1. Background
Patients hospitalized in intensive care units (ICUs) perceive high levels of stress and anxiety due to fear regarding diagnosis, aggressive treatments, using different devices, sleep deprivation, motor restriction and also restricted hospital visiting hours (1). Visiting patients admitted to the ICU is entirely forbidden even for family members in all ICUs of all hospitals in Iran for different reasons (2) including the nurses’ false beliefs that family members interfere with patient’s care, increase the risk of infection, and disturb patient’s rest causing the patient’s anxiety and stress. However, studies have proven that allowing relatives to visit their beloved ones more are ranked high in the list of important needs of patients hospitalized in ICUs (3). Separating sick people from their beloved ones can cause great suffering for patients just as modern science has concluded (4, 5). Unfortunately, the current knowledge has not been yet successful to change the false beliefs regarding visiting patients in ICUs (6, 7).
In addition to physical problems, patients in the ICU experience psychological reactions such as stress which may lead to increased treatment costs, delay in recovery, cardiovascular complications and increasing mortality rates (8-11). Also, results of the studies on patients with coronary artery diseases reveal positive impact of talking to, looking at, smiling to and touching conscious patients in stimulating the nervous system, decreasing the heart rate and diastolic blood pressure, and reducing anxiety (12).
Physiological indices (systolic and diastolic blood pressures, mean arterial pressure, respiratory and heart rates) have been recognized as the important factors in improvement of patients’ general condition and that of treatment progress (13). In this regard, improved physiological measures resulting from increased visitation time will accelerate weaning of the patients from mechanical ventilation and may help to reduce its complications, length of stay in ICU, and hospital costs (14).
Since few studies have investigated the impact of extending visitation time on the physiological indices of patients hospitalized in the ICU and the importance of the presence of family members next to these patients for more longer periods (15) and the concept of the family-centered care model has been considered by medical staff as a new therapeutic approach, few such surveys in Iran have been carried out as well, mostly on the patients admitted to cardiac ICUs, and have had conflicting results (16-18).
2. Objectives
Thus, the present study seems to confirm the previous findings and provide new suggestions. Therefore, the present study aimed to evaluate the effect of extending visitation time on the physiological parameters of the patients admitted to ICUs.
3. Materials and Methods
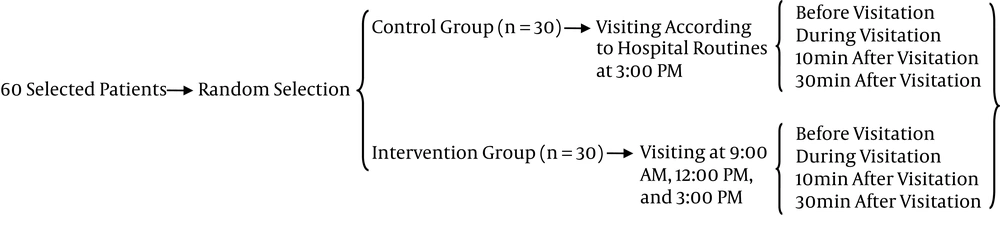
In this clinical trial study, 60 subjects were selected through the convenience method (Equation 1) and then were randomly divided into two groups of intervention and control through the simple random method of assigning odd numbers to one group and even ones to the other group. The subjects were selected from the patients admitted to ICUs of Vali-e-Asr hospital in Arak city (surgical ICU and neurology ICU). The following characteristics were required for the participation in the study: (1) being hospitalized in ICU with consciousness level higher than 7.2, (2) having been hospitalized in ICU for at least 24 hours, (3) aged more than 18 and less than 70, (4) not being under complete isolation, (5) agreement of the first degree relatives of the patient toward their participation in the study, (6) having no hearing deficits. Exclusion criteria were (1) simultaneous participation in another study that can interfere with the present one, (2) being under treatment with sedatives, (3) too much sensitivity of family members toward the patient disturbing the treatment process, and (4) exhaustion of family members due to caring their patient (Figure 1).

Data were collected using two questionnaires: first including items concerning demographic characteristics and the second including items concerning 6 physiological indices of systolic and diastolic blood pressures, mean arterial pressure, pulse and respiratory rates, and oxygen saturation (O2sat). Since the first questionnaire was demographic and the second one only concerned physiological indices, there was no need to establish their validity and reliability.
