1. Background
Patient safety, a global challenge in diagnosing and treating patients, is one of the healthcare system's priorities and a key element of medical service quality (1, 2). The right to be safe from risk and injury while receiving healthcare is one of the most prominent human rights and has become a fundamental requirement for hospital accreditation (3, 4). According to the World Health Organization (WHO) global patient safety action plan 2021 - 2030, patient safety is defined as "a framework of organized activities that create cultures, processes, procedures, behaviors, technologies, and environments in healthcare that continuously and sustainably reduce the risks and occurrence of avoidable injuries, reduce the likelihood of error, and reduce its impact if it occurs" (5, 6).
According to studies, it is estimated that approximately 400,000 patients die each year due to avoidable adverse events, and between two and four million cases have a serious impact on patient health (7). One in ten patients is injured in hospitals, and at least 50 percent of these injuries are preventable, according to the WHO (8). Every year, 2.6 million people die from unsafe care in hospitals in low- and middle-income countries (9). Approximately 42.7 million hospital admissions occur annually. In 2016, Johns Hopkins University reported that medical errors were the third highest cause of death in the United States, and unsafe care was responsible for 14% of permanent disability, 16% of average disability, and 30% of minimal disability (8). The safety culture in Asian countries, including Iran, differs from that in developed countries due to the lack of priority given to patient safety culture (4).
Patient safety culture includes "the values, beliefs, and norms of management and staff regarding the importance of patient safety in the healthcare organization, the expectations for appropriate and inappropriate behavior, and the rewards and punishments for processes and procedures" (10, 11). Optimizing patient safety culture should be a priority for clinical managers, as the role of culture in improving patient and healthcare worker safety is becoming increasingly important (7, 12). To change the culture, it is necessary to first understand it and then challenge it (3). Providing a culture of safety is the first and most important requirement of patient care, as it forms the foundation for other measures (13).
Measuring patient safety culture in hospitals is an important strategy for identifying key areas for continuous quality improvement. One of the benefits of measuring safety culture is that it provides a tangible indicator of the current situation and progress over time, serving as a basis for growth and improvement (4). The relationship between high levels of safety culture and reduced length of stay in hospital, readmissions, and medication errors has been confirmed (9). To strengthen patient safety, hospital managers need an annual assessment of patient safety culture to learn how to work with people more effectively and focus resources on improving system processes, work procedures, and professional practices (14). Hospital management, organizational learning, continuous improvement, and infection prevention are effective in understanding patient safety levels (15, 16), and management activities significantly influence employee compliance with hospital processes, particularly in teamwork and communication (3).
According to the WHO's global patient safety action plan, countries need to regularly survey safety culture in healthcare organizations and participate in international comparative studies. Health systems can observe the strengths and weaknesses related to safety culture and use the experiences of other countries to improve patient safety and reduce unwanted events (9).
2. Objectives
This study aimed to examine and compare the dimensions of patient safety culture in different departments of Imam Hossein Hospital before and after management measures based on hospital survey on patient safety culture (HSOPSC) indicators. The results of the study are expected to serve as a foundation for fundamental changes in the design, planning, and implementation of necessary measures to improve the quality of healthcare and promote patient safety and health.
