1. Background
Nonalcoholic fatty liver disease (NAFLD) is one of the most common causes of chronic liver disease in western countries characterized by accumulation of fat in liver cells in the absence of excessive alcohol consumption (1, 2). It includes simple steatosis, which can progress to nonalcoholic steatohepatitis (NASH). NASH can progress to cirrhosis and liver cancer. With increasing the prevalence of obesity, the impact and prevalence of NAFLD is increasing, thus in the coming decades, NASH would be the most common cause of advanced liver disease (3). Studies have shown that liver-related mortality in patients with nonalcoholic fatty liver was higher in patients with NASH than those without it (4). Many risk factors are involved in increased prevalence of fatty liver. According to previous studies, central obesity, type II diabetes, hyperlipidemia and hypertension are some of known risk factors of NAFLD (5). Prevalence of overweight and obesity is increasing and takes the place of smoking as the leading cause of preventable morbidity and mortality (6). The American Medical Association considered obesity as a disease. Obesity leads to fat deposition in nonadipose tissues called ectopic fat. The liver is one of these tissues and obesity is a major risk factor of NAFLD (7). The prevalence of NAFLD in obese individuals has been reported between 60% and 90% (8) and the mean prevalence of NASH has been reported 33% with a range of 10% to 56% (9). Weight loss is possible by lifestyle changes (behavior therapy) or bariatric surgery. Bariatric surgery is becoming popular with the increasing prevalence of obesity. There is increasing evidence showing that weight loss after bariatric surgery can be helpful for patients with NASH (10). This improvement is associated with a reduction in metabolic parameters and the levels of inflammatory mediators (11). Sleeve gastrectomy also known as the vertical gastrectomy, is a newer bariatric procedure for the treatment of obesity and its related diseases. The sleeve operation is excision of the lateral aspect of the stomach, leaving a reduced tubular stomach (12-14). Although the American Society for Metabolic and Bariatric Surgery (ASMBS) and the American College of Surgeons (ACS) approved the safety of sleeve gastrectomy (15, 16), patients candidates for sleeve gastrectomy have better conditions in comparison of patients candidates for other bariatric methods in Iran (12, 13).
2. Objectives
This study was designed to determine the prevalence of NAFLD in morbidly obese patients undergoing sleeve bariatric surgery in Iran and association of NAFLD existence with other comorbid conditions.
3. Patients and Methods
This was an analytical cross-sectional study approved by Baqiyatallah University of Medical Sciences Ethics Committee (No.32-3, on meeting 2013-07-26). The sample size was calculated using sample size formula [n = Z1-α/2 × P (1-P) / d2]. One hundred and fourteen morbidly obese patients undergoing sleeve gastrectomy by a single surgeon in Baqiyatallah hospital in April 2013 to September 2014 were included. Patients were enrolled using simple random sampling method. Non-morbid obese patients and those with other indications for sleeve gastrectomy were not included. Liver ultrasonography was performed for all patients before the operation. NAFLD was diagnosed and its grade was determined using abdominal ultra-sonography by seeing hyperechoic texture or a bright liver and fatty infiltration and liver enzymes (17, 18). All sonographies were performed by two expert sonographists in Baqiyatallah Hospital sonography ward and inter observers reliability of variables did not have any significant difference. Prevalence of NAFLD and its association with other comorbid conditions (e.g. diabetes mellitus, hyperlipidemia, hypertension, hypothyroidism and ischemic heart disease) were evaluated. Patients with known alcohol consumption, having a mean corpuscular volume of red cells > 100 fl, and those with chronic hepatic disease were excluded from the study.
3.1. Statistical Analysis
Data was analyzed using statistical package for social sciences (SPSS) version 18 (SPSS Inc. Chicago, IL, USA) for windows. Data was reported using mean ± SD, number and percentage. Patients with and without NAFLD were compared together using independent sample T-test, Mann-Whitney U test (in case of non-normal distribution variables) and Chi square test. Normal distribution of variables was approved by one-sample Kolmogorov-Smirnov test.
