1. Background
The chronic nature of diabetes and the development of new treatments that improve patients’ longevity can increase the risk of chronic complications, which, in turn, can lead to numerous problems for patients with diabetes and impose a heavy economic burden on a country’s health care system (1). Among the numerous complications of diabetes, which are increasing and thereby requiring more urgent attention, are foot problems such as foot ulcers or infections and lower limb amputations resulting from non-compliance with safety and prevention methods (2). Research on finding clear and practical solutions for preventing and reducing amputations due to diabetes has shown that health education on foot care is a common strategy for preventing diabetic foot and can prevent lower limb amputation in 85% of those with diabetic foot. (3).
Although the issue of patient education has attracted much attention in recent years in outpatient care centers, there are considerable differences in how such patient education is defined, how to implement it, and the qualifications of the people who provide such services. Because of such ambiguity, patient education is often done using stochastic methods (4). Choosing a health training model is the first step towards planning an educational program. Effective health training depends on adept use of the most suited theories and strategies for a given event (5). Indeed, studies have shown that educational programs applying theoretical cognitive frameworks can have a positive effect on intended outcomes. Several of these programs are currently integrated into primary care, but they have not yet been specifically used to educate diabetic patients (6, 7).
The theory of planned behavior (TPB) is a behavior change model proposed in 1985 and formally developed in 1991 by Ajzen and Fishbein (8). It is an interpersonal theory focusing on factors such as knowledge, attitudes, beliefs, self-concept, mental history, past experience, motivation, skills, and behavior (4). According to the theory, a behavior intention (i.e., thinking about engaging in a behavior) is generated from an attitude toward the related behavior (i.e., positive or negative evaluations of performing the behavior); this attitude is composed of two sub-structures: behavioral beliefs (i.e., a person’s subjective belief that the intended result will be achieved by performing the target behavior) and evaluations of the behavior’s outcome (i.e., an explicit evaluative response to the outcome that influences one’s attitude toward the behavior). Subjective norms refer to the perceived social pressure to perform or not perform a target behavior. People often act according to their own perceptions of what others (e.g., friends, family, colleagues) think that they should do. Therefore, their intention to perform a behavior is potentially affected by people with whom they have close relationships. According to this theory, individuals’ subjective norms are their normative beliefs (i.e., beliefs about the expectations of certain reference groups or individuals) combined with the motivation to follow said groups/individuals (i.e., the desire to satisfy them) by performing a target behavior, despite these expectations. Perceived behavioral control (PBC) refers to the extent to which a person believes he/she has voluntary control over a behavior (i.e., whether performing it is done of their own volition) (4, 9). The TPB has been claimed to have potential in developing interventions for behavior change (10). Indeed, White et al. confirmed its efficacy in the design of educational interventions for physical activity targeted at people with type II diabetes (11). Dydarlu et al. have also argued that, since the TPB can be used to predict self-care behavior and physical activity in people with type II diabetes, it could be a suitable basis for educational interventions aimed at promoting such self-care behaviors in these patients (12, 13). On the other hand, a review of diabetes research in Iran suggests that no TPB-based educational interventions with an emphasis on promoting foot care among patients with diabetes have yet been developed.
2. Objectives
This study was designed to evaluate the effectiveness of a TPB-based intervention aimed at foot care among people with type II diabetes; specifically, the TPB was used as a framework when designing such an intervention.
