1. Background
Chronic obstructive pulmonary disease (COPD) represents a significant contributor to the incidence of illness and death in economically advanced nations (1). This disease is characterized by reduced airflow in the airways, which has a progressive course. It is manifested with shortness of breath, cough, and phlegm. It includes emphysema, chronic bronchitis, or a combination of these disorders (2, 3). Various pathophysiological processes, such as reduced lung growth in early life, exposure to cigarette smoke, air pollution, and infections, are involved in it (4). This disease affects about 384 million people worldwide, and it is estimated that half of them may be undiagnosed (1). It constitutes the fourth leading cause of mortality on a global scale. According to projections from the World Health Organization (WHO), it is anticipated to ascend to the position of the third leading cause of death worldwide by the year 2030, attributable to the escalation in exposure to various risk factors and the demographic shift towards an older population (5, 6). This pathological condition has the potential to cause systemic complications (7). It creates a vicious cycle that prevents recovery and ultimately leads to reduced quality of life due to some behavioral patterns such as reduced levels of physical and social activities (8, 9). Quality of life is considered a key characteristic in evaluating the disease severity and reacting to treatment, and it is used as an implementation to assess patients (10).
Obstructive sleep apnea (OSA) is a respiratory disorder associated with the narrowing of the upper airway, leading to disturbances in natural ventilation during sleep (11). The OSA impacts the quality of life in multiple ways. Some studies attribute the long-term consequences of the condition, such as cardiovascular and endocrine disorders, to the decline in quality of life. Conversely, other research suggests that excessive daytime sleepiness is the principal factor leading to reduced quality of life among these individuals (12). The COPD and OSA are distinct diseases with differing symptoms that can exacerbate one another. The simultaneous occurrence of OSA in patients with COPD is referred to as overlap syndrome, which has been reported in systematic reviews at rates ranging from 2.9% to 65.9%. This syndrome significantly affects the quality of life of those afflicted (13, 14). More than 60% of these patients complain of sleep disturbances and fatigue during the day (15). Sleep quality is the primary factor in these people’s quality of life. Poor sleep quality in these patients predicts their low survival (13).
Although this problem is known, a few studies in the world have evaluated the effect of various factors on the quality of life of these patients (9). Zohal et al. conducted a cross-sectional and descriptive study to investigate the quality of sleep and life in patients with COPD with and without OSA referred to a respiratory clinic in Qazvin province. In this regard, 139 patients were investigated. All patients were evaluated to determine the severity of the disease with pulmonary function testing. In addition, the Berlin Questionnaire (BQ), Epworth Sleepiness Scale (ESS), Pittsburgh Sleep Quality Index (PSQI), and St. George Respiratory Questionnaire (SGRQ) were used to evaluate them. It was found that sleep quality is significantly correlated with quality of life, and individuals diagnosed with overlap syndrome exhibited inferior sleep quality and diminished quality of life in comparison to individuals who do not present with this condition. Stepwise multiple regression analysis revealed that the severity of COPD, OSA, and sleep quality exert significant influences on the quality of life experienced by these individuals (10).
Furthermore, our investigation revealed an absence of studies within the clinical treatment framework of Khuzestan province that examine the impact of various factors on the quality of life experienced by these patients. Individuals with COPD should maintain a lifestyle characterized by moderate activity in an environment with minimal pollutants, temperature fluctuations, and humidity levels. It is advisable for these patients to avoid triggers that may provoke coughing episodes, including emotional stressors and challenging situations (14). Given the unique geographical and climatic features of Khuzestan province, such as its varying weather conditions from northeast to southwest, residents face increasingly incompatible climates. The region’s high annual temperatures, elevated mean relative humidity, and significant air pollution levels compared to other provinces contribute to stressful living conditions. In addition to the above, the multi-ethnic nature of this province, the existence of different cultures, the continuation of hot weather until the end of the evening, and the planning of daily activities outside the home for the early hours of the night can also affect the quality of life of these patients.
2. Objectives
Consequently, the present study aimed to identify factors predicting quality of life, including OSA risk, sleep quality, and demographic variables among COPD patients in this province. We anticipate that clinical interventions conducted by healthcare professionals will enhance their quality of life and improve survival rates through a better understanding of these factors.
