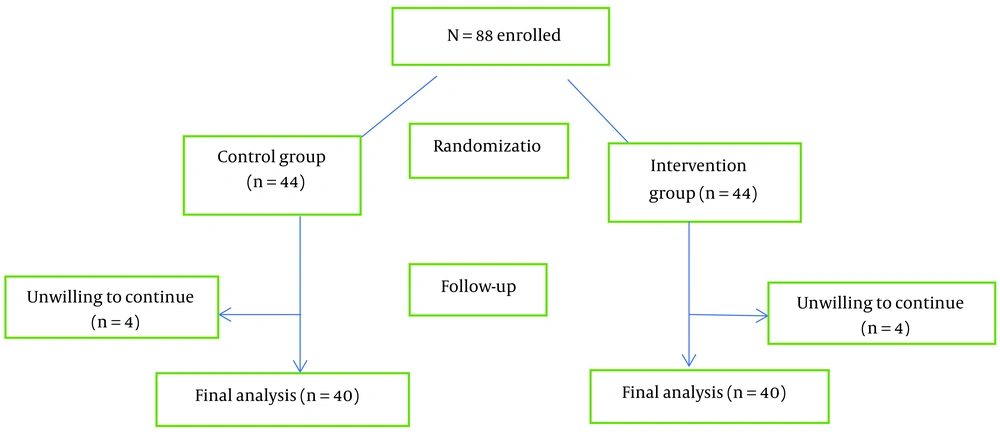
In this clinical trial conducted on 88 overweight and obese pregnant women with diabetes, 88 participants were initially enrolled. However, during the sampling process, 8 individuals—4 from the intervention group and 4 from the control group—withdrew due to their unwillingness to continue (Figure 1). The mean ± standard deviation of the pregnant women's age was 30.58 ± 6.44 years in the intervention group and 31.88 ± 5.15 years in the control group. There was no significant difference in the distribution of demographic information between the intervention and control groups (P > 0.05) (Table 1).
| Variables | Intervention Group (n = 40) | Control Group (n = 40) | P-Value |
|---|---|---|---|
| Age (y) | 30.58 ± 6.44 | 31.88 ± 5.15 | 0.322 |
| Age at childbirth (y) | 26.85 ± 1.15 | 26.48 ± 1.45 | 0.213 |
| Number of miscarriages | 0.25 ± 0.05 | 0.38 ± 0.54 | 0.305 |
| Number of children | 1.08 ± 0.91 | 1.15 ± 0.94 | 0.72 |
| Number of deliveries | 1.13 ± 0.99 | 1.23 ± 1 | 0.655 |
| Number of pregnancies | 2.35 ± 1.16 | 2.06 ± 1.21 | 0.351 |
| Education | 0.917 | ||
| Below diploma | 9 (22.5) | 8 (22.0) | |
| Diploma | 15 (37.5) | 15 (37.5) | |
| Associate's degree | 5 (12.5) | 3 (7.5) | |
| Bachelor's degree | 10 (25.0) | 13 (32.5) | |
| Master's degree | 1 (2.5) | 1 (2.5) | |
| Socioeconomic status | 0.874 | ||
| Low | 4 (10.0) | 5 (12.5) | |
| Medium | 31 (77.5) | 29 (72.5) | |
| High | 5 (12.5) | 6 (15.0) | |
| Occupation | 0.532 | ||
| Housewife | 32 (80.0) | 30 (75.0) | |
| Employed | 2 (5.0) | 1 (2.5) | |
| Self-employed | 1 (2.5) | 4 (10.0) | |
| Other | 5 (12.5) | 5 (12.5) |
a Values are expressed as mean ± SD or No. (%).
