1. Background
Diabetic retinopathy (DR) is a significant complication of diabetes and is one of the primary causes of vision impairment and blindness among adults worldwide (1, 2). The global prevalence of diabetes is on the rise, leading to an increase in the incidence of DR and presenting significant public health challenges (3). Diabetic retinopathy develops when high blood sugar levels damage the blood vessels in the retina, potentially leading to progressive vision loss if not effectively managed (4). Early detection and consistent management of DR are crucial in preventing severe visual impairment (5). However, many patients struggle with adhering to treatment plans and regular monitoring, which are vital for effective disease management (6, 7).
In the 2022 guidelines for self-care interventions published by the World Health Organization (WHO), self-care is defined as the capability of individuals and communities to maintain and enhance health, prevent disease, and manage illness and disability with or without the assistance of healthcare professionals (8). This comprehensive definition underscores the critical role that self-care plays in health maintenance and disease prevention (9).
The advancement of smart technologies and mobile applications is pivotal to the transformation of healthcare delivery (10). This transformation has been accelerated by the COVID-19 pandemic, which emphasized the vital role of mobile phones in enabling accurate and effective communication between patients and healthcare providers (11, 12). The pandemic demonstrated that mobile phones could be invaluable tools in ensuring continuity of care and providing timely health interventions, even when face-to-face consultations are not feasible (13).
The proliferation of mobile phones, which are now commonly used for calls, text messaging, and Internet access, has dramatically altered the landscape of healthcare delivery (14). These devices have expanded the reach and precision of healthcare services, enabling a level of access and engagement that was previously unattainable (15). Mobile Health applications (mHealth) represent a significant aspect of this technological revolution, providing a wide range of healthcare services and information to users globally (16). The increasing use of mHealth apps reflects their potential to support various aspects of healthcare, from chronic disease management to health promotion and education (17).
The increasing prevalence of diabetes and its complications, such as DR, underscores the need for innovative approaches to support patient self-care and disease management (18). Traditional healthcare systems often face challenges in providing continuous and personalized care due to resource limitations and the increasing patient load (19). In this context, mHealth applications have emerged as a promising solution to enhance patient engagement and self-management (17). These applications leverage the widespread use of smartphones and other mobile devices to deliver healthcare services and information directly to patients, providing a convenient and accessible means of managing chronic conditions like DR (7, 20). Mobile Health applications offer several advantages in the management of DR. They can provide patients with real-time access to health information, self-monitoring tools, reminders for medication and appointments, and educational resources (21). These features empower patients to take an active role in managing their condition, leading to better adherence to treatment regimens and improved health outcomes (22). Additionally, mHealth applications can improve communication between patients and healthcare providers, enabling more timely interventions and personalized care (23).
Extensive research has unequivocally proven the remarkable effectiveness of mHealth applications in managing chronic diseases. For instance, applications designed for diabetes management have shown positive results in improving glycemic control, increasing patient knowledge, and enhancing self-care practices (24). However, there is a need for applications specifically tailored to the unique needs of DR patients (2). Such applications should address the specific challenges associated with DR management, such as the need for regular eye examinations, monitoring of visual symptoms, and adherence to complex treatment protocols (20). This groundbreaking study is dedicated to crafting and assessing a cutting-edge mHealth application custom-built to empower diabetic retinopathy patients to take charge of their own self-care.
2. Objectives
The objectives include identifying critical features for inclusion, designing a self-care application for DR patients, assessing the application's usability, and evaluating its impact on self-care practices and glycemic control.
3. Methods
3.1. Study Design
This Participatory Design study was conducted in two primary stages: The design and evaluation of the mHealth application. The study was carried out in 2024, focusing on creating a comprehensive tool to assist patients with diabetic retinopathy in self-managing their condition. The study was designed to be iterative, incorporating feedback from stakeholders and end-users at various stages to ensure the app’s functionality and usability.
3.2. Application Design
3.2.1. Literature Review and Requirement Gathering
The design phase began with a thorough literature review conducted in January 2024. The databases searched included PubMed, Web of Science, Scopus, and Medline. The search terms used were “diabetic retinopathy,” “self-care,” “self-management,” “mobile health,” and "usability testing," focusing on publications from February 1, 2014, to June 31, 2024. This review aimed to identify key functional requirements and challenges faced by diabetic retinopathy patients (Table 1).
| Section | Details |
|---|---|
| Phase | Design |
| Activity | Literature review and requirement gathering |
| Time frame | January 2024 |
| Databases searched | PubMed, Web of Science, Scopus, Medline |
| Search terms | "Diabetic retinopathy," "self-care," "self-management," "mobile health," "usability testing" |
| Publication focus period | February 1, 2014, to June 31, 2024 |
| Objective | Identify key functional requirements and challenges faced by diabetic retinopathy patients |
3.2.2. Expert Panel
An expert panel was convened, comprising two endocrinologists, two ophthalmologists, and two health informatics experts. The panel discussed and refined the application’s functional requirements and information content.