3. Methods
3.1. Participants
The current cross-sectional and descriptive investigation was undertaken on 110 patients with COPD referred to respiratory clinics of Imam Khomeini and Golestan hospitals in Ahvaz city and Khatam al-Anbia in Shoushtar city. A convenience sampling method was employed over a six-month period (April to September 2023). The sample size was calculated to be 110 individuals based on a one-sample mean, referencing the study by Zeidler et al. (9), with a standard deviation for the quality of life score set at S = 19.7, an error rate (α) of 0.05, and a desired accuracy (d) of 3.7. The sample size was calculated using the formula below.
3.2. Eligibility Criteria for Participants
The cohort consisted of adult individuals diagnosed with COPD by a physician, who were in stable physical condition and had no history of mental disorders. Exclusion criteria included medical conditions that could result in sleep disturbances, such as significant chronic pain, symptomatic heart failure, malignancies, dementia, mental or cognitive impairments, other pulmonary diseases, inability to communicate effectively, and unwillingness to participate.
3.3. Tools
The data collection tool covers four parts: (1) Demographic features (age, sex, marital status, duration of disease, employment status, underlying disease, history of sleep disturbances, smoking, and history of taking sleeping pills); (2) the BQ, developed by Netzer et al., was used to assess the risk factors of OSA (16). The BQ encompasses a total of ten inquiries categorized into three distinct classifications. The initial classification comprises five questions pertaining to the phenomenon of snoring. The subsequent classification consists of three items related to the occurrence of daytime somnolence. The final classification incorporates two items addressing the historical prevalence of hypertension or a Body Mass Index (BMI) exceeding 30 kg/m2. High-risk sleep apnea was classified as such if individuals exhibited affirmative scores in two or more of the three designated categories, whereas those categorized as low-risk for sleep apnea demonstrated positive scores in fewer than two categories. The psychometric properties, specifically validity and reliability, of the Persian version of this questionnaire were assessed in a study conducted by Amra et al. in 2012 (17). Reliability analysis for the BQ categories yielded Cronbach’s alpha values of 0.70 for category 1 and 0.50 for category 2. Positive responses for BQ categories 1 through 3 were recorded in 88.5%, 67.5%, and 66.9% of patients, respectively; (3) the PSQI was employed to assess the quality of sleep. This index was formulated by Buysse et al. at the Psychiatric Institute of Pittsburgh. The instrument comprises 18 distinct items and encompasses seven subscales pertaining to the subjective assessment of sleep quality. The variables evaluated include sleep latency, total sleep duration, habitual sleep efficiency, the frequency of sleep disturbances, the use of pharmacological agents for sleep assistance, and the occurrence of dysfunction during daytime hours. Each of these variables is evaluated utilizing a Likert scale that ranges from 0 to 3. They are elucidated in the following manner. Absence of sleep disturbances: Score 0, moderate sleep disturbances: Score 1, severe sleep disturbances: Score 2, and extremely severe sleep disturbances: Score 3. A cumulative score greater than 5 on the entire questionnaire signifies suboptimal sleep quality (18). In the Iranian adaptation of this questionnaire, the validity was reported to be 0.86, while the reliability was assessed at 0.89. Additionally, another study reported the reliability of the questionnaire as 0.46 using Cronbach’s alpha method and 0.52 utilizing the split-half method (19); (4) A health-related quality-of-life measurement instrument included a translated version of the SGRQ. This questionnaire has 76 items. This instrument has been employed in the context of numerous pulmonary pathologies, including asthma and COPD. The understanding of this evaluative tool is both clear and well-accepted (20). The study conducted by Fallah Tafti et al. demonstrated that this instrument possesses adequate validity and reliability, making it suitable for the respiratory assessment of patients with chronic respiratory diseases. The calculated Cronbach's alpha coefficient was 0.93 (21). This questionnaire includes three subscales: (1) Symptoms, (2) disease effect, and (3) activity. The symptom subscale of this questionnaire includes eight items that measure cough, sputum, shortness of breath, wheezing, and the number of attacks. Each question has 4 - 5 options based on the frequency of symptoms or attacks. The subscale of disease effect examines the impact of the disease on the individual’s social and emotional functioning (for example, employment, feeling embarrassed in society, self-satisfaction, taking medications, and attitudes about one's health level). The activity subscale examines physical activities that cause shortness of breath (for example, washing clothes, or climbing stairs) or the level of the effects of shortness of breath (for example, shortness of breath causes washing to take longer than usual). The questions of the subscale of disease activity and impact are true/false. In addition, the total score of this questionnaire is obtained by summing up the scores of the mentioned scales by considering a coefficient for each subscale. Each of the subscales of the questionnaire and the total score will be between 0 and 100. A higher score indicates a more unfavorable state of quality of life on that scale (20).
