1. Background
Depressive disorders and symptoms often occur in women, especially in middle age, when about 8% to 40% women develop symptoms. Puberty onwards, women are 1.5 to 3 times more likely than men to develop depressive disorders. Although at present there are differences of opinion in the literature, the pre- and peri-menopause phases were previously considered periods of high vulnerability to depression (1). Psychological problems, particularly depression, are one of the major problems affecting postmenopausal women in many communities. The prevalence of depression, the most common mood disorder (sometimes called psychological flu), is reportedly 43% during menopause (2). According to available statistics, approximately 15% - 20% adults suffer from depression. The condition is prevalent among 7.7% of the population aged 15 years and over in our country (3, 4). Anxiety is seen in 5% - 15% of the population and is two to three times more likely to affect women. A study performed by Sagzoz et al. using the beck depression inventory (BDI) showed that depression and anxiety can increase in postmenopausal women (5).
Menopause, defined as the permanent cessation of menstruation, is only one aspect of the climacteric period (6) that, according to the world health organization (WHO) definition, is clinically characterized by amenorrhea for at least 12 continuous cycles (6). From the viewpoint of laboratory findings, it indicates the cessation of menstruation that is associated with a reduction in estrogen levels and an increase of over 40 mm units per liter in the levels of follicle stimulating hormone (FSH) (5).
Although the mean age of postmenopausal women is 51 years, 4% women may experience natural menopause before age 40 (7). According to a study in 1982, the average age of menopause in Iran was 50.4 years (8), while in a study by Nouhjah et al. (9), it was found to be 47.97 years in the city of Ahvaz.
During menopause, some women experience numerous and severe symptoms, while others experience minor or no symptoms. The nature and prevalence of menopausal symptoms are common in most women. The differences in menopausal symptoms between cultures are not a reflection of physiological status; rather, they occur due to differences in the communities and the amount that individuals understand the world. In the perimenopausal years, different ethnic groups show negligible difference in hormone levels, which is mainly caused by differences in body size (6).
During the menopausal transition, the level of reproductive estrogen (17-beta-estradiol) is reduced from 250 - 100 pg/mL to less than 10 pg/mL. Therefore, the ability to saturate the receptors and stimulate the targeted tissue cells disappears, leading to estrogenic dysfunction. The symptoms associated with estrogen deficiency, which occur during or after menopause, include hot flashes, night sweats, insomnia, and vaginal dryness. There are other symptoms and conditions that are not necessarily related to estrogen deficiency: abnormal bleeding, osteoporosis, arteriosclerosis, dyslipidemia, depression, irritability, headache, amnesia, dry mouth, eyes, reduced skin elasticity, and muscle and joint pain (10).
Women who are in natural early menopause before age 40 may experience a more significant reduction in estrogen levels and ovarian function, compared to women with later menopause. In a study by Liao et al. (2000), 74% women with premature menopause were classified as depressed people, who may face negative cultural attitudes such as being branded infertile (1).
Dolatian et al. (2) reported the prevalence of depression to vary from 28% - 36%, with the highest and lowest levels observed in both pre and peri menopausal women.
Elucidation of the role of depression during different stages of menopause (peri- vs. post) is of clinical relevance, given its serious consequences for health and cognition. Menopausal symptoms, including depression, greatly influence well-being and quality of life (11). In addition, depression is associated with other chronic diseases, including metabolic syndrome, osteoporosis, cardiovascular disease (12), and reduced cognitive functioning (13). With increasing life expectancy, women spend approximately a third of their life in menopause, and depressed patients need special care and high costs of health care.
2. Objectives
This study aimed to determine the relationship between depression and the variables of menopausal symptoms, age, and body mass index (BMI). If found, such correlations may require appropriate measures to control or prevent depression.
3. Patients and Methods
This descriptive-analytical study was performed with convenience sampling on 250 postmenopausal women who were referred to health centers in Ahvaz from October to December 2012. By using the following formula with a ratio of P = 0.5 and 95% confidence interval, the sample size was estimated at 195 patients according to the estimated d = 0.07, which was increased to 250 people because of the risk of sample loss.

Due to the high population covered by the centers, non-probability convenient sampling was used in this study in two main healthcare centers in the East and West of Ahvaz. Relatively healthy postmenopausal women, aged 45 - 70 years, who had at least one year of normal amenorrhea (without surgery to remove the uterus and ovaries), were included in the study. Exclusion criteria were: debilitating physical diseases, any hormone therapy in the past 6 months, drug use and smoking, any mental illness in the immediate family members and the patient, the use of psychotropic medications, anticonvulsants, narcotic drugs, experience of some stress (such as a spouse’s betrayal, death, serious illness, or prison sentence of close relatives in the past year). The study was conducted with own funds.