3.2.3. Conceptual Model Development
Based on the input from the expert panel, a conceptual model of the application was created using Microsoft Visio 2021. This model included functional, structural, and behavioral components, ensuring comprehensive coverage of the app's intended capabilities. The conceptual model was reviewed and validated by two additional medical informatics experts to ensure all requirements were adequately addressed.
3.2.4. Application Programming
The application was programmed using Java within the Android Studio 2021 environment. The design team focused on creating a user-friendly interface, ensuring robust performance, and integrating all required functionalities as identified in the conceptual model. Following the initial development, the app underwent several rounds of testing and debugging to ensure reliability and usability.
3.3. Application Evaluation
3.3.1. Study Participants
During the evaluation phase, we recruited 30 patients with diabetic retinopathy from a diabetes care center affiliated with Ahvaz Jundishapur University of Medical Sciences. The inclusion criteria for participants were as follows: Diagnosed with diabetic retinopathy, aged between 35 and 60 years, owning an Android smartphone, being information literate in using a smart mobile phone, and willing to participate in the study. Ethical approval was obtained from the university's ethics committee, and all participants provided informed consent.
The exclusion criteria for participants were as follows: Not diagnosed with diabetic retinopathy, not aged between 35 and 60 years, not owning an Android smartphone, or not able to use a smart mobile phone.
3.3.2. Usability Testing
We conducted usability testing of the application using the Mobile Application Usability Questionnaire (MAUQ) developed by Zhou et al. (25). The MAUQ assesses usability across three dimensions: Ease of use, user interface and satisfaction, and usefulness, using a 7-point Likert scale (1 = completely disagree, 7 = completely agree). Since a Persian version of the questionnaire was not available, we translated it into Persian. The translated questionnaire was then back-translated into English by two proficient translators to ensure cross-cultural adaptation. The face validity was assessed by two medical informatics experts, and its reliability was verified in previous research (25-27). The reliability was re-evaluated, and an internal correlation coefficient of 0.94 was determined using Cronbach's alpha.
3.3.3. Data Collection and Analysis
Participants received the application and were given instructions on how to use it. After two weeks, they completed the questionnaire. Data were collected and analyzed using SPSS 26. Descriptive statistics, such as mean and standard deviation, were calculated for each usability dimension. Additionally, the overall usability score was categorized into quartiles: Poor (0 - 1.75), moderate (1.76 - 3.50), good (3.51 - 5.25), and very good (5.26 - 7.00).
4. Results
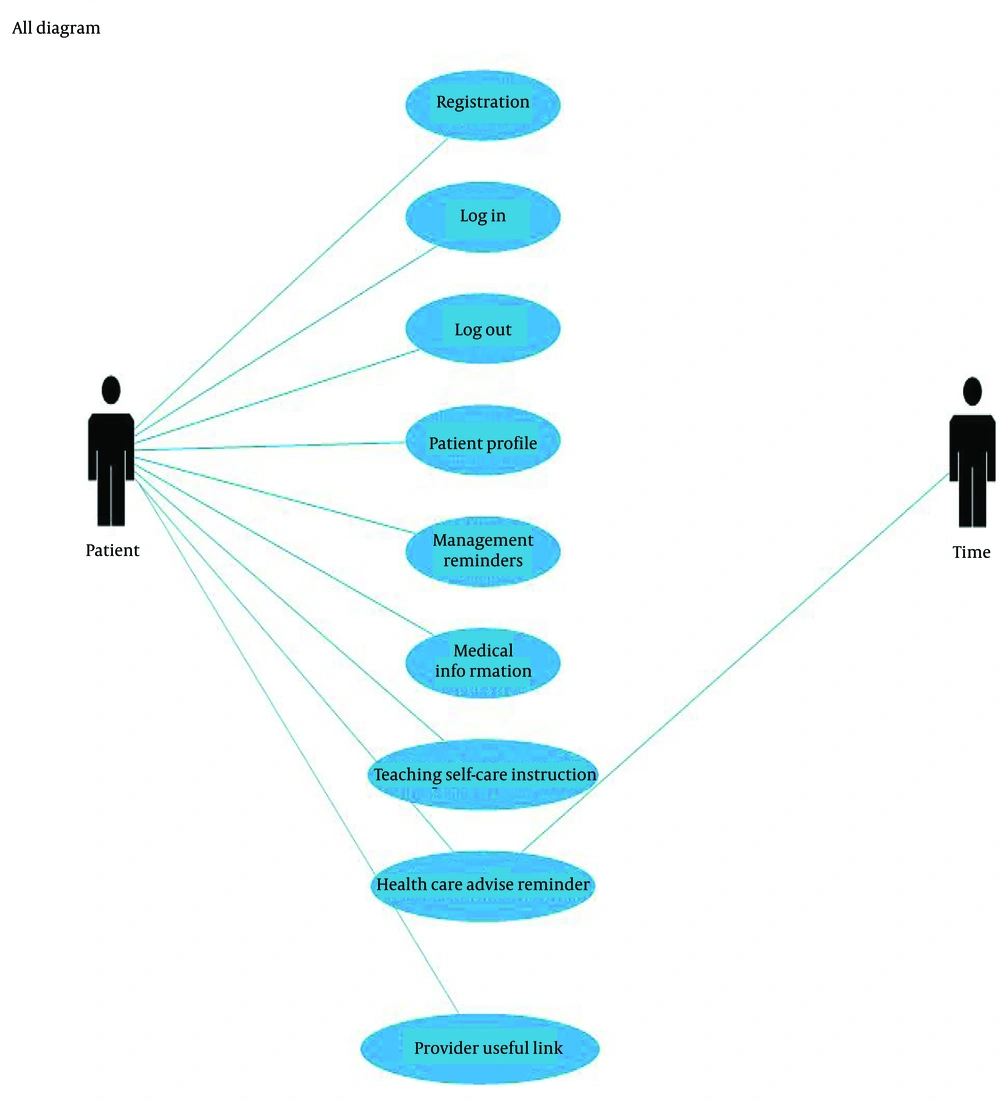
The functional requirements identified in the literature review were discussed with expert panels to confirm their incorporation into the application design (Table 2). The comprehensive use-case diagram of the application is depicted in Figure 1. The application's core features encompass alarms, reminders, medical information, self-care guidelines for retinopathy patients, patient profiles, and access to useful links. The expert panel was composed of an equal number of male and female participants, with three males and three females, each representing 50% of the panel. All proposed requirements received approval from the panel, with an additional requirement for useful links being suggested, discussed, and subsequently approved by the members.
| Functional Requirement | Overview |
|---|---|
| 1. Sign up | The application should enable users to create an account by entering a username and password. |
| 2. Log in | The application should allow users to log in using their username and password. |
