1. Background
AIDS is now known as a crisis throughout the world. It is estimated that 33 million adults and children worldwide are infected with this virus (1). In Iran, 22727 cases of AIDS have been identified in 2011 (2). According to the latest report of the world health organization (WHO), it is estimated that mortality rate due to AIDS in the world has risen from 2.8 million people in 2002 to 5.6 million in 2030 (3).
Retrovirus is the cause of AIDS in human (the AIDS virus is a type of human retrovirus). This virus attacks the CD4+ T-lymphocytes (4). Following the suppression of the immune system and disease progression, especially when there are fewer than 200 T lymphocytes and CD4+ cells per milliliter, a variety of opportunistic pathogens become active and patients often suffer from viral, bacterial, and parasitic infections (5, 6).
The most important parasites that cause infections in people with impaired immune systems include Cryptosporidium, Isospora belli, Microsporidia, Entamoeba histolytica, Giardia intestinalis, Trichuris trichiura, Ascaris lumbricoides, Strongyloides stercoralis, and hook worms. They cause intestinal infections, severe diarrhea, and sometimes systemic infections (6).
One of the main problems of patients with AIDS is diarrhea and severe weight loss, which would be the cause of death too (7, 5). The rate of diarrhea in HIV-infected people in developed countries has been reported 30% - 60% and in developing countries like Africa, 90% (8). Unfortunately, in more than 50% of cases, the cause of diarrhea in HIV-positive and AIDS patients is undiagnosed. However, recently, gastrointestinal parasites are known as the major cause of diarrhea in these patients.
In a study conducted on 119 patients with AIDS in Nigeria in 2011, the prevalence of intestinal parasites was 7.22%, while in HIV-negative patients; it was 6.17% (2). In another study conducted in India in 2006, the prevalence of intestinal parasites in HIV-positive and AIDS patients was 5.37% and in most cases of diarrhea, Entamoeba and Cryptosporidium species were identified (7). Likewise, in a study conducted on 306 HIV-positive and AIDS patients in 2006 - 2008 in Khorramabad, the prevalence of intestinal parasites in HIV-positive and AIDS patients was reported 6.19% and 50%, respectively, indicating the high prevalence of intestinal parasites in AIDS patients (5). Various studies have shown that opportunistic infections are common feature of intestinal parasitic infections in areas with poor sanitation, especially in developing countries and tropical regions which leads to the deaths of approximately 80% of people with AIDS (9, 10). Currently, intestinal parasitic infections are a major concern for the disease control and care of HIV-positive individuals. Thus, the detection of these parasites and understanding the importance of the infection would help control the disease as well as better care of these people (8). Furthermore, in tropical regions, a relationship exists between HIV infection and other diseases such as malaria, tuberculosis, and intestinal parasitic infections, which if not diagnosed and treated early, would cause serious injuries and even death (5, 9).
Considering the importance of this topic and the irreparable consequences of missing infection in people with weak immune systems, we designed this study, as no studies have been conducted in Ahvaz to evaluate the prevalence of intestinal parasitic infections in HIV-positive individuals.
2. Objectives
This research has been designed to find the prevalence of intestinal parasitic infections in HIV-positive patients re continually referred to health centers in Ahvaz in 2011.
3. Patients and Methods
This study is a cross-sectional study, which was conducted to investigate the prevalence of intestinal parasites in HIV-positive patients referring to health centers (Western Ahvaz, 17th Shahrivar health center, Eastern Ahvaz health center, Sepidar health center) of Ahvaz city, Iran in 2012. The study population included all HIV-positive patients (N = 200) previously diagnosed with the disease, having case files in health centers with possible access to them in health-treatment centers affiliated to Ahvaz university of medical sciences. The study inclusion criteria were as follows: patient’s disease diagnosed by a specialist in infectious diseases at the time of the study, CD4+ count above 200, to be interested in participating in the study, not taking any medications affecting the gastrointestinal system and non-infectious diseases. The study exclusion criteria were as follows: lack of cooperation in filling out the questionnaire at any stages and unwillingness to participate in the study.
Diagnosis is based on diarrheal stool consistency (soft, loose, or watery stools) in a contract and consultation with an infectious disease expert and PMN number of dead cells per microscopic Shine contract diarrhea with mild, moderate, and severe split.
CD4 count was done by immunofluorescent tests in the reference lab (in Amaniyeh area). Moreover, these patients were active cases of health centers and their CD4 count were tested and recorded every 6 months.