3. Patients and Methods
3.1. Research Environment and Patients
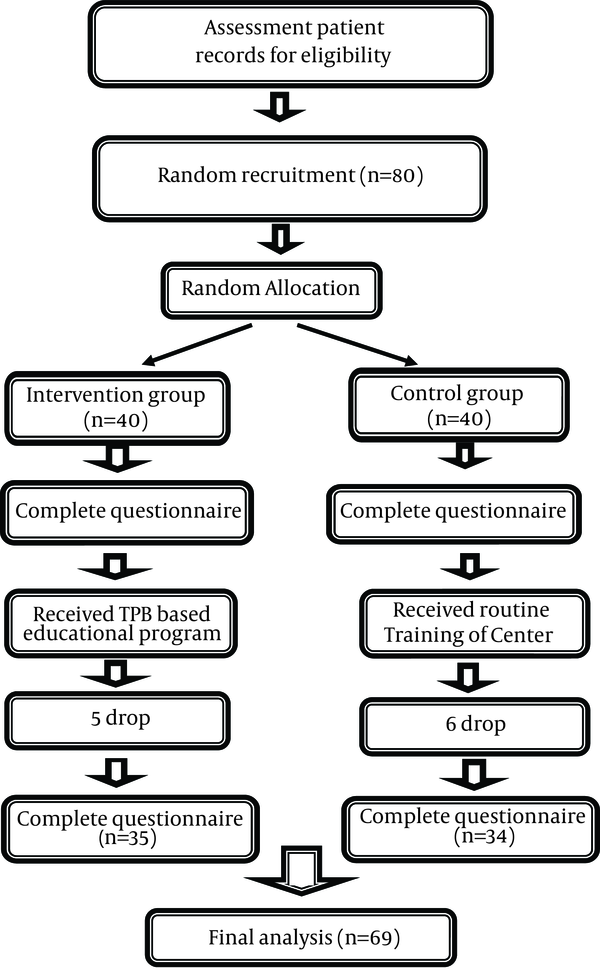
Data were collected from patients with type II diabetes who were referred to the Diabetes Clinic at Ahvaz Golestan Hospital-a major referral center in Iran providing medical and nursing services for patients with type II diabetes in the city of Ahvaz in June-May 2013. The sample size was determined to be 80 people considering the results of a pilot study with 15 participants and a sample size calculation with a proposed 20% dropout rate.
In order to recruit participants, we first checked the medical records of referred patients against the inclusion criteria and prepared a sample list; then, participants were randomly selected using random number generation. Of the approximately 4,000 patients whose medical records were registered in this center, around 1,100 were eligible to participate in the study. The inclusion criteria were as follows: aged 30 - 60 years; residing in the city of Ahvaz; a diagnosis of diabetes for at least 6 months; a lack of diabetic foot ulcers confirmed by the clinics’ physician; no experience of training (except for the routine training of the diabetes center); no history of psychiatric disorders; no history of use of psychotropic drugs; no uncontrolled underlying disease such as a blood pressure over 160/90 mmHg with medication or cardiac or peripheral vascular disorders; and the ability to read and write. Additionally, the exclusion criteria were as follows: failure to participate in any of the training sessions and hospital admission during the study period. Finally, participants were randomly allocated to either the intervention or the control group; each group consisted of 40 participants. The details of the final sample are given in the Results section (Figure 1).
3.2. Intervention
The intervention was designed using the TPB to increase foot care. Participants were selected randomly and divided into two groups (intervention and control). The control group just received the routine training of the center. This routine training consists of a series of educational leaflets and booklets about diabetes and its various treatment methods. These materials contained brief recommendations on foot care.
In contrast, the intervention group took part in a 4-week educational program based on the TPB. The educational content used in the intervention group included information about the causes and risk factors associated with foot ulcers, guidelines that patients with diabetes must be familiar with when caring for their feet, daily foot care activities, positive outcomes of adherence to foot care behaviors, and the negative outcomes of non-adherence. The instructional content was adjusted according to the latest international standards and guidelines, peer-reviewed articles, and books as well as consultations with faculty experts.
The methods of delivering the required educational content in the intervention group included lectures, group discussions, question-and-answer sessions, PowerPoint slides, practical demonstrations of foot care, practicing the demonstrated foot care in the presence of the instructor, and educational booklets. All techniques used in the present study had been identified as potentially benefitting behavioral attitudes, subjective norms, or PBC (14).