3. Methods
3.1. Study Design
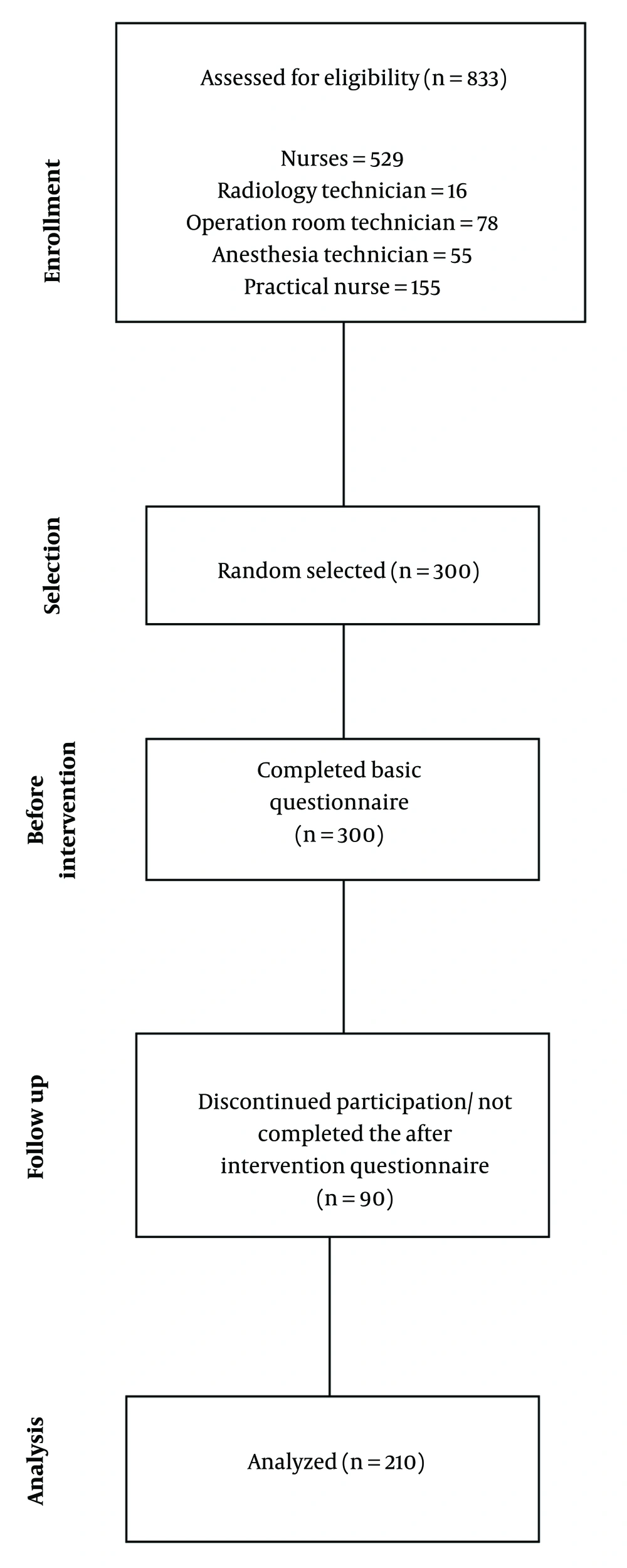
The present study was a semi-experimental study (with a before-and-after design) that examined safety culture indicators at Imam Hossein Hospital, an educational hospital in the east of Tehran province, from the perspective of hospital staff. Data were collected from late December 2023 to early January 2024, before and one year after interventional management actions (IMA). Inclusion criteria for the study were willingness to participate, being a nurse, operation room or radiology technician, practical nurse, or employee in the clinical and paraclinical departments of Imam Hossein Hospital. Participants who did not complete the questionnaire, declined to cooperate, or were unavailable for the second round of the survey were excluded from the study. Data from 90 questionnaires were excluded because they could not be retrieved.
Initially, a list of all healthcare workers, excluding physicians, such as nurses, operating room or radiology technicians, and practical nurses working in the clinical and paraclinical departments, was obtained from the hospital's personnel office. From this list, 300 staff members were randomly selected by assigning a unique code to each individual and using random number generation in Excel. After confirming their eligibility to participate, obtaining informed consent, and introducing the study to the participants, the data collection process began. The details of participant selection are described in Figure 1.
3.2. Ethical Considerations
This study is the result of a research project approved by Shahid Beheshti University of Medical Sciences (IR.SBMU.RETECH.REC.1402.422). Participation in the study was voluntary and required the informed written consent of the participants.
3.3. Data Collection Tools
The questionnaire collected demographic information, such as age, gender, education, service unit, hospital work history, work history in the current profession, hours worked per week, organizational position, patient interaction, and a question to determine the number of errors reported in the past 12 months. Information on patient safety culture was gathered using the HSOPSC assessment questionnaire. The HSOPSC questionnaire consists of 42 questions covering 12 different areas of safety culture, including: Frequency of events reported, overall patient safety perceptions, supervisor/manager expectations and actions promoting patient safety, organizational learning–continuous improvement, teamwork within units, communication openness, feedback and communication about errors, non-punitive response to errors, staffing, management support for patient safety, teamwork across units, and handoffs and transitions.