At the beginning of the study, informed consent was obtained from all subjects. Then, to collect data, a researcher-made questionnaire was used. It contained demographic information (age, occupation, education level) and information on the history of medication use, diarrhea, and dyspepsia. The questionnaires were completed by the patients. After properly training of collecting sterilized samples, the 200 patients collected their fecal samples in specific plastic containers. On each sample, two routine parasitological tests, including direct expansion and formalin-ether concentration were conducted to identify eggs and larvae of worms and protozoan cysts and modified acid-fast staining method for detecting oocytes of Coccidia and spores of Microsporidia. It should be noted that in the end, those with positive identification of pathogenic intestinal parasites were referred to a specialist for prescribing medication and treatment.
In order to analyze the data, SPSS version 19 software was used to do descriptive and inferential statistical tests (Chi-square and ANOVA). P ≤ 0.05 was considered as significance level.
The initial plan of the study was approved by the Ethics Committee of Ahvaz Jundishapur University of Medical Sciences with code No. ETH-649.
4. Results
A total of 60 patients (30%) were from Western Ahvaz health center; 46 (23%) subjects from 17th Shahrivar health center; 45 (22%) patients from Eastern Ahvaz health center; and 49 (25%) patients from Sepidar health center.
About 34% of patients were under age 30, 43.5% between 31 and 40 years, 18% between 41 and 50 years, and 4.5% over 51 years old. Their education levels were as follows: illiterate, 12.5%; primary education, 20%; middle school, 30.5%; high school degrees, 26.5%; and college education, 10.5%. Their occupational status was as follows: self-employed, 39%; unemployed, 23.5%; other jobs, 37.5% (Table 1).
| Variables | Percentage |
|---|---|
| Age, y | |
| Under 30 | 34 |
| 31- 40 | 43.5 |
| 41- 50 | 18 |
| Over 51 | 4.5 |
| Education level | |
| Illiterate | 12.5 |
| Primary education | 20 |
| Middle school | 30.5 |
| High school degree | 26.5 |
| College education | 10.5 |
| Occupational status | |
| Self-employed | 39 |
| Unemployed | 23.5 |
| Other jobs | 27.5 |
Based on the results of gastrointestinal symptoms, 14.5% were asymptomatic, 74.5% had mild diarrhea, and 11% had severe diarrhea.
Regarding CD4+ count, it was below 499 in 28.5% of samples and above 500 in 71.5% of samples.
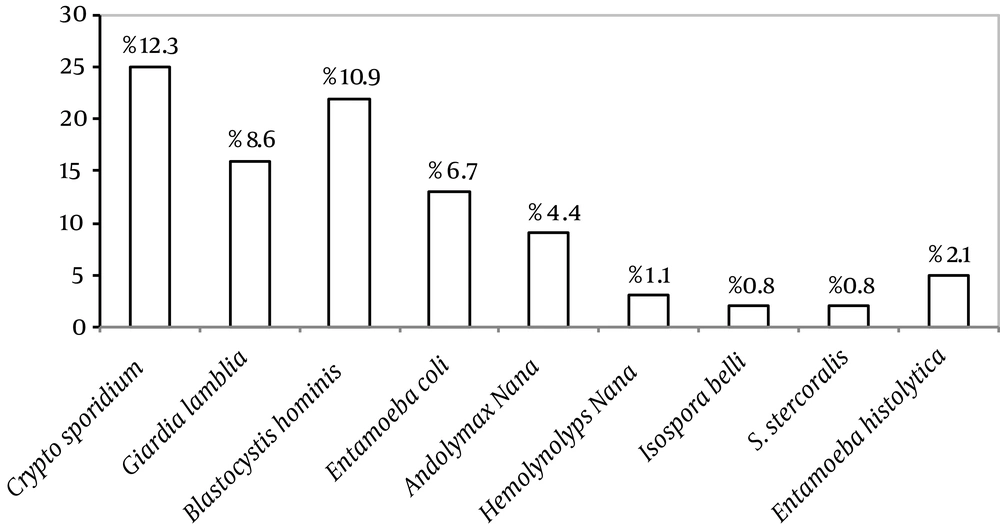
Parasitological test results showed that the overall prevalence of intestinal parasites was 48.5%. The prevalence rate of each parasite is given in Figure 1.