4. Results
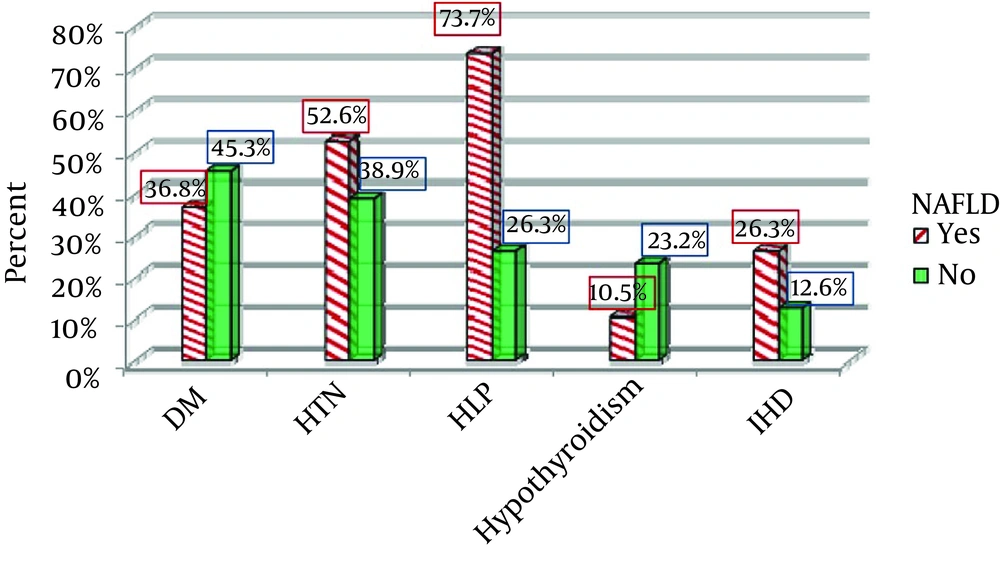
One hundred and fourteen patients with a mean age of 33.96 ± 9.92 years were included (48 males and 66 females). The prevalence of NAFLD was 16.7% (9 patients grade one, 4 patients grade two and 6 patients grade three). The mean BMI was 43.61 ± 5.77 kg/m2. Fifty patients (43.9%) had diabetes mellitus, 39 patients (34.2%) hyperlipidemia, 47 patients (41.2%) hypertension, 24 patients (21.1%) hypothyroidism and 17 patients (14.9%) ischemic heart disease. Comparison of characteristics, comorbid conditions and laboratory findings of patients with or without NAFLD are shown in Table 1. Comparison of comorbid conditions prevalence in patients with and without NAFLD is shown in Figure 1. The mean BMI was 43.21 ± 4.09 kg/m2 in patients with NAFLD and 43.7 ± 6.09 kg/m2 in patients without it (P = 0.759). The mean BMI was 44.23 ± 6.88 kg/m2 in patients with diabetes and 43.15 ± 4.77 kg/m2 in those without it (P = 0.383). The mean BMI was 43.53 ± 4.8 kg/m2 in patients with hypertension and 43.67 ± 6.41 kg/m2 in those without it (P = 0.912). The mean BMI was 44.23 ± 5.89 kg/m2 in patients with hyperlipidemia and 43.26 ± 5.72 kg/m2 in those without it (P = 0.444). The mean BMI was 44.08 ± 5.95 kg/m2 in patients with hypothyroidism and 43.46 ± 5.75 kg/m2 in those without it (P = 0.668). The mean BMI was 46.61 ± 4.83 kg/m2 in patients with ischemic heart disease and 43.11 ± 5.79 kg/m2 in patients without it (P = 0.042).