3.4. Procedure
The patients who met the inclusion criteria were selected after obtaining permission from the Ethical Oversight Committee of the Shoushtar Faculty of Medical Sciences, presenting a letter of introduction to the respiratory clinic officials, providing the necessary explanations to the research subjects, and obtaining their written consent to participate in the study. Data were collected using a demographic checklist, the BQ, PSQI, and SGRQ-St questionnaires.
3.5. Ethical Considerations
Upon the endorsement of the proposal by the Research Committee and the acquisition of the code of ethics from the Ethics Committee of the Shoushtar Faculty of Medical Sciences (IR.SHOUSHTAR.REC.1401.014), the requisite authorizations for the acquisition of data were granted to Khatam Al-Anbia and Imam Khomeini hospitals by the faculty. The importance of maintaining the confidentiality of all information obtained from the records was underscored.
3.6. Statistical Analysis
Quantitative variables were expressed as mean (median), standard deviation (interquartile range), as well as minimum and maximum values. Qualitative variables were represented as counts (percentage). The normality of quantitative variables was assessed using the Kolmogorov-Smirnov test. The Pearson correlation coefficient was used to examine relationships between quantitative variables. Independent t-tests compared means between groups, and ANOVA (analysis of variance) assessed differences across variable levels. Multiple linear regression was performed, and multicollinearity was evaluated using tolerance and variance inflation factor (VIF) statistics. A significance threshold of 0.05 was employed in the present reaserch. Data were analyzed using SPSS-22 software.
4. Results
In this study, 100 subjects participated. Their mean age was 54.59 ± 10.62. In this regard, 89.1% were male, 90.9% were married, and 54.5% were retired. In addition, 59.1% had less than 6 years of infection. The history of underlying diseases, especially hypertension, was 54.5%. Regarding the hospitalization history, 72.7% had a history of hospitalization in internal and intensive care units. Most of the people participating in the study (91.8%) had a history of smoking. Finally, 22.7% reported a history of sleep disturbances. Married subjects had a better quality of life compared to single subjects (P < 0.001). A statistically significant correlation was also identified between the classification of employment and the overall quality of life (P = 0.001). The quality of life decreased as the duration of the disease increased (P = 0.028). Patients with a history of sleep disturbances also had a lower quality of life (P < 0.001) (Table 1). According to the results of the Kolmogorov-Smirnov test, the data distributions for sleep quality (P = 0.12) and quality of life (P = 0.09) were found to be normal.
| Demographics | No. (%) | Quality of Life (Mean ± SD) | P-Value |
|---|---|---|---|
| Age | 0.557 | ||
| 30 - 45 | 20 (18.2) | 58.78 ± 19.35 | |
| 45 - 60 | 55 (50.0) | 53.46 ± 25.50 | |
| 60 -75 | 35 (31.8) | 51.68 ± 22.73 | |
| Gender | 0.394 | ||
| Female | 12 (10.9) | 59.36 ± 20.09 | |
| Male | 98 (89.1) | 53.19 ± 23.94 | |
| Marital status | 0.000 b | ||
| Married | 100 (90.9) | 56.75 ± 21.98 | |
| Single | 10 (9.1) | 25.00 ± 19.64 | |
| Employment history | 0.001 b | ||
| Retired | 60 (54.5) | 56.89 ± 21.55 | |
| Unemployed | 5 (4.5) | 77.27 ± 0.01 | |
| Self-employed | 35 (31.8) | 52.02 ± 23.24 | |
| Employed | 10 (9.1) | 30.45 ± 25.39 | |
| Duration of disease | 0.028 c | ||
| < 24 | 35 (31.8) | 45.41 ± 18.52 | |
| 24 - 72 | 30 (27.3) | 53.71 ± 35.57 | |
| 72 - 120 | 20 (18.2) | 57.04 ± 22.59 | |
| > 120 | 25 (22.7) | 63.34 ± 14.80 | |
| History of underlying disease | 0.987 | ||
| Yes | 60 (54.5) | 53.90 ± 22.18 | |
| No | 50 (45.5) | 53.82 ± 25.33 | |
| Smoking | 0.917 | ||
| Yes | 101 (91.8) | 53.93 ± 21.15 | |
| No | 9 (8.2) | 53.08 ± 44.31 | |
| History of sleep disturbance | 0.000 b | ||
| Yes | 25 (22.7) | 73.36 ± 8.28 | |
| No | 85 (77.3) | 48.13 ± 23.53 | |
| Using sleeping medication | 0.439 | ||
| Yes | 25 (22.7) | 57.09 ± 18.98 | |
| No | 85 (77.3) | 52.92 ± 24.76 |
a Independent t-test or ANOVA were used.