The mean ± standard deviation of one-hour postprandial blood glucose levels was significantly different between the control group (163.55 ± 27.07 mg/dL) and the intervention group (119.32 ± 16.54 mg/dL) (P = 0.007). Similarly, two-hour postprandial blood glucose levels were significantly lower in the intervention group (106.25 ± 25.16 mg/dL) compared to the control group (147.77 ± 24.73 mg/dL) after the intervention (P = 0.0028). Additionally, there was a significant difference in mean weight between the two groups following the intervention, with the intervention group at 82.27 ± 1.88 kg and the control group at 87.07 ± 10.82 kg (P = 0.028) (Table 2).
| Variables | Control Group (n = 40) | Intervention Group (n = 40) | P-Value |
|---|---|---|---|
| Before intervention | |||
| Fasting blood glucose | 117.3 ± 30.35 | 92.82 ± 17.83 | 0.347 |
| One-hour postprandial glucose | 166.67 ± 52/47 | 130.02 ± 17.93 | 0.819 |
| Two-hour postprandial glucose | 146.11 ± 42.47 | 115.32 ± 20.25 | 0.830 |
| Weight | 75.81 ± 11.98 | 75.72 ± 8.96 | 0.975 |
| After intervention | |||
| Fasting blood glucose | 112.12 ± 17.64 | 91.72 ± 16.16 | 0.733 |
| One-hour postprandial glucose | 163.55 ± 27.07 | 119.32 ± 16.54 | 0.007 |
| Two-hour postprandial glucose | 147.77 ± 24.73 | 106.25 ± 15.65 | 0.028 |
| Weight | 87.07 ± 10.82 | 82.27 ± 8.18 | 0.028 |
a Values are expressed as mean ± SD.
The mean scores for total lifestyle (P = 0.011), physical health (P = 0.001), exercise and fitness (P = 0.001), weight control and nutrition (P = 0.001), spiritual health (P = 0.006), disease prevention (P = 0.042), social health (P = 0.020), and avoidance of drugs and narcotics (P = 0.041) showed significant improvements within the intervention group before and after the intervention. Furthermore, significant differences were observed between the control and intervention groups after the intervention in the mean scores for total lifestyle (P = 0.029), physical health (P = 0.047), exercise and fitness (P = 0.001), weight control and nutrition (P = 0.001), and disease prevention (P = 0.042) (Table 3).
| Variables | Control Group (n = 40) | Intervention Group (n = 40) | P-Value |
|---|---|---|---|
| Physical health | |||
| Before intervention | 14.67 ± 3.22 | 13.75 ± 3.58 | 0.229 |
| After intervention | 15.15 ± 3.28 | 16.25 ± 2.61 | 0.042 |
| P-value | 0.445 | 0.001 | - |
| Exercise and wellness | |||
| Before intervention | 8.61 ± 3.27 | 7.27 ± 3.62 | 0.09 |
| After intervention | 8.81 ± 3.29 | 12.35 ± 3.66 | 0.001 |
| P-value | 0.764 | 0.001 | - |
| Weight control and nutrition | |||
| Before intervention | 12.41 ± 3.51 | 10.92 ± 3.54 | 0.065 |
| After intervention | 12.85 ± 4.02 | 15.15 ± 3.4 | 0.006 |
| P-value | 0.394 | 0.001 | - |
| Disease prevention | |||
| Before intervention | 16.97 ± 2.63 | 16.71 ± 2.53 | 0.636 |
| After intervention | 16.42 ± 2.78 | 18.01 ± 2.73 | 0.013 |
| P-value | 0.342 | 0.042 | - |
| Mental health | |||
| Before intervention | 14.35 ± 4.22 | 14.01 ± 4.4 | 0.797 |
| After intervention | 14.65 ± 4.35 | 14.77 ± 4.09 | 0.894 |
| P-value | 0.691 | 0.372 | - |
| Spiritual health | |||
| Before intervention | 14.57 ± 2.68 | 13.82 ± 2.86 | 0.053 |
| After intervention | 14.91 ± 3.66 | 14.82 ± 2.86 | 0.241 |
| P-value | 0.30 | 0.006 | - |
| Social health | |||
| Before intervention | 14.42 ± 3.35 | 13.8 ± 4.24 | 0.467 |
| After intervention | 14.21 ± 3.92 | 15.52 ± 3.63 | 0.121 |
| P-value | 0.691 | 0.02 | - |
| Avoidance of drugs and substances | |||
| Before intervention | 15.12 ± 4.7 | 14.87 ± 4.31 | 0.805 |
| After intervention | 15.5 ± 3.55 | 13.81 ± 3.29 | 0.093 |
| P-value | 0.561 | 0.041 | - |
| Accident prevention | |||
| Before intervention | 18.35 ± 3.87 | 17.22 ± 4.44 | 0.257 |
| After intervention | 17.17 ± 4.49 | 17.35 ± 3.73 | 0.85 |
| P-value | 0.095 | 0.893 | - |
| Environmental health | |||
| Before intervention | 13.47 ± 4.58 | 13.02 ± 4.78 | 0.636 |
| After intervention | 13.01 ± 4.51 | 12.97 ± 4.22 | 0.899 |
| P-value | 0.63 | 0.952 | - |
| Total score | |||
| Before intervention | 142.95 ± 19.93 | 134.51 ± 27.64 | 0.121 |
| After intervention | 141.85 ± 26.64 | 154.27 ± 23.24 | 0.029 |
| P-value | 0.759 | 0.001 | - |
a Values are expressed as mean ± SD.