After completing a consent form, participants completed a baseline questionnaire before the intervention, which included demographic items, a measure of foot care, and a questionnaire assessing the components of the TPB. Once they had completed the baseline survey, participants in the intervention group were divided into four subgroups, each comprising 10 participants. Each subgroup was then delivered the intervention educational materials in three weekly 60-minute sessions. In the first week, a 60-minute lecture was held for each subgroup, wherein PowerPoint slides containing images of foot care behaviors and complications resulting from non-adherence to these behaviors were shown; additionally, participants were shown how to care for their feet and practiced these behaviors in the presence of the instructor in order to increase their awareness of foot care and to draw their attention to the training program. This session aimed to emphasize the importance of foot care for diabetic patients and improve their emotional preparation to perform and continue these activities. In the second week, the session aimed to create and reinforce positive attitudes and overcome negative attitudes about foot care via group discussion and question-and-answer periods. Participants were asked about their attitudes via questions such as “what is your opinion regarding the effect of diabetes on foot health,” or “does adherence to foot care recommendations provided by physicians and medical staff have positive health effects?” At the end of this session, a booklet including the content presented in the first session was given to participants and they were asked to study it at home. Additionally, in order to manipulate their subjective norms, participants were requested to give the booklet to their family members or anyone caring for them. In the third week, another 60-minute session comprising a question-and-answer period and group discussion was held; this session covered PBC and intention. Participants were asked to talk about their previous successful experiences and their control levels with regard to foot care. Furthermore, they were encouraged to talk about barriers impeding foot care activities. Ultimately, participants were presented with possible strategies for removing these barriers and were encouraged to specify the objectives and actions for overcoming them. No session was held in the fourth week. At the end of the fourth week, all participants were asked to complete the follow-up questionnaire. This questionnaire comprised second administrations of the foot care behavior measure and TPB questionnaire.
3.3. Questionnaire
3.3.1. TPB Questionnaire
A self-designed questionnaire was used to assess behavioral intention, attitude, subjective norms, and PBC. The questionnaire was designed using the guidelines for TPB questionnaire construction (15, 16). Behavioral intention, attitude, subjective norms, and PBC were all assessed using this 34-point scale at baseline and follow-up. Behavioral intention for foot care was measured using four items, each relating to the individual’s plans and intentions regarding future foot care performance (e.g., “I plan to perform foot care each day from tomorrow”; answers ranged from “strongly disagree” to “strongly agree”). Consistent with previous research, an overall intention score could be derived from the sum of the four items, with higher scores indicating greater intention (15). The Cronbach’s ɑ for intention subscale was 0.87 at baseline and 0.93 at follow-up. Attitude was assessed as the summed scores of fourteen items, each measured on a semantic differential scale using bipolar adjective pairs (e.g., “For me, preventing diabetic foot and limb amputation from now on is “very important” or very unimportant”). To minimize response biases (15), items were arranged so that the endpoints of the scales were a mix of positive and negative, and scores were reverse coded before analysis, as needed. These items measured both instrumental and affective attitudes; a higher score indicated a stronger positive attitude towards foot care activities. These fourteen items had high internal consistency (Cronbach’s ɑ = 0.74 at baseline and 0.77 at follow-up). Subjective norms were measured using seven items. Items assessed both injunctive and descriptive subjective norms (17) and were measured on a unipolar (+1 to +5) scale ranging from “strongly disagree” to “strongly agree.” (e.g., “Most people who are important to me think that I should perform foot care on a daily basis”). A higher score indicates greater perceived social pressure to perform foot care. The seven-item subjective norms subscale had adequate internal consistency (Cronbach’s ɑ = 0.83 at baseline and 0.86 at follow-up). PBC was measured using three items; two items measured the extent to which the individual believed that foot care was under his/her control (e.g. “It is mostly up to me whether or not I perform foot care from now on”; ratings ranged from “strongly agree” to “strongly disagree”) and two items measured the perceived ease or difficulty of foot care (e.g. “If I wanted to I could perform foot care from now on”; ratings ranged from “strongly agree” to “strongly disagree”). The overall PBC score was derived from the sum of these five items, with a higher score indicating greater perceived control over behavior (15). The Cronbach’s ɑ for the three items of the PBC subscale was 0.71 at baseline and 0.86 at follow-up.