In order to prevent bias while gathering the data, the researchers acted in a way that the nurses had no idea of the nature of the study. Thus, the presence of the visitors and its effect on physiological indices was not revealed to the nurses measuring these indices. Double-blind procedure was used in this study to prevent the bias, that is, both patients’ families and nurses measuring the indices were not informed of the importance of increased visitation time in the study.
The questionnaire of demographic characteristics and health monitoring checklist were used for gathering the data. The cardiac monitoring system’s validity was confirmed referring to the manufacture’s manual, using standard tools (audio and visual settings and annual control of thermal and pressure sensors using analyzers), selecting devices from leading brands, and calibration certificate issued by a medical equipment engineer before starting sampling. To ensure valid and reliable measurements of the physiological parameters, a single monitoring device, Data Ohmeda (GIMM Company), was used for all participants. The blood pressure of the participants was measured by non-invasive monitoring on the right arm (and on the left arm for amputees, paralyzed patients, etc.) in supine position and 30-degree head-up state and recorded automatically on the cardiac monitor. In order to determine the arterial oxygen saturation, the index finger of the patient’s right hand was completely placed into the probe and the digit on the monitor was recorded. Heart and respiratory rates were observed and recorded using cardiac monitoring device and Chest Lead. Sampling was performed during morning and afternoon working shifts. In this study, the ICU patients were considered as the control group and visitors were allowed to visit the patients during the routine hospital visiting time at 3:00 PM in the afternoon for 10 minutes. The patients in neurological ICU were considered as the intervention group and visiting times were at 9:00 AM, 12:00 PM, and 3:00 PM each for 10 minutes. Using a questionnaire, the effect of visitation by relatives on the physiological indices of the patients in both control and intervention groups were recorded and assessed 10 minutes before starting the visitation time, during visitation, and 10 and 30 minutes after the visitation. Then, the obtained data were analyzed using SPSS version 20 and descriptive statistic tests (mean and standard deviation) and qualitative data using chi-square test and the means were compared using the independent t-test and repeated measure test.
This study was approved by the ethical code of 93-164-2 in 2 July 2014 and its IRCT code is 2014052617873N1.
4. Results
The chi-square test results showed that the two groups were homogenous in terms of socio-demographic characteristics including age, sex, marital status, hospitalization background, income, etc. before the study (P > 0.05).
The results of the repeated measure in the control group (visitation time according to hospital routines) in different times showed that there was no significant difference among physiological statuses measured at 15 pm (P < 0.05).
The results of Mauchly’s test of sphericity 2 with P < 0.05 rejected the sphericity conditions. Therefore, given that sphericity assumption is not held, Greenhouse-Geisser correction 3 was used for conducting the repeated measure test in 4 different measurements for intra-rater effects. The result of the test showed that in the intervention group there was a significant difference among the mean values of the measured indices in three times (9:00 AM, 12:00 PM, and 3:00 PM) and in 4 different measurements (P < 0.0001).
Following revealing the significance of the measured indices’ mean values in 4 measuring times at 9:00 AM, 12:00 PM, and 3:00 PM, mutual assessing of significant difference among these 4 means was conducted using paired comparisons (means difference (I - J)) through the Bonferroni post hoc test, as shown in the following tables representing the change occurred in the means of the studied indices.