b Significance at 0.01 level.
c Significance at 0.05 level.
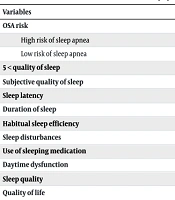
Based on the results of the reaserch, 45 patients (40.9%) were at high risk of OSA. The mean sleep quality score of the patients was 6.55 (4.53). Among them, 65 people (59.01%) had poor sleep quality, and 40.09% had good sleep quality. The mean quality of life score of the patients was 53.86 (23.55). In addition, 15 people (13.6%) had a very good quality of life, 35 people (31.8%) were at a good level, 35 people (31.8%) were at a moderate level, and 25 people (22.7%) were at a poor level (Table 2).
| Variables | No. (%) or Mean ± SD |
|---|---|
| OSA risk | |
| High risk of sleep apnea | 45 (40.9) |
| Low risk of sleep apnea | 65 (59.1) |
| 5 < quality of sleep | 65 (59.1) |
| Subjective quality of sleep | 0.68 ± 0.54 |
| Sleep latency | 1.31 ± 1.06 |
| Duration of sleep | 0.86 ± 0.72 |
| Habitual sleep efficiency | 0.86 ± 0.64 |
| Sleep disturbances | 10.63 ± 0.71 |
| Use of sleeping medication | 0.18 ± 0.65 |
| Daytime dysfunction | 0.95 ± 0.82 |
| Sleep quality | 6.55 ± 4.53 |
| Quality of life | 53.86 ± 23.55 |
Abbreviation: OSA, obstructive sleep apnea.
There was a statistically significant and direct relationship between the total sleep quality score and the quality of life. This means that an increase in sleep disturbances led to a poorer quality of life (P = 0.002 and r = 0.287). The subscales of sleep latency (P < 0.001 and r = 0.395), sleep duration (P = 0.001 and r = 0.325), use of sleeping medications (P = 0.001 and r = 0.325), and daytime dysfunction (P = 0.013 and r = 0.237) had a significant and direct relationship with quality of life. The subscales of subjective quality of sleep, sleep disturbances, and habitual sleep efficiency had no significant relationship with quality of life (P < 0.05) (Table 3).
| Overall Quality of Life | Subjective Quality of Life | Sleep Latency | Sleep Duration | Sleep Disturbances | Use of Sleeping Medications | Daytime Dysfunctions | Habitual Sleep Efficiency | Total Sleep Quality |
|---|---|---|---|---|---|---|---|---|
| Pearson correlation | -0.015 | 0.395 b | 0.325 b | 0.042 | 0.325 b | 0.237 c | -0.043 | 0.519b |
| P-value (2-tailed) | 0.877 | 0.000 | 0.001 | 0.663 | 0.001 | 0.013 | 0.652 | 0.000 |
a Pearson's correlation coefficient test was used.
b Correlation is significant at 0.01 level (2-tailed).
c Correlation is significant at 0.05 level (2-tailed).