The response scale for the Likert-type questions consists of 5 items with a score ranging from one to five: Strongly disagree (1), disagree (2), no opinion/undecided (3), agree (4), and strongly agree (5) for questions with a positive concept, according to the questionnaire instructions. For questions with a negative concept, reverse scoring is used (17).
Additionally, the method proposed by the HSOPSC questionnaire designers was applied to compare the results with those of other studies. For questions with negative connotations, "Strongly Disagree" and "Disagree" were considered negative responses, while "Strongly Agree" and "Agree" were considered positive responses. The average percentage of positive responses was calculated by summing the positive scores within the range (17, 18). It is important to note that this questionnaire was used and validated in a master's project to evaluate the culture of patient safety in Iranian educational hospitals (19). The validity of this questionnaire was confirmed, and its reliability was reported to be 82% (Cronbach's alpha = 0.82) (19).
3.4. Interventional Management Actions
Interventional management actions in this study included training on safety guidelines through in-person retraining courses and electronic webinars, encouraging high reporters, and disseminating lessons learned from errors to hospital departments and units. The educational intervention of the management system, which lasted for four months (from February to May 2023), was conducted as follows:
- Face-to-face training: Held weekly, these in-person classes were led by the head nurse, educational and clinical supervisors, and the patient safety coordinator in each department. Each session lasted one hour and was organized as structured group classes.
- Safety protocol education: Implemented through in-person retraining courses and webinars, a total of six training sessions were conducted over these four months, all accredited for continuing education.
- Staff incentives: Personnel who reported the highest number of events (errors) were recognized with certificates of appreciation and increased performance bonuses, fostering a non-punitive approach to error reporting.
- Root cause analysis (RCA) meetings: A total of 11 RCA sessions were held within the specified four-month period. These meetings involved individuals relevant to the reported errors, with the outcomes communicated to the treatment team across all groups while maintaining confidentiality. Additionally, lessons learned from these errors were documented, and learning letters were disseminated and shared among various treatment teams within the hospital.
3.5. Data Gathering Method
Information on patient safety culture and error reporting rates in the previous 12 months was collected both before and one year after the IMA. Each participant was assigned a unique code, and baseline information and safety culture data were collected one week before the start of the intervention. Participants were surveyed again about the HSOPSC one year after the intervention. Both rounds used electronic questionnaires through the hospital information system (HIS). Additionally, to reduce participant drop-out, each participant was contacted via phone and email to invite them to participate in the study one year after the intervention actions, over the course of one week.
3.6. Sampling Method and Sample Size Estimation
Participants were randomly selected from the list of clinical and paraclinical staff based on the study entry criteria. Assuming an 8% change (effect size = 0.08) in the percentage of positive responses in the overall safety culture domain after the IMA compared to before, and considering a type I error of 5% and a power of 80%, the sample size was estimated to be approximately 300 people using G*Power software. After removing incomplete data, the analysis was performed with 210 samples.
3.7. Statistical Analysis
The normality distribution of the HSOPSC was assessed using a Q-Q plot. Continuous variables were reported as mean and standard deviation, while categorical variables were described as frequencies and percentages. Means were compared using one-way ANOVA or the Kruskal-Wallis test for more than two groups, and the Student's t-test or Mann-Whitney U test for comparisons between two groups. A paired t-test or Wilcoxon signed-rank test was used to assess changes in each factor after the IMA, based on the normality distribution of the data. All analyses were performed at a significance level of less than 0.05 using Stata version 14 software (StataCorp LLC, College Station, TX 77845, USA).
4. Results
A total of 210 out of the 300 distributed questionnaires were completed and returned in full (response rate = 70%). The majority of participants in this study were female (82.86%) and in the age range of 40 - 49 years (43.81%). Among the participants, 71.75% were nurses, 15.24% were operating room technicians, anesthesiologists, or radiologists, and 10.48% were nursing assistants or aides (practical nurses). Most participants reported working 40 - 59 hours per week. Other participant information is shown in Table 1.