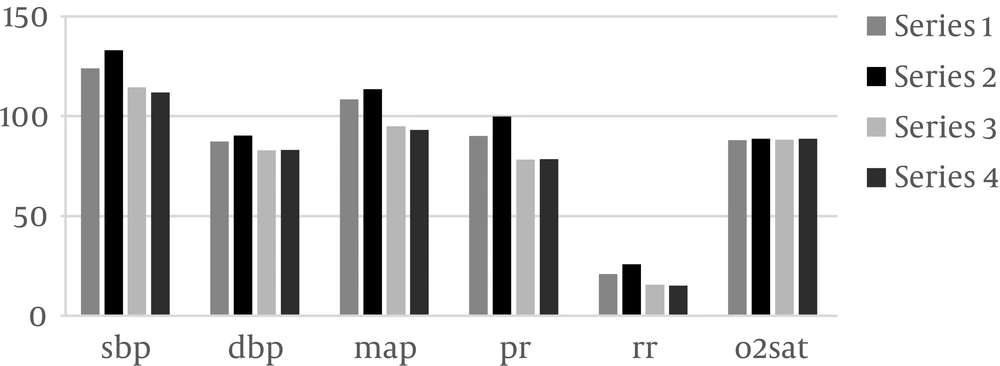
As the Table 1 indicates, physiological indices of the patients in the control group were evaluated just before 9:00 AM, while these indices of those in the intervention group were measured before, during and 10 minutes and then 30 minutes after visitation. The results suggested that blood pressure parameters (the mean systolic blood pressure: 114.40, mean diastolic blood pressure: 90.4, mean arterial pressure: 113.60, mean heart rate: 99.7, and mean respiratory rate: 25.7) had the highest mean values during the hospital visitation and means’ differences were statistically significant in 4 different measurements (P < 0.05). No increase, however, was reported in arterial oxygen index during the visitation compared to before visitation (mean difference = -0.34). Given the results of repeated measures, changes in these indices at 9:00 AM in the intervention group suggested improvement in physiological status of the patients after planned hospital visitations (Figure 2, Tables 2 and 3).
| Measure/Time | Mean ± Std. Error | 95% Confidence Interval | |
|---|---|---|---|
| Lower Bound | Upper Bound | ||
| SBP | |||
| Before | 124.033 ± 2.096 | 119.746 | 128.321 |
| During | 133.033 ± 1.506 | 129.953 | 136.113 |
| 10 | 114.400 ± 1.744 | 110.834 | 117.966 |
| 30 | 111.900 ± 1.722 | 108.379 | 115.421 |
| DBP | |||
| Before | 87.400 ± 0.581 | 86.213 | 88.587 |
| During | 90.400 ± 0.590 | 89.193 | 91.607 |
| 10 | 82.867 ± 0.655 | 81.527 | 84.207 |
| 30 | 83.233 ± 0.592 | 82.022 | 84.445 |
| MAP | |||
| Before | 108.433 ± 0.886 | 106.621 | 110.246 |
| During | 113.600 ± 0.954 | 111.650 | 115.550 |
| 10 | 94.900 ± 0.842 | 93.178 | 96.622 |
| 30 | 93.133 ± 0.731 | 91.637 | 94.629 |
| PR | |||
| Before | 90.033 ± 1.189 | 87.601 | 92.466 |
| During | 99.767 ± 1.661 | 96.369 | 103.165 |
| 10 | 78.233 ± 0.860 | 76.475 | 79.992 |
| 30 | 78.400 ± 0.744 | 76.879 | 79.921 |
| RR | |||
| Before | 20.900 ± 0.451 | 19.978 | 21.822 |
| During | 25.767 ± 0.449 | 24.848 | 26.685 |
| 10 | 15.633 ± 0.260 | 15.101 | 16.166 |
| 30 | 15.033 ± 0.242 | 14.538 | 15.528 |
| O2sat | |||
| Before | 88.033 ± 0.520 | 86.970 | 89.096 |
| During | 84.767 ± 0.558 | 83.624 | 85.909 |
| 10 | 88.167 ± 0.508 | 87.128 | 89.205 |
| 30 | 88.667 ± 0.564 | 87.513 | 89.820 |
Abbreviations: DBP, diastolic blood pressure; O2sat, oxygen saturation; RR, repertory rate; SBP, systolic blood pressure.