At the beginning of the study, consent of all the women for participation was obtained after the project was described. After that, their blood pressure, height, and weight were measured. Data collection instrument was an inventory consisting of two parts (personal information questionnaire and questions of the study), for which we used the standard BDI and the menopause rating scale (MRS) questionnaire.
The personal information questionnaire was prepared after reading the latest books and research papers, and its content validity was confirmed by a number of experienced professors in this area. The BDI is one of the most suitable instruments to assess depression, with two long and short forms. The long form of the BDI, which was used in the study, consists of 21 items to measure somatic, behavioral, and cognitive symptoms of depression. Each item has 4 options scored from 0 to 3, which determines the varying degrees of depression, from mild to severe. The maximum and the minimum scores in the inventory are 63 and 0, respectively. The score obtained from the total items of the BDI is interpreted in this manner, that we considered the total score of 0 - 10 as natural (or non-depressed), 11 - 16 as mild depression, 17 - 30 as moderate depression, 31 - 40 as severe depression, and more than 40 as extreme depression. Reliability and validity of the BDI have been reported in several cases, with the internal consistency found between 0.48 and 0.86 (14).
To evaluate menopausal symptoms, we also used the MRS a standard international scale that examines menopausal symptoms, based on extensive studies of factor analysis, and uses numerous questions about the evaluation of different menopausal symptoms (15, 16). The standardized inventory (MRS) examines menopausal symptoms in three areas, including 11 items in total: 1) somatic symptoms (hot flashes, heart failure, sleep disturbance, and joint and muscular problems); 2) psychological symptoms (depressed mood, irritability, anxiety, physical and mental fatigue); and 3) urogenital symptoms (sexual problems, vaginal dryness, and bladder problems) (17). Depending on the severity of symptoms expressed subjectively by the patient, each item was scored between 1 (no symptom) and 5 (very severe) on the point Likert scale. After the scores of each item were gathered together, the score for each sub-group and overall score were calculated. The total scores of the MRS questionnaire ranged from 11 to 55. The higher overall MRS score or score for each area (or questions of that area), the higher severity of experienced menopausal symptoms.
First, written consent was obtained from the participants after detailed explanations of the researcher on the design objectives and confidentiality of information about each subject. Then, the personal characteristics and the results of measurement of height, weight, blood pressure, etc. were collected in the inventory, and the subjects were asked to complete the BDI and MRS, by examining their physical and mental condition during the prior month.
3.1. Statistics
SPSS 17.0 software was used for analyzing data. The data obtained were analyzed by using descriptive statistics, Pearson and Spearman correlation coefficients, chi-square, and ANOVA.
4. Results
According to the findings of the study, which was performed on 250 people, the mean age and the mean age at menopause of the participants in the study were 58.81 ± 6.66 and 48.86 ± 7.19 years, respectively; the mean BMI was 29.12 ± 5.12 kg/m2. The majority of participants in the study were married (69.6%) with 5 ± 2.7 children and housewives (89.7%), with education up to the primary school level (42.1%) (Table 1).