| Variables | NAFLD (+) (n = 19) | NAFLD (-) (n = 95) | Total (n = 114) | P Value |
|---|---|---|---|---|
| Age, y | 36.58 ± 8.52 | 33.41 ± 10.15 | 33.96 ± 9.92 | 0.208 |
| Male gender | 10 (52.6) | 38 (40) | 48 (42.1) | 0.309 |
| Weight, kg | 129.13 ± 28.74 | 121.86 ± 24.06 | 123.16 ± 24.93 | 0.293 |
| Height, cm | 171.88 ± 16.56 | 166.74 ± 12.4 | 167.66 ± 13.27 | 0.162 |
| Body Mass Index, kg/m2 | 43.21 ± 4.09 | 43.7 ± 6.09 | 43.61 ± 5.77 | 0.759 |
| Systolic Blood Pressure, mmHg | 125.32 ± 12.04 | 117.85 ± 12.28 | 119.12 ± 12.51 | 0.017 |
| Diastolic Blood Pressure, mmHg | 75.0 ± 9.72 | 72.22 ± 8.71 | 72.69 ± 8.91 | 0.216 |
| Diabetes Mellitus | 7 (36.8) | 43 (45.3) | 50 (43.9) | 0.499 |
| Hyperlipidemia | 14 (73.7) | 25 (26.3) | 39 (34.2) | < 0.001 |
| Hypertension | 10 (52.6) | 37 (38.9) | 47 (41.2) | 0.269 |
| Hypothyroidism | 2 (10.5) | 22 (23.2) | 24 (21.1) | 0.335 |
| Ischemic Heart Disease | 5 (26.3) | 12 (12.6) | 17 (14.9) | 0.157 |
| Hospital Stay, days | 1.21 ± 0.54 | 2.17 ± 1.41 | 2.01 ± 1.37 | 0.004 |
| White Blood Cell, 103/mm3 | 10.53 ± 3.12 | 10.18 ± 3.4 | 10.24 ± 3.34 | 0.699 |
| Red Blood Cell, 106/mm3 | 5.03 ± 0.73 | 4.74 ± 0.47 | 4.79 ± 0.53 | 0.050 |
| Hemoglobin, mg/dL | 14.26 ± 2.45 | 13.15 ± 1.49 | 13.31 ± 1.7 | 0.018 |
| Hematocrit | 42.57 ± 6.27 | 39.38 ± 4.41 | 39.86 ± 4.83 | 0.018 |
| Platelet | 237.59 ± 44.3 | 262.77 ± 61.63 | 258.44 ± 59.59 | 0.113 |
| Fasting Blood Sugar, mg/dL | 99.58 ± 24.53 | 119.32 ± 46.27 | 116.03 ± 43.95 | 0.074 |
| BUN, mg/dL | 12.56 ± 3.01 | 14.08 ± 3.83 | 13.77 ± 3.71 | 0.146 |
| Creatinine, mg/dL | 0.931 ± 0.22 | 0.896 ± 0.13 | 0.902 ± 0.15 | 0.395 |
| Triglyceride, mg/dL | 185.09 ± 73.31 | 136.39 ± 51.15 | 143.73 ± 57.19 | 0.008 |
| Total Cholesterol, mg/dL | 164.79 ± 22.48 | 168.31 ± 41.68 | 167.48 ± 37.95 | 0.726 |
| HDL, mg/dL | 42.94 ± 11.85 | 48.32 ± 11.98 | 47.15 ± 12.09 | 0.087 |
| LDL, mg/dL | 127.29 ± 35.56 | 118.23 ± 30.43 | 120.21 ± 31.63 | 0.272 |
| Alanine Aminotransferase, U/L | 54.16 ± 49.58 | 23.07 ± 5.77 | 32.02 ± 30.09 | < 0.001 |
| Aspartate Aminotransferase, U/L | 65.84 ± 23.72 | 45.61 ± 12.23 | 51.44 ± 22.08 | < 0.001 |
| Alkaline Phosphatase | 181.21 ± 59.68 | 94.0 ± 58.86 | 119.11 ± 70.86 | < 0.001 |
| Sodium, mEq/L | 137.42 ± 3.4 | 135.9 ± 4.37 | 136.19 ± 4.22 | 0.267 |
| Potassium, mEq/L | 4.18 ± 0.3 | 3.94 ± 0.4 | 3.98 ± 0.39 | 0.048 |
5. Discussion
The prevalence of NAFLD among patients undergoing sleeve surgery was 16.7%, which is higher than the value reported in Harnois et al. study (19). Although some previous studies reported a higher prevalence, general prevalence of NAFLD in patients undergoing bariatric surgery was reported between 2.6% and 91% (20-25). The gold standard to diagnose and grading NAFLD and NASH is liver biopsy (18, 26). However, due to its invasive nature, is not performed routinely for NAFLD screening in Iran (18). However, age, gender, BMI and other risk factors may be involved in the dispute. Fatty liver prevalence increases with age, while patients undergoing sleeve surgery in this study were younger than previous studies, and their mean age was 34 years. In this study, no significant differences were observed between obese patients with and without NAFLD regarding age, gender, weight, height, body mass index, diabetes, hypertension, cardiovascular disease and hypothyroidism, but this difference was significant for hyperlipidemia. Some of these findings are consistent with previous studies and some are inconsistent with previous studies (Table 2). It is recommended to perform diagnostic gold standard (liver biopsy during the operation) to determine the exact prevalence of NAFLD and NASH in patients undergoing sleeve surgery. It is also recommended to assess the impact of sleeve surgery on fatty liver in short-term and long-term in further investigations. A high prevalence of diabetes, hyperlipidemia, hypertension and hypothyroidism was observed in these patients; thus, it is recommended to examine the effects of surgery in controlling comorbid conditions in short-term and long-term.