| 3. Log out | The application should include a feature that allows users to log out. |
| 4. Alerts management | The application must alert the user about any harmful conditions. |
| 5. Reminders management | The application should remind users to take their medications and attend doctor appointments. |
| 6. Eye exercises | The application should offer users eye exercises. |
| 7. Providing medical information | The application should provide information about eye anatomy, diabetes, and diabetic retinopathy. |
| 8. Providing self-care guidelines for retinopathy patients | The app should provide information about medication management, proper diet, psychological needs management, eye health, daily activities, and doctor appointment follow-up. |
| 9. References and useful links | The application should offer the user useful links. |
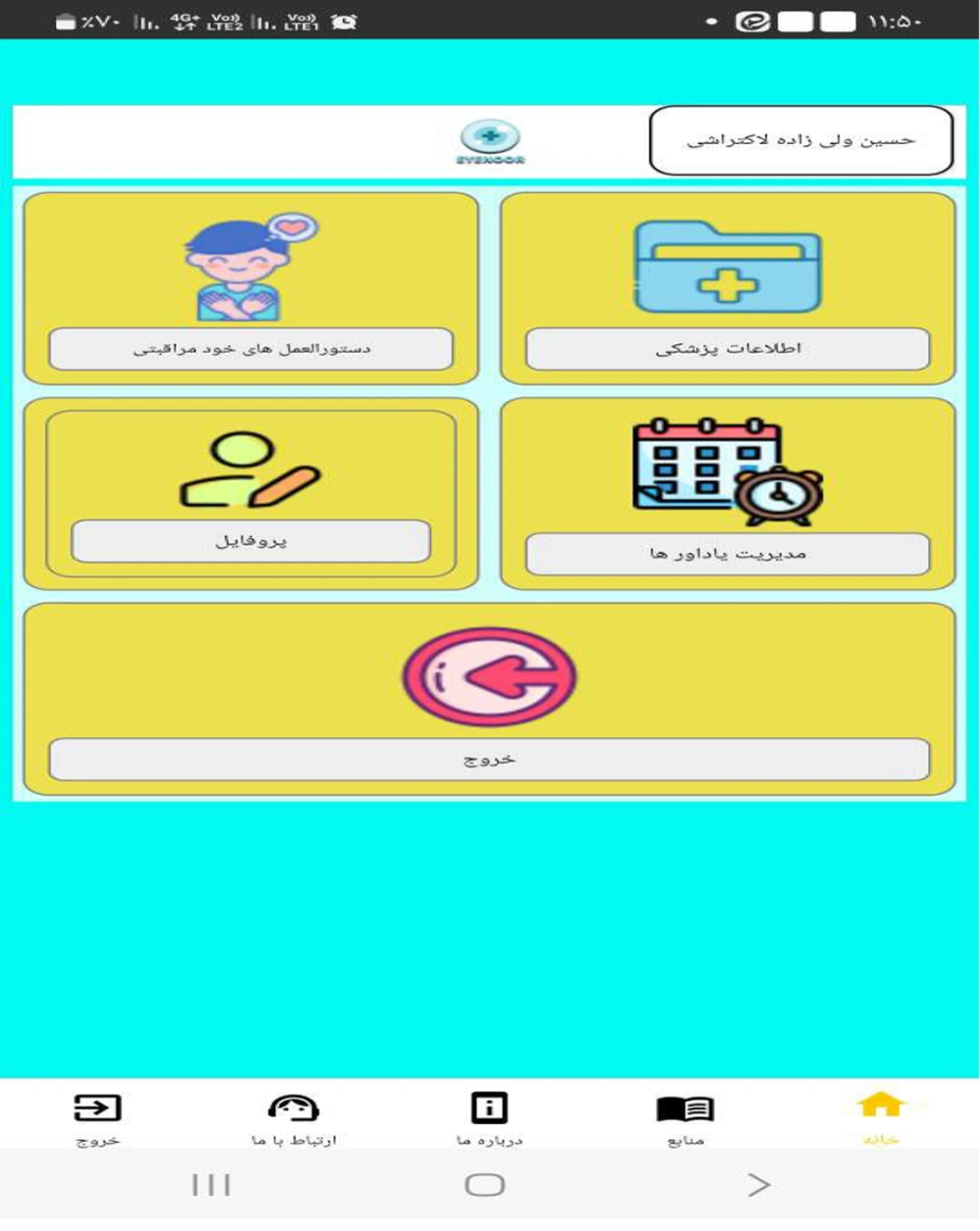
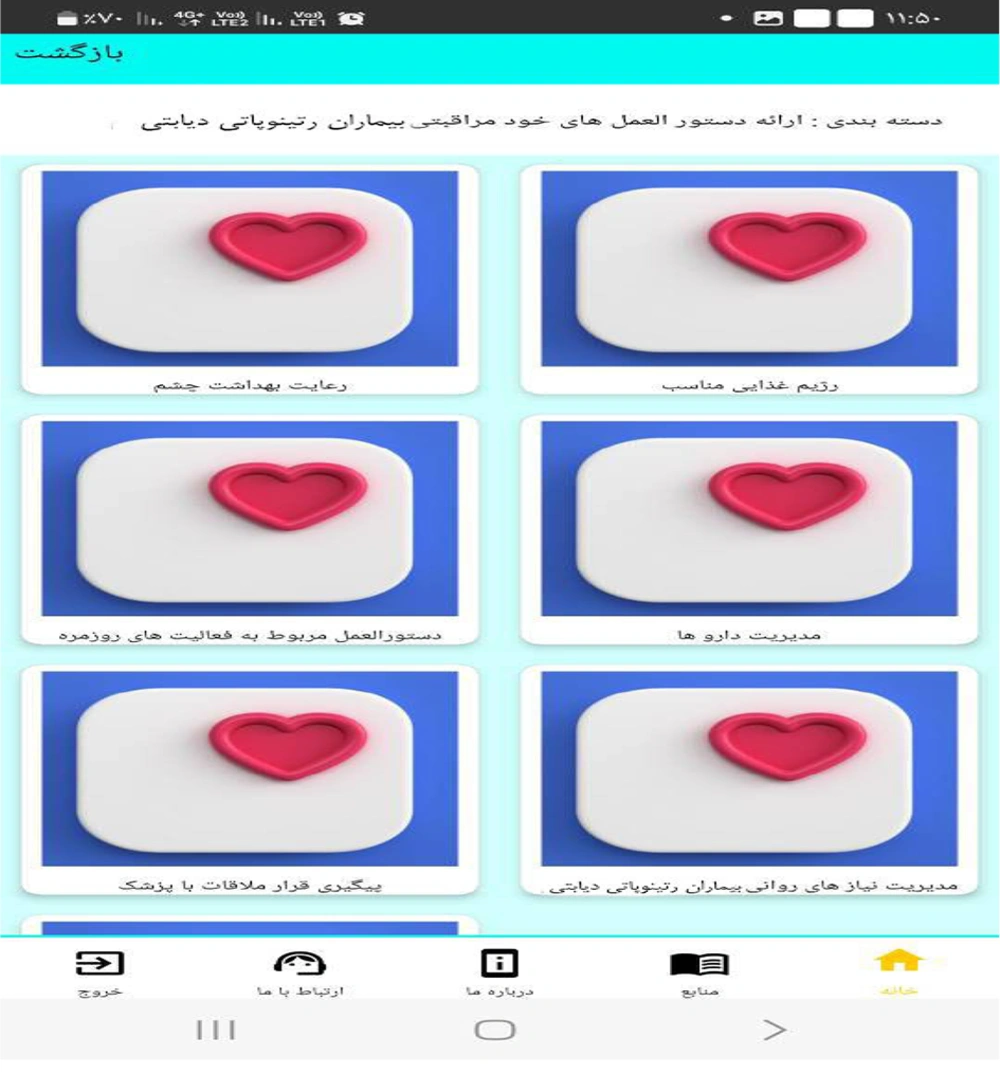
The home page of the application is designed to provide users with a comprehensive array of features related to medical information, self-care instructions, reminder management, and patient profiles (Figure 2). Within the self-care guidelines section, users can access valuable information regarding diet, eye hygiene, medication management, daily activity recommendations, psychological support for diabetic retinopathy patients, and guidance on scheduling and attending doctor's appointments (Figure 3). Additionally, the application offers useful resources and external links for further research and information (Figure 2).
The reminder management function of the application allows users to input and track medications, including dosage and administration times. Users can also set reminders for appointments and other health-related activities. This feature aims to enhance medication adherence and ensure timely follow-up with healthcare providers (Figure 4).