An evaluation of the quality of life and quality of sleep among patients in relation to the risk of sleep apnea reveals a noteworthy disparity in the quality of life experienced by individuals classified as having a high risk versus those categorized as having a low risk of sleep apnea (P = 0.001, P < 0.001). The difference in quality of life score in patients with a high risk of sleep apnea compared to patients without sleep apnea was 21.74 ± 4.08. This means that patients with a high risk of OSA had a poorer quality of life. Additionally, the difference in sleep quality score in patients with a high risk of sleep apnea compared to patients without sleep apnea was 3.23 ± 0.82, indicating that patients with a high risk of sleep apnea had a poorer sleep quality (Table 4).
a An independent t-test was used.
b Correlation is significant at 0.01 level (2-tailed).
The simultaneous effect of OSA and sleep quality variables on the quality of life was investigated by controlling significant demographic variables using a linear regression model. The independent variables were incorporated into the regression model, which was predicated on the hierarchy of their significance in elucidating the dependent variable. The final model had a good (F = 19.86, P < 0.001). Collinearity analysis indicated that there was no multicollinearity among the independent variables, as evidenced by a VIF of 1.14 and a tolerance value of 0.876. The two variables of OSA (β = 0.361, P < 0.001) and sleep quality (β = 0.268, P < 0.001) could explain and predict 27% of the changes in the quality of life variable (R-Square = 0.271). The normality of the residuals was evaluated using the Shapiro-Wilk test, which revealed that the residuals followed a normal distribution (P-value = 0.165) (Table 5).
| Models | Unstandardized Coefficients | Standardized Coefficients | t | P-Value | 95% Confidence Interval for B | Partial Squared | Collinearity Statistics | |||
|---|---|---|---|---|---|---|---|---|---|---|
| B | Std. Error | Beta | Lower Bound | Upper Bound | Tolerance | VIF | ||||
| Constant | 37.68 | 3.47 | - | 10.83 | 0.000 b | 30.79 | 44.58 | 0.538 | - | - |
| Sleep apnea | 17.23 | 4.20 | 0.361 | 4.09 | 0.000 b | 8.89 | 25.57 | 0.136 | 0.876 | 1.142 |
| Quality of sleep | 1.39 | 0.45 | 0.268 | 3.03 | 0.000 b | .484 | 2.30 | 0.079 | 0.876 | 1.142 |
Abbreviation: VIF, variance inflation factor.
a Multiple linear regression test was used.
b Significance at 0.01 level.
5. Discussion
The present study investigated some factors affecting the quality of life of patients with COPD. Sleep quality and the risk of OSA affected the quality of life of these patients. The risk of OSA was a better predictor than the quality of sleep in this regard. The study by Zohal et al. reported the significant effect of these two variables (10). However, Zeidler et al. concluded that poor sleep quality affects the quality of life of these patients more than the risk of OSA (9). Although both COPD and OSA have significant implications for respiratory function and the maintenance of normative oxygen saturation levels, they exhibit distinct differences in their underlying pathophysiological mechanisms. The COPD (usually including emphysema and chronic bronchitis) can narrow the airways by affecting the alveoli and bronchi and making the passage of air harder while awake. These patients also have trouble falling asleep due to difficulty breathing and wheezing, so they select the sitting position to relieve the respiratory symptoms. Although sitting may relieve the symptoms of difficulty breathing, sleeping makes it more difficult. Accordingly, COPD patients may suffer from insomnia since they are trying to find a comfortable sleeping position when they are awake. In contrast, OSA manifests during sleep. As the musculature at the posterior aspect of the pharynx undergoes relaxation, the lumen of the upper airway either constricts or occludes entirely, resulting in significant impediments to the individual’s ability to breathe. Therefore, OSA causes frequent and sudden awakenings at night. In addition, both diseases reduce the level of oxygen and increase the level of carbon dioxide in the blood. Consequently, the underlying disease mechanisms of COPD and OSA contribute to a further decline in sleep quality among individuals with overlap syndrome, ultimately resulting in a more significant reduction in the quality of life for this patient population. In contrast, patients who do not have OSA experience a decline in sleep quality solely due to the primary mechanism of their underlying disease, leading to a higher quality of life compared to those with overlap syndrome.