The mean levels of moderate physical activity (P = 0.001) and sedentary physical activity (P = 0.001) differed significantly between the control and intervention groups after the intervention (P < 0.01). Additionally, significant differences were observed between the control and intervention groups in the mean levels of walking (P = 0.001), sedentary physical activity (P = 0.001), and total physical activity (P = 0.001) both before and after the intervention. Furthermore, the mean level of moderate physical activity in the control group showed a significant difference between the pre- and post-intervention stages (P = 0.001) (Table 4).
| Variables | Control Group (n = 40) | Intervention Group (n = 40) | P - Value |
|---|---|---|---|
| Intense physical activity | |||
| Before intervention | 302.75 (0 - 1200) | 298.25 (0 - 1200) | 0.945 |
| After intervention | 389.75 (1260 - 0) | 365.75 (0 - 940) | 0.731 |
| P-value | 0.252 | 0.236 | - |
| Moderate physical activity | |||
| Before intervention | 660.71 (900 - 120) | 448 (0 - 1100) | 0.717 |
| After intervention | 610 (990 - 400) | 439 (120 - 900) | 0.001 |
| P-value | 0.001 | 0.856 | - |
| Walking | |||
| Before intervention | 657.08 (1186 - 0) | 632.15 (180 - 1188) | 0.560 |
| After intervention | 915 (1584 - 445) | 856 (396 - 2772) | 0.659 |
| P-value | 0.001 | 0.001 | - |
| Sedentary activity | |||
| Before intervention | 160.35 | 135.5 | 0.171 |
| After intervention | 163.55 | 236.07 | 0.001 |
| P-value | 0.001 | 0.001 | - |
| Total Physical activity | |||
| Before intervention | 1839.91 | 2030.72 | 0.113 |
| After intervention | 1639. 18 | 1545 | 0.394 |
| P-value | 0.001 | 0.001 | - |
The results revealed significant differences in the mean total self-care score (P = 0.001), diet (P = 0.001), exercise (P = 0.039), blood glucose testing (P = 0.001), insulin injection (P = 0.018), and foot care (P = 0.083) within the intervention group before and after the intervention. Furthermore, the mean total self-care score (P = 0.001) and the subscales of diet (P = 0.003), exercise (P = 0.001), and insulin injection (P = 0.001) demonstrated significant differences between the control and intervention groups following the intervention (Table 5).