The results showed that 86 (43%) patients had parasitic infections and 103 (51%) patients were free of parasitic infection. The prevalences of intestinal parasites in different centers were as follows: Western Ahvaz health center: 44.3 %; 17th Shahrivar health center: 24.7%; Eastern Ahvaz health center: 21.63%, and Sepidar health center: 9.27%. Based on the results of the Chi-square test, there was a significant correlation between the sampling sites and prevalence of intestinal parasites (Table 2).
| Parasitic Species | Centers b | Total | |||
|---|---|---|---|---|---|
| Sepidar Health Center | East Health Center | 17th Shahrivar Health Center | West Health Center | ||
| Cryptosporidium | 3 (10) | 3 (10) | 5 (20.8) | 14 (32.6) | 25 (25.8) |
| Giardia lamblia | 0 | 3 (10) | 4 (16.7) | 9 (20.9) | 16 (16.5) |
| Blastocystis hominis | 2 (6.65) | 2 (6.65) | 8 (33.3) | 10 (23.3) | 22 (22.7) |
| Entamoeba coli | 4 (13.35) | 4 (13.35) | 0 (0) | 5 (11.60) | 13 (13.4) |
| Endolimax nana | 0 | 3 (10) | 2 (8.30) | 4 (9.30) | 9 (9.3) |
| Hymenolepis nana | 0 | 2 (6.70) | 1 (4.20) | 0 (0) | 3 (3.1) |
| Isospora belli | 0 | 0 (0) | 2 (8.30) | 0 (0) | 2 (2.1) |
| Strongyloides stercoralis | 0 | 2 (6.70) | 0 (0) | 0 (0) | 2 (2.1) |
| Entamoeba histolytica | 0 | 2 (6.70) | 2 (8.30) | 1 (2.30) | 5 (5.2) |
| Total | 9 (9.27) | 20 (21.63) | 24 (24.70) | 43 (44.30) | 97 (100) |
aData are presented as No. (%).
bP value = 0.044.
The Chi-square test results showed the variation of intestinal parasites prevalence in age groups (year): age group under 30, 38.1%; age group of 31 - 40, 37.1%; age group of 41 - 50, 20.6%, and age group over 50, 4.1%. There was a significant relationship between age group and the parasitological test results (P < 0.05). The prevalences of intestinal parasites in people based on education level were as follows: illiterates, 41.2%; primary education, 16.5%; secondary school degrees, 16.2%; high school degrees, 16.8%; and higher education levels, 9.3%. There was a significant correlation between educational level and prevalence of intestinal parasites (P = 0.001). The prevalences of intestinal parasites varied from 14.4% in self-employed people to 32% in unemployed and 53.6% in individuals with other professions. There was a significant relationship between job and the prevalence of intestinal parasites (P < 0.05).
Among the patients with parasitic infection, 7.2% were without diarrhea; 70.1% had mild diarrhea, and 22.7% had severe diarrhea. Based on the results, there was a significant correlation between different parasites prevalence and duration of diarrhea (P < 0.05). The results showed that 38.1% of people had dyspepsia and 61.9% showed no symptoms of dyspepsia. Based on the Chi-square test, there was no significant association between the risk of all kinds of intestinal parasites and dyspepsia (P = 0.103). At levels of 400 CD4+ and below, the prevalence of gastrointestinal parasites was equal to 28.5%, while at levels of 500 CD4+ and above, the prevalence of intestinal parasites was 71.5%. There was no significant correlation between parasitic infection and CD4+ levels (P = 0.293).
5. Discussion
The present study was conducted to determine the prevalence of intestinal parasites in HIV-positive patients attending health-treatment centers in the city of Ahvaz in 2012. The results indicated that the prevalence of intestinal parasitic infections in these patients was high. Studies from across the world on the intestinal parasites have reported high prevalence of these parasites in HIV-positive patients (11-14), which is consistent with the present study. In a study in 2004 by Hailemariam et al. in Ethiopia on 104 patients, it was found that of 78 HIV-positive patients, 41 patients (52.6%) and of 26 HIV-negative patients, 11 patients (42.32%) had gastrointestinal parasite infection; also multiple gastrointestinal parasite infections were common in these patients (15). In Iran, based on studies carried out in Tehran (16) and Khorramabad (5), the prevalences of intestinal parasites in HIV-positive patients were reported as 18.4% and 19.4%, respectively which represents a high incidence of opportunistic gastrointestinal parasites in AIDS and HIV-positive patients indicating that these patients need more care.
According to the current study results, the most common parasite found in HIV-positive individuals was Cryptosporidium species. In other studies, the only parasite significantly found more in HIV-positive individuals compared to HIV-negative subjects was Cryptosporidium, which is consistent with the present study (17, 18). In Vyas et al. study, the prevalence of Cryptosporidium (37.93%) in northern India and the prevalence of Isospora belli (31.3%) in southern India was more than other species (19). Also, in Akinbo et al. study in Nigeria in 2010, Cryptosporidium (22.2%) and Isospora belli (7.8%) species were seen as opportunistic infections (6), which are consistent with the present study and some other studies (20-24).