In the present research, about 40% of the patients were suffering from overlap syndrome, and the risk of OSA in these patients was much higher than the level estimated for the normal population. This result is the same with the results of the studies by Zohal et al. and Gislason et al. (10, 22).
Based on the results, among 7 subscales of the Petersburg Scale, the subscales of sleep latency, sleep duration, use of sleeping medications, and daytime dysfunctions, respectively, had the highest effect on the quality of life of patients. In the study by Zeidler et al., the three subscales of daytime dysfunction, sleep disturbances, and sleep latency, respectively, affected the quality of life of these patients (9). Sleep latency of more than 20 minutes increases the time of awakening during the night and decreases the duration of deep sleep. Circadian sleep rhythm disorder, daytime sleepiness, and increased stress levels due to the person’s worry about lack of sleep affect the daily performance and ultimately reduce the quality of life of the person.
The results of the present study indicate that marital status, employment status, duration of disease, and history of sleep disturbances were significantly correlated with the quality of life. However, no significant correlation was found between other demographic factors such as age, gender, underlying disease, smoking, use of sleeping medications, and quality of life. Consistent with the present study, the study by Bastani and Farajtabar reported a significant relationship between the duration of infection and quality of life (23). Suffering from this disease for a longer time will compromise sleep, and their quality of life will decrease for various reasons such as reduced physical and mental abilities, daytime disturbances, increased stress and worry about their health and future, social isolation, increased treatment costs and imposing a financial burden on patients and their families. Married people mostly enjoy more emotional and psychological support that can help reduce stress, increase life satisfaction, and improve their quality of life. The job type helps to improve the quality of life while providing peace of mind and financial security. In the present study, unemployed patients experienced the lowest quality of life, and people working in public organizations had the highest quality of life.
Farag et al. this investigation assessed the health-related quality of life in individuals diagnosed with COPD within the Egyptian context. In contrast to the findings of the present study, the authors inferred that factors such as advancing age and comorbid conditions, particularly hypertension, exhibited a significant correlation with quality of life metrics. The disparity in the climatic features, ethnicity, demographic characteristics, and sample size between the two investigations may account for this observed variation (24). Although the act of smoking did not demonstrate a significant impact on the quality of life within the current investigation, it did, however, exert an influence on the quality of sleep. Consequently, one may deduce that it has an indirect effect on the overall quality of life experienced by these patients. Cheng and Michael also concluded that the higher the mean number of cigarette packs per year, the worse the patient’s quality of life (25). Unlike the results of the present reaserch, the studies by Younas et al. and Masroor Roodsari et al. reported that men with COPD generally experience higher levels of quality of life than women with this disease (26, 27). The lack of difference between the quality of life of men and women with COPD in the present study is due to general reasons such as the need for expensive health care, the lack of proper structuring of centers, the need to stand in long queues to visit a physician, problems in completing forms needed, the overtired personnel, and having an unfavorable attitude toward the elderly to receive health care cause a decrease in their quality of life.
The following are some of the limitations of the present study: The present investigation was constrained by several factors, including the advanced age of the majority of the participants, their limited educational attainment, and a notable deficiency in the willingness to engage in the completion of multiple questionnaires. To solve this problem, the sampler read the questions for these patients. In a comprehensive review study entitled “Interventions to Enhance the Quality of Life of Individuals with COPD in Vietnam”, Vu et al. concluded that it is imperative to conduct empirical investigations on the efficacy of non-pharmacological interventions aimed at augmenting the quality of life for these patients (28). In this regard, Srijithesh et al. also concluded that positional therapy is less effective than continuous positive airway pressure (CPAP) in reducing the Apnea-Hypopnea Index (AHI) in COPD patients, but patients may use CPAP for a longer period during the night (29).
Based on the results of the present study, the risk of OSA is a more important factor than sleep quality on the quality of life of COPD patients, which can be controlled and treated by managing it in the form of lifestyle changes, use of a home CPAP machine, positional therapy during sleep, medication adherence, etc. In addition, observing sleep hygiene tips can also improve sleep quality, and ultimately, controlling these factors improves the quality of life of these patients by increasing productivity in daily life. It is advisable that subsequent research endeavors be undertaken to examine additional non-pharmacological interventions aimed at alleviating the aforementioned disorders and enhancing the overall quality of life for these patients.