| Variables | Values (n = 210) |
|---|---|
| Age (y) | |
| 20 - 29 | 35 (16.67) |
| 30 - 39 | 57 (27.14) |
| 40 - 49 | 92 (43.81) |
| ≥ 50 | 26 (12.38) |
| Gender | |
| Female | 174 (82.86) |
| Male | 36 (17.14) |
| Education level | |
| Diploma | 14 (6.67) |
| Bachelor’s degree | 164 (78.10) |
| Master’s degree | 25 (11.90) |
| PhD | 7 (3.33) |
| Job | |
| Nurse/supervisor | 159 (75.71) |
| Technician in operation room or radiology | 32 (15.24) |
| Practical nurse | 19 (9.05) |
| Work unit/ward | |
| ICU/CCU/NICU | 67 (31.90) |
| Other clinical unit | 121 (57.62) |
| Para clinic | 22 (10.48) |
| Working time in this hospital (y) | |
| < 1 | 20 (9.52) |
| 1 - 5 | 44 (20.95) |
| 6 - 10 | 12 (5.71) |
| 11 - 15 | 47 (22.38) |
| 16 - 20 | 51 (24.29) |
| > 20 | 36 (17.14) |
| Working time in current job (y) | |
| < 1 | 11 (5.24) |
| 1 - 5 | 40 (19.05) |
| 6 - 10 | 22 (10.48) |
| 11 - 15 | 43 (20.48) |
| 16 - 20 | 52 (24.76) |
| > 20 | 42 (20.00) |
| Working time in current unit/ward (y) | |
| < 1 | 28 (13.33) |
| 1 - 5 | 80 (38.10) |
| 6 - 10 | 39 (18.57) |
| 11 - 15 | 26 (12.38) |
| 16 - 20 | 28 (13.33) |
| > 20 | 9 (4.29) |
| Working hours per week (h) | |
| 20 - 39 | 36 (17.14) |
| 40 - 59 | 125 (59.52) |
| 60 - 79 | 33 (15.71) |
| 80 - 99 | 7 (3.33) |
| ≥ 100 | 9 (4.29) |
| Direct interaction/contact with patients | |
| Yes | 202 (96.19) |
| No | 8 (3.81) |
a Values are expressed as No. (%).
In response to the question about the number of error reports in the past 12 months, as shown in Table 2, approximately half of the study participants (49.05%) did not report any events (errors or incidents) in the 12 months prior to the interventional management action (IMA). However, after one year of IMA implementation, it was observed that the frequency of event reporting among these participants had changed significantly. Conversely, the frequency of patient safety events reported increased from 50.95% to 61.90% after the IMA (P-value = 0.048). This resulted in a decrease in the distribution of non-reporting to 38.10% and, consequently, an improvement in the distribution of reporting.
| Reported Patient Safety Events (Number) | Before IMA | After IMA | Paired Comparison P-Value |
|---|---|---|---|
| 0 | 103 (49.05) | 80 (38.10) | 0.048 b |
| 1 - 2 | 59 (28.10) | 67 (31.90) | |
| 3 - 5 | 20 (9.52) | 26 (12.38) | |
| 6 - 20 | 24 (11.43) | 36 (17.14) | |
| ≥ 21 | 4 (1.90) | 1 (0.48) |
Abbreviation: IMA, interventional management actions.
a Values are expressed as No. (%).
b P-value < 0.05.
According to Table 3, the mean HSOPSC scores before and after the IMA were 121.37 ± 18.77 and 134.53 ± 16.35, respectively. This observed improvement after the implementation of management interventions was statistically significant (P-value < 0.001). Significant changes in HSOPSC scores after one year of management intervention were observed in all dimensions except overall patient safety perception and supervisor/manager expectations (P-value < 0.05).