Mohandas et al. (2002) in India showed that 30% of HIV-positive patients were suffering from intestinal parasitic infections, 10.8% of which had Cryptosporidium parvum infection and 8.3% were diagnosed as having Giardia (giardiasis). In this study, of 36 HIV-positive patients, 27 patients (75%) had diarrhea, and the most common parasite associated with diarrhea was identified as Cryptosporidium, which is consistent with the results of this study (8). In a study in 2007 by Ramakrishnan et al. (7) on 80 HIV-positive patients, it was found that 38.7% of HIV-positive patients and 17.5% of HIV-negative individuals suffered from intestinal parasitic infections, from which 37.5% were infected by Entamoeba and 28.7% by Cryptosporidium. This may be due to immunological differences between individuals and nonobserving personal and environmental hygiene in individuals in this community (7).
In a study by Nkenfou et al. (9) in East Cameroon (2013) on 396 patients (42 HIV-positive patients and 345 HIV-negative patients), the results showed that the overall prevalence of parasitic infections in all patients in this study was equal to 14.64%, while 59.5% of HIV-positive and 9.32% of HIV-negative individuals had gastrointestinal parasitic infections. The most common known parasite in people infected included 19.04% for Cryptosporidium and 22.42% for Entamoeba coli, which may be due to the condition of the disease and quality of drinking water as risk factors for intestinal parasitic infections (9).
In this study, diarrhea rate was high in patients with intestinal infections. However, we cannot clearly attribute diarrhea to the type of pathogen in HIV-positive patients; rather neuronal and gastrointestinal dysfunctions in HIV-positive individuals may be responsible for diarrhea in these patients. In Zali et al. (16) study, the incidence of diarrhea in HIV-positive patients has been reported as 53.6%, which is lower than the results in the present study. Contrary to the claim that HIV infection increases the risk of intestinal parasitic infections, the results of Nilsson et al. studies (2006, 2007) denied it as the HIV-positive individuals rather than HIV-negative people develop behaviors related to personal hygiene (25, 26).
According to the results, Cryptosporidium parasite has been found more common in people under 30 years old, the illiterates, and self-employed people showing that they are at higher risk for intestinal parasitic infection. In a study by Tian et al. (2012), age has been reported as a factor influencing the incidence of gastrointestinal parasitic infections. According to the study, young people under the age of 42 are more susceptible to parasitic infections, which is consistent with our results (27). Therefore, the focus of health, treatment, prevention, and health promotion should be on this group of people. Akinbo study showed that the job of HIV-positive patients affects the rate of intestinal parasitic infections. Artisans, farmers, and most police forces drink and eat from the contaminated sources because they have more access to such sources. Thus, higher prevalence of parasitic infections has been reported in this group. Also, in illiterates, the prevalence of intestinal parasites has been reported as 47.37% (6).
In general, parasitic infections are an important cause of morbidity and mortality in developing countries, particularly among HIV-positive individuals (6). Factors such as employment, health status, education, and age affect the incidence of parasitic infections. Performing screening tests, identifying those infected with virus and prescribing appropriate medications are among the most important measures to control communicable diseases for all patients, especially HIV-positive people and AIDS patients. In general, performing routine fecal tests for detection of intestinal parasites is particularly useful for HIV-positive patients and individuals with weakened immune systems. The results of these tests can reduce mortality and morbidity rates and increase people's quality of life. Therefore, the need for doing periodic parasitological tests is recommended for all people with HIV.
Unfortunately, the exact number of sufferers of HIV infection in Ahvaz was not available, and the study samples included only those referred to health centers for treatment and receiving drugs with special case files. Certainly, there are many people in society infected with the HIV virus, and unfortunately unaware of their illness. Most people go into diagnostic centers long after they have been infected, and naturally, due to a weakened immune system; not much can be done to cure or control the diseases of these people, which accounts for the limitations of our study too.
Providing samples from HIV-positive patients are difficult. Respecting and protecting the confidentiality of patient information is an absolute priority. Many people had not yet given sample container. Access to patients' medical records in terms of ethics was very difficult too.
The overall prevalence of intestinal parasites was 48.5%; so the high prevalence of intestinal parasites in HIV-positive patients indicates weakened immune systems and a higher susceptibility to the development of gastrointestinal parasites, in particular opportunistic parasites. Thus, performing routine tests of stool for diagnosis of intestinal parasites is recommended for those with weakened immune systems.