3.3.2. Behavior
Foot self-care was assessed using the Summary of Diabetes Self-Care Activities-Revised and Expanded (SDSCA-RandE), developed by Toobert et al. (18). The SDSCA-RandE has four items assessing recommended foot care among persons with type II diabetes mellitus; items are rated on a 7-point scale from 0 (i.e., “foot self-care was never performed during the past week”) to 7 days (i.e. “foot self-care done every day during the past week”). The items are as follows: (1) On how many of the last 7 days did you wash your feet? (2) On how many of the last 7 days did you dry between your toes after washing? (3) On how many of the last 7 days did you check your feet? (4) On how many of the last 7 days did you inspect the insides of your shoes? The scores of the four items are summed to create a total score for foot care in the previous week.
3.4. Ethical Considerations
After obtaining permission from the research council and ethical committee of the university (Ethical code: ajums. REC. 1392, 35) and coordinating with the authorities of Ahvaz Golestan Hospital and the Diabetes Clinic, we conducted the study. Before completing the questionnaire, participants were informed of their role in the study, their confidentiality, how we would not inappropriately use their information, and the objective of the study; then, written consent was obtained for inclusion. The participants were assured of the right to withdraw anytime during the study period at no additional cost or disadvantage to them. The current study was part of an MSc thesis in medical surgical nursing approved by the Ahvaz Jundishapur University of Medical Sciences, Iran, and has been registered in the Iranian registry of clinical trials (IRCT ID: IRCT2013051113292N1).
3.5. Statistical Analysis
Data were analyzed using SPSS version 19. The chi-square test was used to compare nominal variables between the two groups, the paired t-test was used to compare pre- and post-test mean scores of the TPB variables and foot care in each group, and the independent t-test to compare scores between the control and intervention groups. A P < 0.05 was considered significant.
4. Results
Eighty participants completed baseline data collection. Participants’ age ranged from 30 to 60 years, with a mean of 54.32 years (SD = 10.3). The majority of participants (53.6%) were male (Table 1).
| Group | Intervention (n = 35) | Control (n = 34) | P |
|---|---|---|---|
| Age, y | 0.79 | ||
| 30 - 40 | 8 (22.9) | 6 (17.6) | |
| 41 - 50 | 11 (31.4) | 13 (38.2) | |
| 51 - 60 | 16 (45.7) | 15 (44.1) | |
| Gender | 0.91 | ||
| Male | 19 (54.3) | 18 (52.9) | |
| Female | 16 (45.7) | 16 (47.1) | |
| Marital status | 0.5 | ||
| Married | 30 (85.7) | 32 (94.2) | |
| Single | 5 (14.3) | 4 (9.8) | |
| Diabetes duration, y | 0.45 | ||
| 1 - 5 | 21 (60) | 15 (44.1) | |
| 6 - 10 | 8 (22.9) | 9 (26.5) | |
| 11 - 15 | 3 (8.6) | 7 (20.6) | |
| 16 - 20 | 3 (8.6) | 3 (8.8) | |
| Diabetes treatment | 0.66 | ||
| Oral | 23 (65.7) | 24 (70.6) | |
| Insulin | 12 (34.3) | 10 (24.9) | |
| Family history of diabetes | 23 (65.7) | 20 (58.8) | 0.55 |
| Diabetic foot history | 15 (42.9) | 16 (47.1) | 0.72 |
| Other disease history | 18 (51.4) | 25 (73.5) | 0.06 |
| Smoking | 7 (20) | 12 (35.3) | 0.15 |
| Fasting Blood Suger, mg/dL | 0.47 | ||
| 60 - 150 | 8 (22.9) | 8 (23.5) | |
| 151 - 240 | 15 (42.8) | 9 (26.5) | |
| 241 - 330 | 8 (22.9) | 10 (29.4 | |
| > 330 | 4 (11.4) | 7 (20.6) |
Participant Characteristics (n = 69) a
A series of independent t-tests and chi-square tests of independence were conducted to ensure that the two groups were equivalent at baseline. The two groups were compared in terms of all demographic variables and the baseline TPB and foot care measures. The results showed that there were no significant group differences for any variables (P > 0.05). Therefore, it was concluded that randomization was successful.