| HSOPSC Dimensions | Before | After | Mean Difference b | Pairwise Comparison P-Value | ||
|---|---|---|---|---|---|---|
| Mean ± SD | Positive Response a (%) | Mean ± SD | Positive Response a (%) | |||
| Frequency of events reported | 9.99 ± 1.57 | 60.47 | 9.20 ± 1.48 | 30.10 | -0.78 ± 2.29 | < 0.001 c |
| Overall patient-safety perceptions | 12.74 ± 2.89 | 53.20 | 12.51 ± 2.89 | 50.47 | -0.22 ± 4.19 | 0.430 |
| Supervisor/manager expectations and actions promoting patient safety | 12.19 ± 3.80 | 46.52 | 12.37 ± 3.98 | 49.40 | 0.17 ± 5.57 | 0.647 |
| Organizational learning-continuous improvement | 10.10 ± 2.25 | 59.52 | 11.88 ± 1.45 | 87.14 | 1.77 ± 2.65 | < 0.001 c |
| Teamwork within units | 12.04 ± 3.21 | 45.95 | 15.85 ± 1.87 | 86.42 | 3.80 ± 3.65 | < 0.001 c |
| Communication openness | 7.86 ± 2.54 | 28.40 | 11.35 ± 1.59 | 75.07 | 3.49 ± 3.13 | < 0.001 c |
| Feedback and communication about error | 9.19 ± 2.15 | 39.36 | 10.12 ± 2.40 | 50.95 | 0.93 ± 3.04 | < 0.001 c |
| Non-punitive response to errors | 9.11 ± 2.23 | 41.58 | 8.34 ± 1.46 | 35.07 | -0.77 ± 2.68 | < 0.001 c |
| Staffing | 7.91 ± 2.58 | 15.83 | 8.53 ± 2.00 | 17.13 | 0.61 ± 3.24 | 0.006 c |
| Management support for patient safety | 8.11 ± 2.59 | 29.76 | 8.81 ± 3.02 | 40.79 | 0.69 ± 3.92 | 0.010 c |
| Teamwork across units | 8.21 ± 2.41 | 36.18 | 9.28 ± 2.57 | 47.61 | 1.06 ± 3.43 | < 0.001 c |
| Handoffs and transitions | 13.85 ± 3.36 | 36.56 | 16.24 ± 3.66 | 51.90 | 2.38 ± 4.90 | < 0.001 c |
| Total | 121.37 ± 18.77 | 41.07 | 134.53 ± 16.35 | 51.83 | 13.16 ± 24.90 | < 0.001 c |
Abbreviation: HSOPSC, hospital survey on patient safety culture.
a Averaging the item-level percent positive scores.
b Mean difference = after value - before value.
c P-value < 0.05.
Although the mean HSOPSC score changes in the areas of frequency of events reported (mean difference = -0.78 ± 2.29) and non-punitive response to errors (mean difference = -0.77 ± 2.68) decreased compared to before the interventions (P-value < 0.001), the total percentage of positive safety culture scores before the IMA was 41.07%, which improved to 51.83% after the IMA. The findings indicate that, from the participants' perspective, before the management interventions, the strongest aspect of the hospital's safety culture was the frequency of events reported, with the highest percentage of positive scores (60.47%), while the weakest aspect was staffing (15.83%). After one year of implementing the IMA, the strongest aspect became organizational learning-continuous improvement, with the highest percentage of positive scores (87.14%), and the weakest aspect remained staffing, with the lowest percentage of positive scores (17.13%).
Table 3 shows the mean HSOPSC scores and their changes, along with the percentage of positive scores for each dimension.
Table 4 presents the results of comparing the mean changes in the HSOPSC score (before and after the IMA) based on the characteristics of the participants. In general, an improvement in the safety culture score of the participants was observed in most cases after the IMA (P-value < 0.05). This difference was statistically significant between the subgroups studied, differentiated by gender and department type. Specifically, the mean difference was greater in men (17.36 ± 31.07) compared to women (12.29 ± 23.44), and this difference was statistically significant between the two groups (P-value = 0.025). Additionally, the improvement in scores observed in different hospital units varied. In ICU/CCU/NICU (P-value = 0.0007) and other clinical units (P-value = 0.0005), a greater improvement in safety culture scores was observed after the IMA compared to paraclinical units.