| Measure/Factor 1 (I)/Factor 1 (J) | Mean Difference (I - J) | Std. Error | P Value | 95% Confidence Interval for Difference | |
|---|---|---|---|---|---|
| Lower Bound | Upper Bound | ||||
| SBP | |||||
| Before | |||||
| During | -9.000a | 1.313 | 0.0001 | -12.718 | -5.282 |
| 10 | 9.633a | 0.992 | 0.0001 | 6.823 | 12.444 |
| 30 | 12.133a | 1.650 | 0.0001 | 7.462 | 16.804 |
| During | |||||
| 10 | 18.633a | 1.150 | 0.0001 | 15.376 | 21.890 |
| 30 | 21.133a | 1.407 | 0.0001 | 17.148 | 25.119 |
| 10 | |||||
| 30 | 2.500 | 1.314 | 0.402 | -1.220 | 6.220 |
| DBP | |||||
| Before | |||||
| During | -3.000a | 0.398 | 0.0001 | -4.128 | -1.872 |
| 10 | 4.533a | 0.621 | 0.0001 | 2.775 | 6.292 |
| 30 | 4.167a | 0.638 | 0.0001 | 2.360 | 5.973 |
| During | |||||
| 10 | 7.533a | 0.669 | 0.0001 | 5.639 | 9.428 |
| 30 | 7.167a | 0.692 | 0.0001 | 5.208 | 9.125 |
| 10 | |||||
| 30 | -0.367 | 0.347 | 1.000 | -1.350 | 0.617 |
| MAP | |||||
| Before | |||||
| During | -5.167a | 0.875 | 0.0001 | -7.644 | -2.689 |
| 10 | 13.533a | 0.966 | 0.0001 | 10.799 | 16.268 |
| 30 | 15.300a | 0.983 | 0.0001 | 12.517 | 18.083 |
| During | |||||
| 10 | 18.700a | 1.015 | 0.0001 | 15.826 | 21.574 |
| 30 | 20.467a | 0.969 | 0.0001 | 17.722 | 23.211 |
| 10 | |||||
| 30 | 1.767 | 0.664 | 0.075 | -0.113 | 3.646 |
Abbreviations: DBP, diastolic blood pressure; SBP, systolic blood pressure.
aSignificant.
| Measure/Factor 1 (I)/Factor 1 (J) | Mean Difference (I - J) | Std. Error | P Value | 95% Confidence Interval for Difference | |
|---|---|---|---|---|---|
| Lower Bound | Upper Bound | ||||
| PR | |||||
| Before | |||||
| During | -9.733a | 1.073 | 0.0001 | -12.772 | -6.695 |
| 10 | 11.800a | 0.972 | 0.0001 | 9.046 | 14.554 |
| 30 | 11.633a | 1.002 | 0.0001 | 8.797 | 14.470 |
| During | |||||
| 10 | 21.533a | 1.498 | 0.0001 | 17.293 | 25.774 |
| 30 | 21.367a | 1.425 | 0.0001 | 17.331 | 25.402 |
| 10 | |||||
| 30 | -0.167 | 0.413 | 1.000 | -1.335 | 1.002 |
| RR | |||||
| Before | |||||
| During | -4.867a | 0.342 | 0.0001 | -5.834 | -3.900 |
| 10 | 5.267a | 0.447 | 0.0001 | 4.001 | 6.532 |
| 30 | 5.867a | 0.544 | 0.0001 | 4.326 | 7.407 |
| During | |||||
| 10 | 10.133a | 0.439 | 0.0001 | 8.891 | 11.376 |
| 30 | 10.733a | 0.514 | 0.0001 | 9.278 | 12.189 |
| 10 | |||||
| 30 | 0.600 | 0.274 | 0.219 | -0.175 | 1.375 |
| O2sat | |||||
| Before | |||||
| During | 3.267a | 0.371 | 0.0001 | 2.216 | 4.318 |
| 10 | -0.133 | 0.398 | 1.000 | -1.259 | 0.992 |
| 30 | -0.633 | 0.414 | 0.820 | -1.805 | 0.538 |
| During | |||||
| 10 | -3.400a | 0.451 | 0.0001 | -4.678 | -2.122 |
| 30 | -3.900a | 0.427 | 0.0001 | -5.109 | -2.691 |
| 10 | |||||
| 30 | -0.500 | 0.283 | 0.524 | -1.300 | 0.300 |
Abbreviations: O2sat, oxygen saturation; RR, repertory rate.
aSignificant.