Of participants enrolled in the study, 69 completed the follow-up questionnaire at the fourth week. This represents a loss to follow-up of 13.7%. A series of independent t-tests were conducted to ensure that the participants who dropped out of the study at follow-up did not significantly differ from those who finished the study. Specifically, participants who dropped out of the study were compared to completers in terms of baseline TPB and foot care measures. The results showed that there were no significant differences between completers and dropouts in any of these measures (P > 0.05). Therefore, it was concluded that selective attrition was not likely to be a factor in this study.
First, we examined both groups for possible changes in variables over the intervention period. The intervention effects were formally compared using paired t-tests, which examined changes in primary and secondary outcome measures between the two time points (baseline and follow-up). In both the intervention and control groups, attitude increased significantly between baseline and follow-up, indicating that participants had a more positive attitude for foot care practices at follow-up than they did at pre-intervention. PBC increased an average of 1.35 points between baseline and follow-up; this effect was significant. This indicates an increase in the perception that foot care was achievable or controllable. There was a significant difference in reported foot care between baseline and follow-up. However, subjective norms also increased, by an average of 1.9 points, between baseline and follow-up. This effect was not significant. This finding indicates an increase in perceived social pressure to perform foot care between baseline and follow-up. There was no significant difference in the intention to practice foot care between baseline and follow-up. Of course, it should be said that the mean intention score was rather high at baseline, although this does not appear to have affected their foot care behavior. Next, we determined the differences between the intervention and control groups at follow-up using independent t-tests. Despite the increases in the average scores of all TPB variables at follow-up, there were only significant differences between groups in attitude, and foot care; there were no significant differences in PBC, subjective norms or intention. The results of these analyses are summarized in Table 2.
| Variables and Time | Control (n = 34) | Intervention (n = 35) | Independent t-Test |
|---|---|---|---|
| Attitude | |||
| Baseline | 48.44 ± 5.88 | 50.12 ± 7.7 | 0.31 |
| Follow-up | 49.78 ± 7 | 54.18 ± 6.72 | 0.001 |
| Paired t-test | 0.0001 | 0.001 | |
| Subjective norms | |||
| Baseline | 31.57 ± 2.94 | 29.89 ± 4.06 | 0.051 |
| Follow-up | 31.78 ± 2.73 | 30.8 ± 2.73 | 0.118 |
| Paired t-test | 0.53 | 0.083 | |
| Perceived behavioral control | |||
| Baseline | 19 ± 3.6 | 17.8 ± 3.7 | 0.174 |
| Follow-up | 19.8 ± 3.45 | 19.15 ± 3.15 | 0.39 |
| Paired t-test | 0.18 | 0.004 | |
| Intention | |||
| Baseline | 16.84 ± 3.12 | 16.64 ± 2.56 | 0.80 |
| Follow-up | 17.4 ± 2.16 | 17.24 ± 1.8 | 0.75 |
| Paired t-test | 0.16 | 0.11 | |
| Foot care | |||
| Baseline | 17.76 ± 7.84 | 16.32 ± 7.76 | 0.45 |
| Follow-up | 18.96 ± 7.36 | 19.32 ± 6.48 | 0.0001 |
| Paired t-test | 0.19 | 0.001 |
Baseline and Follow-up Means (Standard Deviations) of TPB Variables and Foot Care (n = 69) a
5. Discussion
The results of this study were only partially supportive of the hypotheses derived from the TPB (8). The intervention led to increased performance of foot care amongst this sample of Iranian diabetic patients. Average self-reported foot care in the intervention group rose by 3 points between baseline and an immediate post-intervention follow-up. In their study on the same topic, Darker et al. reported that the average time participants spent walking increased from 19.8 minutes to 32.2 minutes per day after they took part in an educational intervention based on the TPB (19). In his study, Dydarlu also reported that a theory-based educational intervention could increase self-care behaviors (including adherence to drugs; compliance with recommended diets, exercise, and physical activity; and self-monitoring of blood glucose), improve metabolic control (reduction of HbA1c), and improve quality of life in patients with diabetes (20). These prior results are consistent with the results obtained in the present study regarding foot care in patients. Unlike in the present study, Kinmonth et al. found that an educational intervention based on the TPB had no effect on the amount of physical activity (21). The reason for this difference could be the measurement of physical activity, which they did through more objective measures such as heart rate monitoring or HbA1c. Similarly, Ahmadi Tabatabai et al. reported that intervention and control participants did not differ in terms of physical activity after an educational intervention, which is also inconsistent with the results of the present study (22). Notably, in Ahmadi Tabatabai et al.’s study, the TPB-based educational program comprised only one 2-hour lecture, which is perhaps the cause of the observed differences.