| Variables | Control Group (n = 40) | Intervention Group (n = 40) | P-Value |
|---|---|---|---|
| Diet plan | |||
| Before intervention | 16.5 ± 5.28 | 14.7 ± 4.45 | 0.471 |
| After intervention | 17.57 ± 5.29 | 20.87 ± 2.77 | 0.003 |
| P-value | 0.304 | 0.001 | - |
| Exercise | |||
| Before intervention | 4.17 ± 3.16 | 3.35 ± 3.15 | 0.247 |
| After intervention | 3.67 ± 3.48 | 7.02 ± 2.63 | 0.001 |
| P-value | 0.423 | 0.039 | - |
| Blood sugar test | |||
| Before intervention | 6.45 ± 4.73 | 5.23 ± 3.78 | 0.217 |
| After intervention | 6.22 ± 3.43 | 9.81 ± 2.99 | 0.001 |
| P-value | 0.698 | 0.001 | - |
| Insulin injection | |||
| Before intervention | 3.71 ± 2.75 | 2.66 ± 2.51 | 0.067 |
| After intervention | 3.11 ± 2.07 | 4.92 ± 2.16 | 0.001 |
| P-value | 0.533 | 0.001 | - |
| Foot care | |||
| Before intervention | 13.95 ± 7.22 | 12.21 ± 5.22 | 0.093 |
| After intervention | 11.97 ± 8.52 | 13.25 ± 6.89 | 0.467 |
| P-value | 0.083 | 0.018 | - |
| Overall score | |||
| Before intervention | 44.67 ± 15.1 | 43.11±11.14 | 0.103 |
| After intervention | 42.65 ± 17.58 | 56.02 ± 11.63 | 0.001 |
| P-value | 0.388 | 0.001 | - |
a Values are expressed as mean ± SD.
5. Discussion
This study aimed to evaluate the impact of self-care education delivered via WhatsApp on self-care behaviors among overweight and obese pregnant women with diabetes. The findings indicated no significant difference in the overall mean self-care scores between the control and intervention groups prior to the intervention. However, after the intervention, a significant improvement in self-care behaviors was observed in the intervention group compared to the control group. Similarly, Hosseinzadeh et al. reported no significant differences in self-care scores among three groups before the intervention, but significant increases were noted in the face-to-face and Telegram-based education groups compared to the control group afterward (20).
Additionally, Bahremand et al. found that WhatsApp-based diabetes self-care education significantly improved overall self-care behaviors, including diet adherence, foot care, blood glucose control, and medication adherence in type 2 diabetes patients. Their conclusion that mobile-based self-care education via WhatsApp can enhance self-care behaviors and prevent adverse diabetes outcomes aligns with the results of the present study (30). These findings suggest that integrating social media into diabetes management could serve as a viable strategy to promote better health outcomes among high-risk populations.
The implementation of this program significantly heightened pregnant women's awareness of their health and that of their fetuses. The program's valuable content led to high levels of participant satisfaction and acceptance, consistent with the findings of Pirdel (31). This study also highlights the effectiveness of WhatsApp-based education in improving postprandial blood glucose levels among overweight and obese pregnant women with diabetes. While significant differences were observed in postprandial levels, fasting blood glucose showed no change, reflecting the results of Al Omar et al., which demonstrated that social media interventions positively affect glycemic control in diabetic patients (32).
The lack of significant differences in fasting glucose aligns with findings from Yang et al. (33) and Arani et al. (34), suggesting that mobile-based educational interventions may more effectively target specific aspects of glycemic control, such as postprandial levels. Collectively, these studies support the potential of digital health interventions to enhance self-care practices and glycemic outcomes, particularly in vulnerable populations like pregnant women.
The findings of this study underscore the effectiveness of WhatsApp-based self-care education in improving self-care behaviors and health outcomes among overweight and obese pregnant women with diabetes. These results align with previous research, such as that by Bahremand et al. (30), which demonstrated significant improvements in self-care behaviors among patients with type 2 diabetes who received education via WhatsApp. Additionally, the significant reductions in postprandial blood glucose levels observed in this study are consistent with findings by Al Omar et al. (32) and Yang et al. (33), who reported similar benefits of social media interventions on glycemic control.
Furthermore, the weight reduction achieved in this study supports the findings of Guo et al. (35), who noted that mobile health interventions positively influenced weight management in women with gestational diabetes. Collectively, these studies highlight the potential of digital platforms to enhance health education and self-management for individuals with diabetes, suggesting a promising avenue for future interventions in maternal and child health.
This study also revealed a significant difference in the mean overall lifestyle score between the control and intervention groups, both before and after the intervention. Interestingly, the mean lifestyle score was higher in the control group prior to the intervention. However, following the intervention, the mean lifestyle score was significantly higher in the intervention group, reflecting the positive impact of WhatsApp-based self-care education. Notably, the mean lifestyle score in the intervention group increased by approximately 10% post-intervention. These findings align with those of Bijani et al., who reported that a health education intervention significantly improved lifestyle scores among patients with hypertension (36).