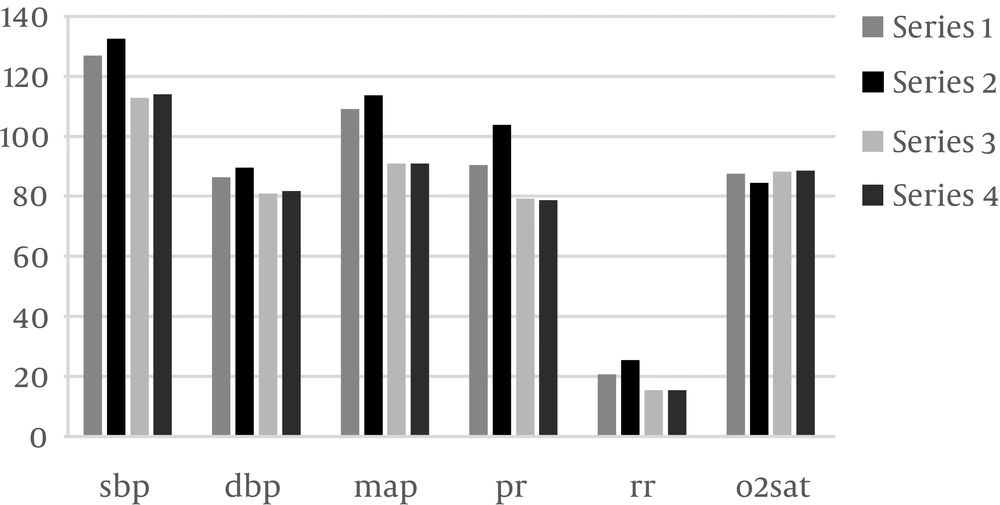
Evaluating indices for patients in the control and intervention groups at 12:00 PM indicated that, like the case in 9:00 AM, blood pressure indices (the mean systolic blood pressure: 132.5, mean diastolic blood pressure: 89.6, mean arterial pressure: 113.7, mean heart rate: 103.73) had the highest mean values during visitation. However, the arterial oxygen saturation level was not significantly increased compared to before visitation (mean difference: -0.34) (P > 0.05). These kinds of changes can be due to the patient’s emotions associated with visiting her/ his relatives (Table 4 for 12:00 PM; Tables 5 and 6 and Figure 3).
| Measure/Time | Mean ± Std. Error | 95% Confidence Interval | |
|---|---|---|---|
| Lower Bound | Upper Bound | ||
| SBP | |||
| Before | 126.933 ± 1.744 | 123.367 | 130.500 |
| During | 132.500 ± 1.806 | 128.806 | 136.194 |
| 10 | 112.800 ± 1.979 | 108.752 | 116.848 |
| 30 | 114.033 ± 1.817 | 110.318 | 117.749 |
| DBP | |||
| Before | 86.800 ± 0.631 | 85.509 | 88.091 |
| During | 89.633 ± 0.665 | 88.273 | 90.994 |
| 10 | 80.967 ± 0.704 | 79.527 | 82.406 |
| 30 | 81.733 ± 0.551 | 80.607 | 82.860 |
| MAP | |||
| Before | 109.133 ± 0.963 | 107.163 | 111.104 |
| During | 113.700 ± 0.791 | 112.082 | 115.318 |
| 10 | 90.933 ± 0.816 | 89.264 | 92.603 |
| 30 | 91.000 ± 0.932 | 89.093 | 92.907 |
| PR | |||
| Before | 89.833 ± 1.284 | 87.207 | 92.459 |
| During | 103.733 ± 1.762 | 100.129 | 107.338 |
| 10 | 79.167 ± 0.867 | 77.393 | 80.940 |
| 30 | 78.667 ± 0.843 | 76.942 | 80.391 |
| RR | |||
| Before | 20.667 ± 0.466 | 19.714 | 21.619 |
| During | 25.533 ± 0.552 | 24.404 | 26.663 |
| 10 | 15.433 ± 0.364 | 14.689 | 16.178 |
| 30 | 15.400 ± 0.298 | 14.791 | 16.009 |
| O2sat | |||
| Before | 87.600 ± 0.495 | 86.588 | 88.612 |
| During | 84.567 ± 0.669 | 83.198 | 85.935 |
| 10 | 88.133 ± 0.502 | 87.106 | 89.161 |
| 30 | 88.600 ± 0.430 | 87.720 | 89.480 |
Abbreviations: DBP, diastolic blood pressure; O2sat, oxygen saturation; RR, repertory rate; SBP, systolic blood pressure.