The present results also indicated that our TPB-based intervention successfully improved attitudes towards foot care. A study by Dydarlu on this same topic showed that an educational intervention based on the extended theory of reasoned action led to significant improvements in attitudes toward the practice of self-care behaviors among diabetic women (20). Additionally, White et al., in a study evaluating the effect of a TPB-based educational intervention on the promotion of physical activity and healthy eating in adults with type II diabetes, reported that, after the intervention, attitudes toward practicing regular physical activity statistically differed between the intervention and control groups, which is consistent with the results of the present study. However, in contrast with the results of the present study, White et al. reported no statistically significant change after the intervention in attitudes towards healthy eating (11). Ahmadi Tabatabai et al. also found no statistically significant difference between participants’ attitudes before and after a TPB-based intervention for physical activity, which is inconsistent with the results obtained in this study (22). As mentioned above, differences in educational methods based on the theory and measurement tools can cause conflicting results.
Although our TPB-based intervention led to significant increases in mean scores of subjective norms and PBC in the intervention group from baseline to follow-up, the scores at follow-up were not significantly different between the two groups. Subjective norms are one component of the TPB and refer to the amount of social support or pressure influencing an individual to adopt a desired behavior. If there is greater social support and pressure by family members (especially spouses), physicians, health experts, and friends to perform certain healthy behaviors, then it is more likely that the patient will engage in such behaviors (20). After implementing a TPB-based educational intervention to promote walking, Darker et al. reported no differences between the intervention and control groups in mean scores for subjective norms, which is consistent with the results of the present study (19). Ahmadi Tabatabai et al. also reported that their TPB-based intervention aimed at promoting physical activity had no effect on the subjective norms of study participants, which is consistent with the results of the present study (22). In contrast, Dydarlu reported that the mean score of subjective norms for self-care behaviors in women with type II diabetes increased significantly after his TPB-based intervention (20). As was previously mentioned, the intervention group, at the end of the second session, were asked to give their educational booklets on foot care to their own family members, which we posited would influence their subjective norms. Therefore, it can be concluded that this intervention method was unsuccessful in improving participants’ subjective norms. It seems that there are no adequate measures available to increase social support (i.e. subjective norms) among patients in this study; to do so, more time might be spent educating patients as well as families, caregivers, friends, and even health care providers in direct contact with the patient. In addition, it might be helpful to attempt to highlight the roles of people whose recommendations are important to the patient regarding observation of self-care behaviors (including foot care).