The study involved a total of 30 participants diagnosed with diabetic retinopathy. The participants' demographic characteristics are summarized in Table 3. The average age was 52.4 years with a standard deviation of 9.3 years. The gender distribution was relatively balanced, with a slight predominance of female participants (60%). The majority of the participants had completed secondary education (44%), followed by those with primary education (36%), and a smaller percentage holding a bachelor’s degree (20%).
| Characteristic | Values |
|---|---|
| Number of participants | 30 |
| Average age (y) | 52.4 ± 9.3 |
| Gender distribution | |
| Female | 60 |
| Male | 40 |
| Educational level | |
| Primary education | 36 |
| Secondary education | 44 |
| Bachelor's degree | 20 |
a Values are expressed as % unless otherwise indicated.
The usability of the mHealth application was assessed using the MAUQ. The MAUQ evaluates usability across three dimensions: Ease of use, user interface and satisfaction, and usefulness. Participants rated each item on a 7-point Likert scale, where 1 indicates strong disagreement and 7 indicates strong agreement.
The overall usability score was high, with a mean score of 5.67 ± 1.04, indicating an excellent usability rating. The ease-of-use dimension received the highest average score (6.12 ± 0.84), followed by user interface and satisfaction (5.58 ± 1.10), and usefulness (5.32 ± 1.18). Detailed scores for each dimension are presented in Table 4.
| Dimension | Mean Score ± SD |
|---|---|
| User-friendly | 6.12 ± 0.84 |
| User interface and satisfaction | 5.58 ± 1.10 |
| Usefulness | 5.32 ± 1.18 |
| Overall usability | 5.67 ± 1.04 |
Participants provided qualitative feedback during post-evaluation interviews, highlighting several key aspects of the application. Positive feedback included a user-friendly interface, comprehensive educational content, and helpful reminders for medication and appointments. Some participants suggested additional features, such as integration with other health monitoring devices and personalized health tips based on their data.