| Parameters | Frequency (n = 250) |
|---|---|
| Age Group, y | |
| 45 - 49.9 | 29 (10.3) |
| 50 - 54.9 | 40 (15) |
| 55 - 59.9 | 58 (23.8) |
| 60 - 64.9 | 64 (26.6) |
| 65 - 70 | 59 (24.3) |
| Body Mass Index, kg/m2 | |
| 19.8 > | 11 (0.9) |
| 19.8 - 26 | 43 (15.9) |
| 26 - 29 | 113 (48.6) |
| 29 < | 83 (34.6) |
| Educational Level | |
| Uneducated | 79 (32.7) |
| Primary school level | 99 (42.1) |
| Secondary school level | 55 (21.5) |
| Collegiate | 17 (3.7) |
| Occupation | |
| Housewife | 194 (90.6) |
| Practitioner | 21 (9.4) |
| Smoking | |
| Smoker | 23 (2.3) |
| Non-smoker | 227 (97.6) |
| Exercises | |
| Yes | 65 (22) |
| No | 185 (78) |
Frequency Distribution of Personal Characteristics of the Participants in the Study a
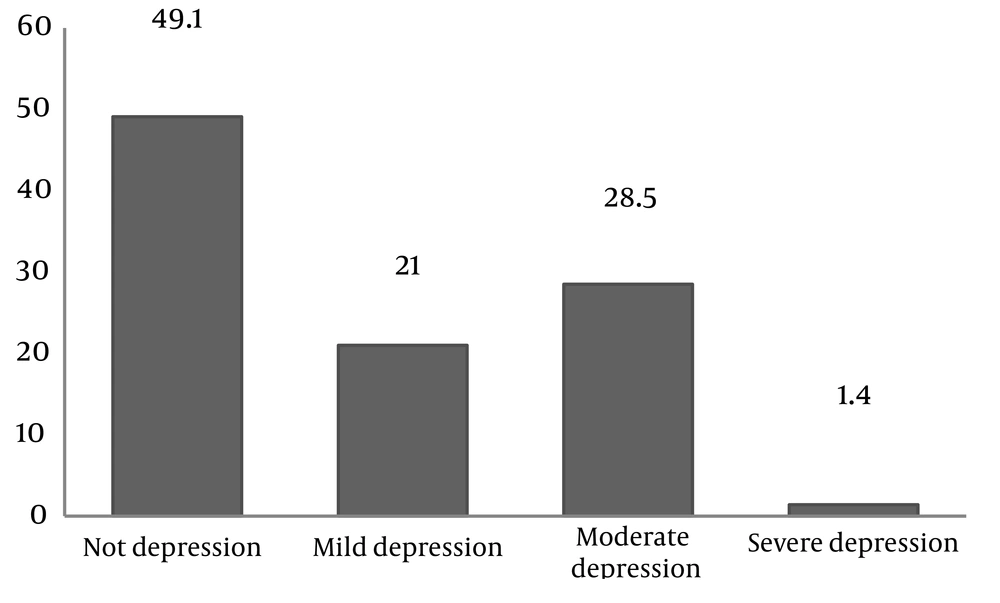
The study results showed that the mean score of depression was equal to 11.43 ± 8.64: 21% with mild depression, 28.5% with moderate depression, and 1.4% with severe depression (Figure 1).
The average overall MRS score in the study was 13.04 ± 8.01, and the highest score was related to the area of somatic health, with an average of 5.48 ± 3.28 (Table 2). However, the highest complaints associated with menopause were related to muscle and joint problems (1.86 ± 1.38), irritability (1.42 ± 1.31), and sleep disturbance (1.4 ± 1.26). By using the Pearson correlation test, a significant relationship was observed between depression and MRS in all the three areas (P > 0.001).
| Parameters | Mean ± SD |
|---|---|
| Somatic | 5.48 ± 3.28 |
| Psychological | 5.08 ± 4.03 |
| Urogenital | 2.48 ± 2.34 |
| Total MRS | 13.04 ± 8.01 |
Score of Menopausal Symptoms According to the MRS Scale in Terms of Subscales
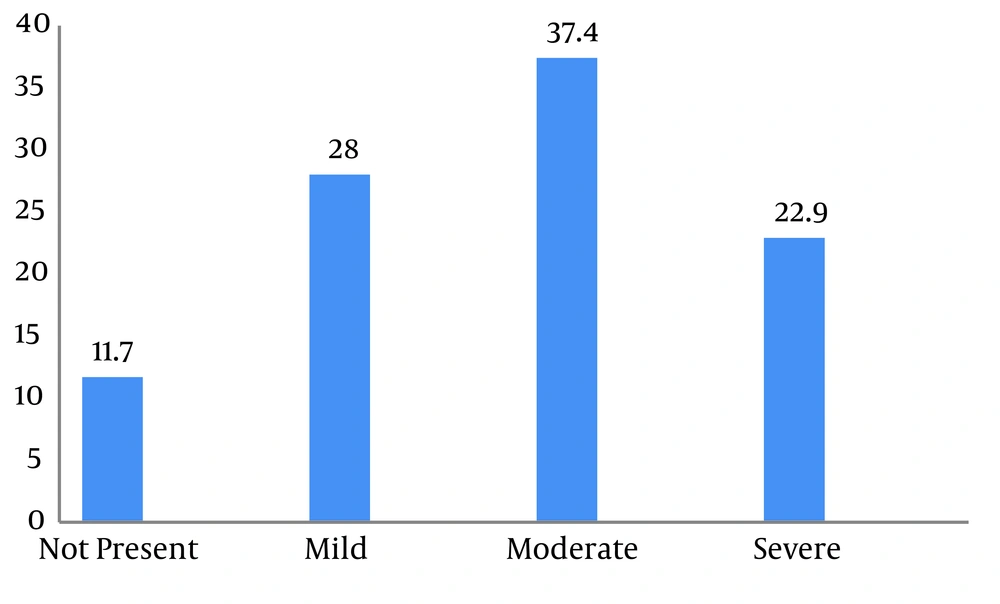
The ANOVA results for the relationship between depression and menopausal symptoms showed a significant statistical difference observed in the mean score of depression at different levels of menopausal symptoms (P < 0.05), except for heart failure, decreased libido, sexual satisfaction, as well as vaginal dryness and burning, in which it was not statistically significant (P > 0.05) (Table 3). Overall, menopausal symptoms were mild in 28% women, moderate in 37.4%, and severe in 22.9% (Figure 2).