PBC refers to individuals’ beliefs about their ability to organize activities and successfully perform an intended behavior to achieve specific results in certain situations; in other words, it refers to the degree that people feel that they have voluntary control over their behavior. If there are restrictions on performing the behavior—namely, an individual feels that he/she does not have adequate facilities or time to perform that behavior then the individual may not experience a strong intention to perform that behavior, despite having a positive attitude and high subjective norms (17). Dydarlu reported significant improvements in the mean score of PBC for self-care behaviors among intervention-group women with type II diabetes after implementation of his educational intervention. This differs from the results of our study (20). Darker et al. also found that the mean score of PBC for walking in the intervention group increased significantly after their TPB-based intervention, which is not consistent with the results of the present study (19). In contrast, Parrott et al., who evaluated the effect of a TPB-based educational intervention on the promotion of physical activity in a group of adults, found no significant changes in scores of PBC after intervention, which is in line with the results of the present study (23). Mehri et al. and Barati et al. also reported no significant changes in the mean scores of PBC in their intervention groups after a TPB-based intervention, which is consistent with the results of the present study (24, 25). However, we might suggest that the current educational program does affect PBC, but only to a minor extent. In addition, since PBC depends on the presence or absence of perceived facilitators of or barriers to an ability or behavior, there might have been numerous barriers in the program or previously existing barriers that were not completely resolved via the educational program. Similarly, a study by Baghianimoghadam et al. found that in a group of people with type II diabetes, people’s understanding of their level of control over their behavior toward walking was associated with age and educational level; specifically, greater age and lower education level were associated with reduced understanding of their control over their own behavior (26). Jahanloo et al. noted similar results in this regard (27). Since about half of the people who participated in this study were aged 51 - 60 years and had only a primary-level education, the non-significant change in the mean score of PBC may have been associated with participants’ higher mean age and education level.
The results also indicated that the TPB-based intervention had no impact on patients’ intention to perform foot care. Darker et al. stated that the mean score of intention to walk in the intervention group increased significantly after their TPB-based intervention, which is not consistent with the results of the present study (19). However, White et al. reported that, after their intervention, the intention to engage in healthy eating was not significantly different between the intervention and control groups, which is consistent with the results of the present study (11). It should be noted that although interventions targeting behavioral, normative, or control beliefs may succeed in producing corresponding changes in attitudes, subjective norms, and PBC, which in turn would influence individuals’ intentions in the desired direction, the intervention would have no effect unless the individuals are able to actually carry out these intentions. Thus, researchers must ensure a strong link from intentions to behavior; specifically, if this link is weak, then steps should be taken to strengthen it. Perhaps the most effective means of doing so currently is to have individuals form an implementation intention in other words, a specific plan detailing when, where, and how the desired behavior should be performed (28). Such plans makes it easier for people to carry out their intended actions; furthermore, it must be said that an intention is necessary for a behavior but is not sufficient for causing that behavior (20).
The intervention resulted in changes in attitudes and self-reported behavior; however, the obtained results do not support the hypotheses that the intervention would result in changes in subjective norms, PBC, and intention to engage in foot care. These are promising findings, suggesting that an intervention based on the TPB could promote foot care in Iranian diabetic patients. Given the short-term follow-up used in the current study, it is difficult to determine the long-term effects of this TPB-based intervention. However, it is interesting to note that several interventions used to promote self-care behaviors among type II diabetic patients have been able to maintain intervention effects over the medium- to long-term (11, 20). Further research is needed to determine whether the increased foot care observed in the current study can be maintained over time.
5.1. Strengths and Limitations
There were a number of strengths to this study. First, this study has an explicit theoretical basis: The TPB was used in the current study as a theoretical framework to design, implement, and evaluate an intervention. Second, the TPB has previously mainly been used to measure processes and outcome variables and to predict intention and behavior; it has been used less commonly to develop or evaluate interventions (29). By contrast, the present study tested the effects of an intervention, which ultimately yielded strong effects on behavior. Third, this is the only study, based on literature review, to utilize the TPB to develop and evaluate an intervention specifically for foot care in a diabetic patient sample. There were also a number of limitations to the present study. The self-report nature of the SDSCA-RandE introduces a degree of bias inherent to survey research. Direct observation of participants’ foot care would have provided a more reliable source of measurement for this behavioral variable. However, most previous studies utilized this method for data collection (11, 20-22), and there was no possibility for a more accurate assessment of participants. Another limitation of this study is that participants’ psychological states could have affected their responses. Controlling this limitation would have been difficult for the researchers.