| Variables | Before | After | Mean Difference | Pairwise Comparison P-Value |
|---|---|---|---|---|
| Age (y) | ||||
| 20 - 29 | 117.4 ± 20.55 | 131.25 ± 16.24 | 13.85 ± 28.47 | 0.007 c |
| 30 - 39 | 117.82 ± 17.24 | 135.84 ± 15.28 | 18.01 ± 22.76 | < 0.001 c |
| 40 - 49 | 120.84 ± 15.85 | 135.13 ± 15.56 | 14.28 ± 20.17 | < 0.001 c |
| 50 ≤ | 136.34 ± 22.54 | 133.96 ± 21.06 | -2.38 ± 33.62 | 0.720 |
| Gender | ||||
| Female | 121.89 ± 18.36 | 134.18 ± 16.55 | 12.29 ± 23.44 | < 0.001 c |
| Male | 118.83 ± 20.83 | 136.19 ± 15.44 | 17.36 ± 31.07 | 0.002 c |
| Education level | ||||
| Diploma | 126.14 ± 25.59 | 132.07 ± 16.90 | 5.92 ± 38.19 | 0.571 |
| Bachelor’s degree | 121.29 ± 18.20 | 134.84 ± 16.62 | 13.55 ± 23.65 | < 0.001 c |
| Master’s degree | 119.44 ± 15.35 | 134.12 ± 14.85 | 14.68 ± 20.71 | 0.001 c |
| PhD | 120.57 ± 29.17 | 133.57 ± 17.04 | 13.00 ± 37.31 | 0.392 |
| Job | ||||
| Nurse/supervisor | 121.34 ± 18.76 | 135.03 ± 17.13 | 13.69 ± 24.14 | < 0.001 c |
| Technician in operation room or radiology | 122.65 ± 13.33 | 132.75 ± 14.10 | 10.09 ± 20.53 | 0.009 c |
| Practical nurse | 119.42 ± 26.26 | 133.31 ± 13.30 | 13.89 ± 36.63 | 0.115 |
| Work unit/ward | ||||
| ICU/CCU/NICU | 117.76 ± 16.85 | 135.53 ± 16.87 | 17.77 ± 23.62 | < 0.001 c |
| Other clinical unit | 119.76 ± 17.75 | 134.33 ± 15.78 | 14.57 ± 22.92 | < 0.001 c |
| Paraclinic | 141.22 ± 18.63 | 132.54 ± 18.31 | -8.68 ± 28.93 | 0.174 |
| Working time in current job (y) | ||||
| < 1 | 124.63 ± 14.49 | 135.18 ± 19.99 | 10.54 ± 19.01 | 0.095 |
| 1 - 5 | 118.10 ± 23.30 | 133.82 ± 15.31 | 15.72 ± 31.31 | 0.003 c |
| 6 - 10 | 119.00 ± 14.04 | 131.13 ± 16.08 | 12.13 ± 19.26 | 0.007 c |
| 11 - 15 | 120.00 ± 15.85 | 135.93 ± 17.11 | 15.93 ± 22.77 | < 0.001 c |
| 16 - 20 | 120.32 ± 14.97 | 135.80 ± 14.85 | 15.48 ± 19.58 | < 0.001 c |
| > 20 | 127.57 ± 23.09 | 133.80 ± 18.00 | 6.23 ± 29.50 | 0.178 |
| Working hours per week (h) | ||||
| 20 - 39 | 123.77 ± 12.06 | 136.47 ± 16.31 | 12.69 ± 21.67 | 0.001 c |
| 40 - 59 | 122.90 ± 19.25 | 133.76 ± 16.37 | 10.85 ± 25.26 | < 0.001 c |
| 60 - 79 | 121.78 ± 19.69 | 136.36 ± 16.70 | 14.57 ± 24.44 | 0.001 c |
| 80 - 99 | 98.57 ± 18.53 | 134.71 ± 19.01 | 36.14 ± 24.09 | 0.007 c |
| 100 ≤ | 106.66 ± 16.14 | 130.66 ± 14.98 | 24.00 ± 27.33 | 0.030 c |
Abbreviation: HSOPSC, hospital survey on patient safety culture.
a Values are expressed as mean ± SD.
b Mean difference = after value – before value.
c P-value < 0.05.
5. Discussion
Patient safety is a global issue, and one way to gain insight into it is by using safety culture assessment tools. One of the benefits of measurement is that it provides tangible indicators of the current situation and helps improve the hospital and medical staff over time (20, 21). The aim of the present study was to assess the safety culture at Imam Hossein Hospital using the HSOPSC questionnaire, comparing staff responses before and after the IMA. Before intervening to change the hospital safety culture, it is necessary to assess the current state of safety culture. By evaluating the current state of patient safety culture, the hospital can identify its strengths and weaknesses. Developing a culture of safety can prevent adverse events or help correct errors quickly before patients are harmed.