Conversely, Khavoshi et al. (37) found that an educational intervention had no effect on the lifestyle and psychosocial health of the elderly, indicating that complex behaviors, such as smoking cessation, may be influenced by various social and personal factors. These studies emphasize the variability in intervention effectiveness based on demographic and contextual factors, suggesting that tailored approaches may be necessary to achieve optimal health outcomes across diverse populations.
The present study demonstrated a significant increase in moderate physical activity, walking, and sedentary behavior in the intervention group compared to the control group following the intervention. While the mean scores for vigorous physical activity decreased in both groups, the decline was less pronounced in the intervention group, indicating that these women gained a better understanding of the importance of physical activity during pregnancy and were more inclined to engage in light- to moderate-intensity activities.
The decrease in vigorous physical activity across both groups may be attributed to advancing gestational age, as pregnant women experience specific limitations due to fetal growth and weight gain during this stage. Supporting these findings, Szmeja et al. (38) did not report a significant difference in physical activity levels between the control and treatment groups of pregnant women who received remote education via DVDs during the third trimester. This suggests that while education can improve certain aspects of physical activity, the overall impact may be influenced by the physiological changes associated with pregnancy.
5.1. Strengths and Limitations
The most significant strength of this study was the use of WhatsApp as a virtual messaging platform for education. This approach offered several advantages:
- Accessibility and cost-effectiveness: Patients received necessary health advice promptly and without incurring additional costs, indirectly reducing the economic burden and improving accessibility.
- Enhanced engagement: The ability to share educational materials in various formats (videos, images, audio) via WhatsApp made the intervention more engaging and appealing compared to traditional SMS messaging.
- Social impact: Beyond individual knowledge enhancement, the sharing of diabetic education messages within social circles could potentially influence the lifestyle habits of others, promoting broader health behavior change.
However, this study has limitations that should be considered for a transparent interpretation of the findings.
Firstly, the inability to assess the long-term sustainability of the intervention’s effects represents a significant limitation, as the follow-up period was confined to the ten-week program. Consequently, it is unclear whether the observed improvements in self-care behaviors and glycemic control would persist beyond the intervention period.
Additionally, individual and sociocultural differences among participants may have influenced the study outcomes. Factors such as socioeconomic status, education level, and cultural beliefs could potentially affect adherence to self-care practices, introducing variability in the results and limiting the generalizability of the findings. While random selection was employed to mitigate bias, these inherent differences remain a concern.
Moreover, the reliance on self-reported data collection methods poses another limitation, as it may introduce social desirability bias, potentially skewing the reported outcomes.
Future research should prioritize several key areas informed by the findings and limitations of the current study. Longitudinal studies are critical to assessing the long-term sustainability of WhatsApp-based self-care education interventions, particularly in relation to maintaining self-care behaviors and glycemic control over time. Expanding research to include diverse populations will enhance the generalizability of the results, allowing for a broader understanding of the intervention's applicability across different demographic and cultural contexts.
The use of objective measurement techniques, such as continuous glucose monitoring, should be incorporated to improve data accuracy and reliability. Comparative studies evaluating the effectiveness of WhatsApp-based education against other digital platforms or traditional education methods can provide valuable insights into the most effective delivery modalities for such interventions.
Additionally, integrating behavioral strategies, such as motivational interviewing, into WhatsApp-based programs may enhance participant engagement and adherence to self-care practices. Exploring the impact of these educational interventions on broader health outcomes, including maternal mental health and neonatal health indicators, will offer a more comprehensive understanding of their overall effectiveness. By addressing these areas, future research can optimize digital health interventions and expand their utility in improving maternal and child health outcomes.
5.2. Conclusions
The findings of this study suggest that social media-based educational interventions, particularly those utilizing mobile applications like WhatsApp, can effectively influence the behaviors of pregnant women. By enhancing motivation to adopt healthier practices, these interventions can lead to significant improvements in maternal health outcomes. Therefore, it is recommended that healthcare providers integrate this educational approach into routine diabetes care for pregnant women, especially for those who face barriers to in-person sessions due to physical limitations, geographic distance, financial constraints, or other challenges.