The results showed that although using Pearson correlation test, there is no significant relationship between depression and the variables of age of women, age at menopause, BMI, and abdomen and waist circumference (P > 0.05). However, a significant relationship was observed (using ANOVA) between education level and depression (P < 0.001) women with a higher level of education had a lower mean score of depression.
| Parameters | Not Present | Mild | Moderate | Severe | Very Severe | P Value |
|---|---|---|---|---|---|---|
| Somatic | ||||||
| Hot flushes | 7.15 ± 9.19 | 11.4 ± 9.49 | 13.06 ± 8.33 | 15.11 ± 8.03 | 12.73 ± 13.04 | P < 0.01 |
| Heart discomfort | 11.05 ± 7.82 | 10.02 ± 10.39 | 11.6 ± 8.5 | 17.25 ± 7.84 | 15.2 ± 8.67 | P = 0.06 |
| Sleeping problems | 7.92 ± 5.52 | 11.13 ± 8.43 | 12.16 ± 8.82 | 16.95 ± 11.71 | 17.05 ± 8.8 | P < 0.001 |
| Muscle and joint problems | 8.98 ± 6.96 | 10.57 ± 9.05 | 11.2 ± 9.36 | 11.7 ± 8.94 | 16.89 ± 7.43 | P < 0.003 |
| Psychological | ||||||
| Depressive mood | 8.38 ± 5.92 | 11.87 ± 10.64 | 13.09 ± 9.53 | 17.54 ± 8.58 | 15.63 ± 8.24 | P < 0.001 |
| Irritability | 8.4 ± 6.53 | 8.24 ± 9.15 | 13.38 ± 8.11 | 16.71 ± 12.09 | 18.33 ± 6.59 | P < 0.001 |
| Anxiety | 7.72 ± 5.89 | 12.81 ± 8.3 | 12.98 ± 9.32 | 16.5 ± 9.99 | 21.5 ± 13.3 | P < 0.001 |
| Physical and mental exhaustion | 8.92 ± 7.44 | 12 ± 8.02 | 11.88 ± 9.89 | 14.9 ± 9.21 | 15.2 ± 7.37 | P < 0.007 |
| Urogenital | ||||||
| Sexual problems | 11.89 ± 7.77 | 10 ± 10.74 | 11.37 ± 8.52 | 9.87 ± 9.37 | 13.66 ± 12 | P = 0.709 |
| Bladder problems | 10.45 ± 8.06 | 8.23 ± 8.74 | 14.54 ± 7.96 | 17.2 ± 8.28 | 18 ± 11.31 | P < 0.001 |
| Dryness of the vagina | 11.1 ± 8 | 11.72 ± 7.45 | 10.89 ± 10.45 | 16.87 ± 13.63 | 17.66 ± 9.23 | P = 0.284 |
Evaluation of the Mean Score of Depression in Terms of the Severity of Menopausal Symptoms in the Women Studied
5. Discussion
According to the results of the present study, a significant relationship was observed between depression and menopausal symptoms. The same relationship was observed in a study by Chedraui et al. (18) and Reed et al. (19). Freeman et al. (20) also found similar results that were consistent with the findings of this study. However, conflicting results were observed in the study of Bahri et al. (21) which reported no significant relationship between the severity of menopausal symptoms and the two variables of depression and anxiety.