According to the results of the present study, nearly half of the participants (49.05%) had not reported any errors or incidents in the past 12 months before the IMA. However, after one year of implementing the IMA, which included training on safety guidelines, encouraging personnel with the highest reporting statistics, and disseminating lessons learned from errors to hospital departments and units, it was observed that the frequency of reported events among these participants showed significant improvement. This is consistent with the study by Yilmaz and Goris (22), where the majority of nurses (88%) never documented a report. However, the prevalence of non-reporting in our study was lower. This difference, along with the excessively low error reporting in other studies, may indicate reluctance among staff to report errors. Reporting errors is a critical aspect of achieving patient safety, and one possible reason for non-reporting may be the punitive culture in hospitals and fear of the consequences of reporting errors. However, the present study found a positive outcome after the IMA, which suggests a shift in this culture.
In our study, the mean score of the HSOPSC improved in most dimensions, except for the dimensions of overall patient safety perceptions and supervisor/manager expectations and actions promoting patient safety. The frequency of events reported was the strongest dimension of safety culture before the IMA and staff training in hospitals, which is consistent with the results of other studies (7, 23, 24), but inconsistent with the findings of Filiz and Yesildal (9) and Tereanu et al. (25). According to the results of our study, "Organizational learning-continuous improvement" also received the highest positive score after the IMA, which aligns with the results of other studies (3, 15, 26-28). The optimal status of this dimension can indicate the presence of approaches aimed at promoting and improving patient safety, as well as the consideration of clinical risks, attention to work performance, and open training courses for staff.
"Staffing", as one of the dimensions of patient safety culture, reflects issues related to hospital staff that affect patient safety. According to the results of the present study, it had the least positive result both before and after the IMA. This may be attributed to differences in human personality, which is consistent with the findings of Ahmed et al. (29) and Abdulla et al. (20), but inconsistent with the results of other studies (30). In fact, one of the employee-related issues addressed in the current study that received the lowest positive score was the systematic assessment of key outcome indicators and the evaluation of employee perceptions and attitudes toward patient safety. This is crucial for helping healthcare organizations identify priority areas for improving healthcare safety and quality.
Ultimately, the results of the study by Lassoued et al. (31), conducted in 2024 at one of the teaching hospitals in Tunisia, showed that after implementing educational interventions at the hospital staff level, the frequency of reported adverse events increased from 30% to 65%, and various aspects of patient safety culture improved. Specifically, after the intervention, “teamwork across units” received the highest positive responses, while management support for patient safety showed the greatest positive changes. Therefore, based on the existing evidence and the results of our study, we can conclude that educational interventions, such as organizing workshops or self-learning programs for staff, can be effective in enhancing patient safety culture. However, the sustainability of this improvement relies on regular performance monitoring, coupled with encouragement, refresher training sessions, and the commitment of staff at all levels, which should be taken into consideration at the management level.
The findings of our study have several practical applications, including:
1. Improving patient safety culture: The insights gained can inform strategies to enhance patient safety culture within healthcare organizations.
2. Policy development: The results can assist policymakers in formulating guidelines and policies aimed at improving patient safety practices.
3. Training programs: The study may inform the development of targeted training programs for healthcare professionals to address identified weaknesses in patient safety culture.
4. Benchmarking: The findings can serve as a benchmark for future studies and help healthcare organizations assess their performance in relation to patient safety culture.
5.1. Limitations
The current study has several limitations that should be acknowledged. These include factors such as a limited sample size, the single-center nature of the study, the restricted setting related to nurses, potential biases such as response or interview bias, and the low generalizability of the findings.
To enhance the robustness of future research, it is suggested to design multicenter studies with larger sample sizes, conduct longitudinal studies to assess the long-term effects of interventions on HSOPSC scores, and compare HSOPSC scores across different healthcare settings or regions to identify best practices.
5.2. Conclusions
The results of this study showed that the overall average dimensions of safety culture improved compared to before the IMA, indicating that the expectations of hospital managers and research goals were met in most cases. These improvements include enhancing the quality and satisfaction of the patient safety culture, improving the technical and scientific skills and literacy of faculty and clinical staff, and increasing staff awareness of patient safety through repeated training.