5. Discussion
The study aimed to design and evaluate an mHealth application to aid in the self-care of diabetic retinopathy. The findings from the usability testing of the application demonstrated promising results in terms of user satisfaction, ease of use, and perceived usefulness. These outcomes highlight the potential impact of digital health solutions on improving self-care practices among patients with chronic conditions such as diabetic retinopathy.
The high usability scores, particularly in ease of use, suggest that the application's design successfully met the needs of the target user group. This aligns with the principles of user-centered design, which emphasize the importance of creating intuitive and accessible interfaces to enhance user engagement and adherence (28, 29). The positive feedback on the user interface and overall satisfaction indicates that the application's aesthetic and functional design elements were well-received, contributing to a positive user experience. This is consistent with the findings of Rezaee et al., who reported high user interface satisfaction scores in a mobile application designed for adolescent self-care, further underscoring the significance of user-centered design in mHealth applications (30).
Despite the overall positive reception, the slightly lower score in the usefulness dimension indicates that there is still room for improvement in the application's functionality. Future iterations could benefit from incorporating more personalized features and leveraging advanced data analytics to provide users with tailored health recommendations and predictive insights. This would enhance the application's ability to deliver meaningful and actionable information to users, thereby increasing its perceived usefulness (31). For instance, Rezaee et al. highlighted the importance of personalized educational content in enhancing user engagement and self-care practices, suggesting a potential area for further development (30).
The study's findings are consistent with previous research on mHealth applications for chronic disease management. Coups and Ritterband found that mobile applications could effectively enhance self-management behaviors in patients with skin cancer, similar to the current study's findings for diabetic retinopathy (29). Additionally, Buller et al. demonstrated that a mobile sun safety application could positively influence user behavior and engagement, reinforcing the potential of mHealth solutions to promote healthy practices (28). Furthermore, the study by Langarizadeh et al. on a mobile-based nutrition education application for infertile women showcased the effectiveness of mHealth applications in promoting multiple health behaviors, which aligns with the potential observed in our study for diabetic retinopathy management (32).
Educational content is a crucial component of effective mHealth applications, as evidenced by Einollahi et al. and Karthikeyan et al. (31, 33). The current study incorporated comprehensive educational materials on diabetic retinopathy, which were well-received by users and contributed to their understanding and management of the condition. This underscores the importance of providing relevant and easily accessible educational resources in health applications to empower patients and support informed decision-making. Shanmugavel et al. also emphasized the necessity of high-quality, reliable educational content in mHealth applications for promoting self-care among diabetes patients, further validating our approach (34).
5.1. Limitations and Future Research
The study has shown promising results, but it is important to note some limitations. The findings may not be widely applicable due to the small sample size of 30 participants. To validate the results and gain a better understanding of the effectiveness of the application, future studies should include larger and more diverse populations.
Furthermore, the short duration of the evaluation period may not fully capture the long-term benefits and challenges associated with using the mHealth application. Longitudinal studies are needed to assess the sustained impact on health outcomes, adherence to self-care routines, and patient satisfaction over time.
In order to improve the application's capabilities, it is important to consider integrating advanced technologies such as artificial intelligence (AI) and machine learning (ML) in future research. These technologies have the potential to facilitate the creation of predictive algorithms that analyze user data. This analysis can be used to offer personalized health recommendations and provide early warnings about potential complications.
Additionally, further work is needed to refine the application's features based on user feedback and evolving needs. Continuous updates and iterative development will ensure the application remains relevant, user-friendly, and effective in meeting the demands of patients with diabetic retinopathy.
5.2. Conclusions
The mHealth application developed for the self-care of diabetic retinopathy patients, as discussed in this study, demonstrates significant potential to enhance patient self-care alongside traditional medical treatments. The high scores for ease of use and user satisfaction highlight the importance of involving end-users in the design process, ensuring that the application meets their needs effectively.
However, the usefulness, though rated as good, suggests room for improvement, particularly in integrating more clinical functionalities and personalized features. Future work should focus on expanding the application to other operating systems and extending the evaluation period to assess long-term benefits and impacts on patient behavior and clinical outcomes. Broader and more diverse user testing could also help refine and validate the app’s functionalities, ensuring its adaptability and effectiveness across different populations.
In conclusion, the study underscores the critical role of user-centered design in developing mHealth applications that not only support medical treatments but also empower patients in their self-care routines. By continually involving users in the development and evaluation process, such applications can achieve higher usability and relevance, ultimately contributing to better health outcomes and more efficient healthcare delivery.