In addition, according to the results of this study, a significant correlation was observed between depression and many areas of menopausal symptoms, including hot flashes, sleep disturbance, muscle pain, feelings of depression, irritability, anxiety, loss of memory, and urinary incontinence. Karaoulanis et al. (22) found a significant relationship between depression and hot flashes, concluding that depressed premenopausal women experience higher severity and frequency of hot flashes than did healthy premenopausal women. In addition, the results of a study by Melby et al. (23) showed that women with moderate to severe depression had more complaints of vasomotor symptoms than those without depression or with mild depression. Shogaeean et al. (3) reported conflicting results, suggesting that there is no statistically significant relationship between hot flashes and depression. Ozturk et al. (24) reported no statistically significant relationship between vasomotor symptoms and the severity of depression, which was consistent with the results of the study by Shogaeean et al. (3).
Depression leads to irregular sleep patterns; the sleep-wake pattern may change in menopause as well (25). The domino theory presents the hypothesis that sleep disorders act as mediator between vasomotor symptoms and mood problems. In other words, vasomotor symptoms cause sleep disturbances, which in turn leads to negative mood (26). In the present study, a significant relationship was found between depression and sleep problems. Brown et al. (27) also showed a statistically significant relationship between frequent nocturnal insomnia and higher scores of depression. Lampio et al. (28) also concluded that depressive symptoms can cause sleep disorders, regardless of whether the patient is perimenopausal or menopausal. In connection with the other menopausal symptoms, Tarverdy and Shabani (4) found a significant relationship between the mean score of depression in terms of whether symptoms such as bone pain, headache, numbness of fingers, as well as urinary incontinence and burning are present. In a study by Bosworth et al. (29), a significant relationship was found between depression and menopausal symptoms in women, the results of which were consistent with the results of this study. However, conflicting results were found in the study by Shogaeean et al. (3) that showed no significant relationship between the mean score of depression and symptoms such as bone pain, headache, numbness of fingers, and urinary incontinence and burning.
Longitudinal studies have clearly shown that people with symptoms of severe depression or a history of major depressive disorder are more likely than non-depressed individuals to experience cardiovascular events (30). In other words, hormonal changes during the menopausal transition can be involved in the worsening of cardiovascular events (31). Llaneza et al. (13) also concluded that women with a severe depression are at higher risk of cardiovascular events with poor cognitive function than non-depressed women. The non-significant relationship between depression and heart failure in the present study can be attributed to the low prevalence of severe depression in the study population.
Sexual dysfunction in women is a multifactorial and multidimensional disorder, consisting of sexual, physical, physiological, and psychological causes. Reduction in sexual pleasure or decreased libido, as one of its first symptoms, had a high prevalence in the general population of women (32). In the study by Jonusiene et al. (33), the main risk factors for the onset of sexual dysfunction were reported to be depression, anxiety, menopausal symptoms, and age. Avellanet et al. (32) also showed that depression symptoms and signs were significantly associated with decreased sexual pleasure. In the present study, no significant relationship, however, was found between the mean score of depression and the two variables of decreased libido and sexual satisfaction. Shogaeean et al. (3) also observed no significant relationship between depression score and decreased libido. In addition, Zhou et al. (34) found similar results, suggesting no significant relationship between depression and the variables of age of women, duration of menopause and BMI. Whereas Bosworth et al. (35) reported no difference in the proportion of depressed to non-depressed women in terms of age, Dolatian et al. (2) concluded that age is directly proportional to depression in all phases of pre-, peri- and post-menopause. In addition, Rasooli et al. (2004) showed that the severity of anxiety and depression are not affected by the duration of menopause and BMI (5), which is consistent with the results of this study. However, Woods et al. (36) reported a significant relationship between BMI and depression. Along with obtaining similar results, Sternberg and Lee (37) also stated that high BMI is associated with the prevalence of depressive symptoms.
In the present study, a significant relationship was observed between education level and depression; women with a higher level of education had a lower mean score of depression. Dolatian et al. (2) also concluded that the level of depression decreases with increase in the education level of individuals. Kakkar et al. (38) also found similar results, which is consistent with the results of this study. However, the conflicting results in the study by Zhou et al. (34) state that women with higher levels of education are more likely to experience depression during menopause.
One strength of the present study was the use of MRS as an internationally valid scale to assess menopausal symptoms. Face to face interviews were also used in this study to complete the inventories, which minimizes the likelihood of error in completing the inventories.
The use of face to face interviews is also a limitation of this study, because the researchers had to rely on what the subjects answered about the severity of symptoms during the past month.
Depression was observed with a high prevalence of 50% in the study. A significant relationship was noted between menopausal symptoms and the severity of depression, which means that the latter can increase with increasing menopausal symptoms. Thus, necessary measures are suggested for the diagnosis and treatment of menopausal symptoms to reduce the problems of depression.