| Study, Year | BMI | Mean Age | Male, % | Sample Size | Kind of Surgery | Diagnostic Method | NAFLD/ NASH Prevalence, % | Related Factors | Not-Related Factors |
|---|---|---|---|---|---|---|---|---|---|
| Spaulding et al. (23), 2003 | 51 | Not clear | 16 | 48 | Roux-en-Y gastric bypass (RYGBP) | Biopsy | 56 | DM, Abnormal LFT | Central Obesity, Gender, HLP, HTN |
| Moretto et al. (22), 2003 | 48.1 | 36.1 | 24.7 | 77 | Bariatric Surgery (undefined) | Biopsy | 2.6 NASH, 83.1 Steatosis | HLP, DM | BMI |
| Boza et al. (27), 2005 | 42 | 40 | 38 | 127 | Bariatric Surgery (undefined) | Biopsy | 26 | Female, Type 2 DM, HDL, AST, ALT, Insulin resistance, Metabolic syndrome | BMI, Age, HTN, Chol, LDL, TG |
| Harnois et al. (19), 2006 | 45.7 | 38 | 8 | 92 | Laparoscopic Gastric Bypass/Laparoscopic gastric band | Biopsy | 9.8 | BMI, Chol, TG | Gender, Age, Waist/ Hip Ratio, DM, HTN, FBS, ALT, AST |
| Feijo et al. (28), 2013 | 44.2 | 38.4 | 27 | 60 | Gastric bypass | Biopsy | 66.7 | γGT | Age, Gender, DM, BMI, Waist, HDL, TG, Uric Acid, LFT, Ferritin |
| Holterman et al. (29), 2013 | |||||||||
| Adolescents | 52 | 16 | 21 | 24 | Gastric Banding | Biopsy | 87.5 | Not clear | Not clear |
| Adults | 51 | 38 | 12.5 | 24 | Gastric Banding | Biopsy | 50 | Not clear | Not clear |
| Present study | 43.6 | 34 | 42.1 | 114 | Sleeve Bariatric Surgery | Sonography | 16.7 | SBP, HLP, Hgb, Hct, TG, LFT, Potassium | Age, Gender, Weight, Height, BMI, DBP, DM, HTN, Hypothyroidism, IHD, WBC, RBC, Plt, FBS, BUN, Cr, Chol, HDL, LDL, Na |
Comparison of Our Study With Previous Studies Showing NAFLD and NASH Prevalence and Association With Other Comorbid Conditions a
Ultrasound method was used in our study, which is a routine method for NAFLD screening in Iran and it was one of the limitations of the present study. Another limitation was the small sample size, because of small number of bariatric surgery with sleeve method in Iran and prospective structure of our study. We selected patients undergoing sleeve bariatric surgeries because of special conditions of these patients compared to other bariatric methods (e.g. younger age).
This is the first study reporting the prevalence of NAFLD in patients undergoing sleeve gastrectomy in Iran. Despite using ultrasonography instead of gold standard (liver biopsy) for diagnosis of NAFLD, our study showed an almost high prevalence of NAFLD in morbidly obese patients undergoing sleeve gastrectomy in Iran. We suggest using the gold standard diagnostic method (liver biopsy) to determine the exact NAFLD prevalence and evaluate the impact of sleeve surgery on NAFLD in short and long term follow-up.