| Measure/Time (I)/Time (J) | Mean Difference (I - J) | Std. Error | P Value | 95% Confidence Interval for Difference | |
|---|---|---|---|---|---|
| Lower Bound | Upper Bound | ||||
| SBP | |||||
| Before | |||||
| During | -5.567a | 0.761 | 0.000 | -7.122 | -4.011 |
| 10 | 14.133a | 1.504 | 0.000 | 11.058 | 17.209 |
| 30 | 12.900a | 1.587 | 0.000 | 9.655 | 16.145 |
| During | |||||
| 10 | 19.700a | 1.585 | 0.000 | 16.458 | 22.942 |
| 30 | 18.467a | 1.631 | 0.000 | 15.130 | 21.803 |
| 10 | |||||
| 30 | -1.233 | 0.771 | 0.121 | -2.811 | 0.344 |
| DBP | |||||
| Before | |||||
| During | -2.833a | 0.622 | 0.000 | -4.105 | -1.562 |
| 10 | 5.833a | 0.767 | 0.000 | 4.264 | 7.403 |
| 30 | 5.067a | 0.785 | 0.000 | 3.462 | 6.672 |
| During | |||||
| 10 | 8.667a | 0.660 | 0.000 | 7.317 | 10.016 |
| 30 | 7.900a | 0.680 | 0.000 | 6.509 | 9.291 |
| 10 | |||||
| 30 | -0.767a | 0.345 | 0.034 | -1.472 | -0.062 |
| MAP | |||||
| Before | |||||
| During | -4.567a | 0.598 | 0.000 | -5.790 | -3.343 |
| 10 | 18.200a | 1.174 | 0.000 | 15.799 | 20.601 |
| 30 | 18.133a | 1.211 | 0.000 | 15.657 | 20.610 |
| During | |||||
| 10 | 22.767a | 1.129 | 0.000 | 20.457 | 25.076 |
| 30 | 22.700a | 1.147 | 0.000 | 20.354 | 25.046 |
| 10 | |||||
| 30 | -0.067 | 0.503 | 0.895 | -1.095 | 0.961 |
Abbreviations: DBP, diastolic blood pressure; SBP, systolic blood pressure.
aSignificant.
| Measure/Time (I)/Time (J) | Mean Difference (I - J) | Std. Error | P Value | 95% Confidence Interval for Difference | |
|---|---|---|---|---|---|
| Lower Bound | Upper Bound | ||||
| PR | |||||
| Before | |||||
| During | -13.900a | 1.363 | 0.000 | -16.688 | -11.112 |
| 10 | 10.667a | 1.600 | 0.000 | 7.395 | 13.939 |
| 30 | 11.167a | 1.556 | 0.000 | 7.984 | 14.349 |
| During | |||||
| 10 | 24.567a | 1.756 | 0.000 | 20.975 | 28.159 |
| 30 | 25.067a | 1.786 | 0.000 | 21.415 | 28.719 |
| 10 | |||||
| 30 | 0.500 | 0.270 | 0.074 | -0.053 | 1.053 |
| RR | |||||
| Before | |||||
| During | -4.867a | 0.321 | 0.000 | -5.523 | -4.211 |
| 10 | 5.233a | 0.306 | 0.000 | 4.608 | 5.859 |
| 30 | 5.267a | 0.368 | 0.000 | 4.514 | 6.019 |
| During | |||||
| 10 | 10.100a | 0.456 | 0.000 | 9.168 | 11.032 |
| 30 | 10.133a | 0.476 | 0.000 | 9.159 | 11.108 |
| 10 | |||||
| 30 | 0.033 | 0.182 | 0.856 | -0.340 | 0.407 |
| O2sat | |||||
| Before | |||||
| During | 3.033a | 0.607 | 0.000 | 1.791 | 4.276 |
| 10 | -0.533 | 0.495 | 0.290 | -1.546 | 0.480 |
| 30 | -1.000 | 0.523 | 0.066 | -2.070 | 0.070 |
| During | |||||
| 10 | -3.567a | 0.529 | 0.000 | -4.648 | -2.485 |
| 30 | -4.033a | 0.607 | 0.000 | -5.276 | -2.791 |
| 10 | |||||
| 30 | -0.467 | 0.283 | 0.109 | -1.045 | 0.111 |
Abbreviations: O2sat, oxygen saturation; RR, repertory rate.
aSignificant.
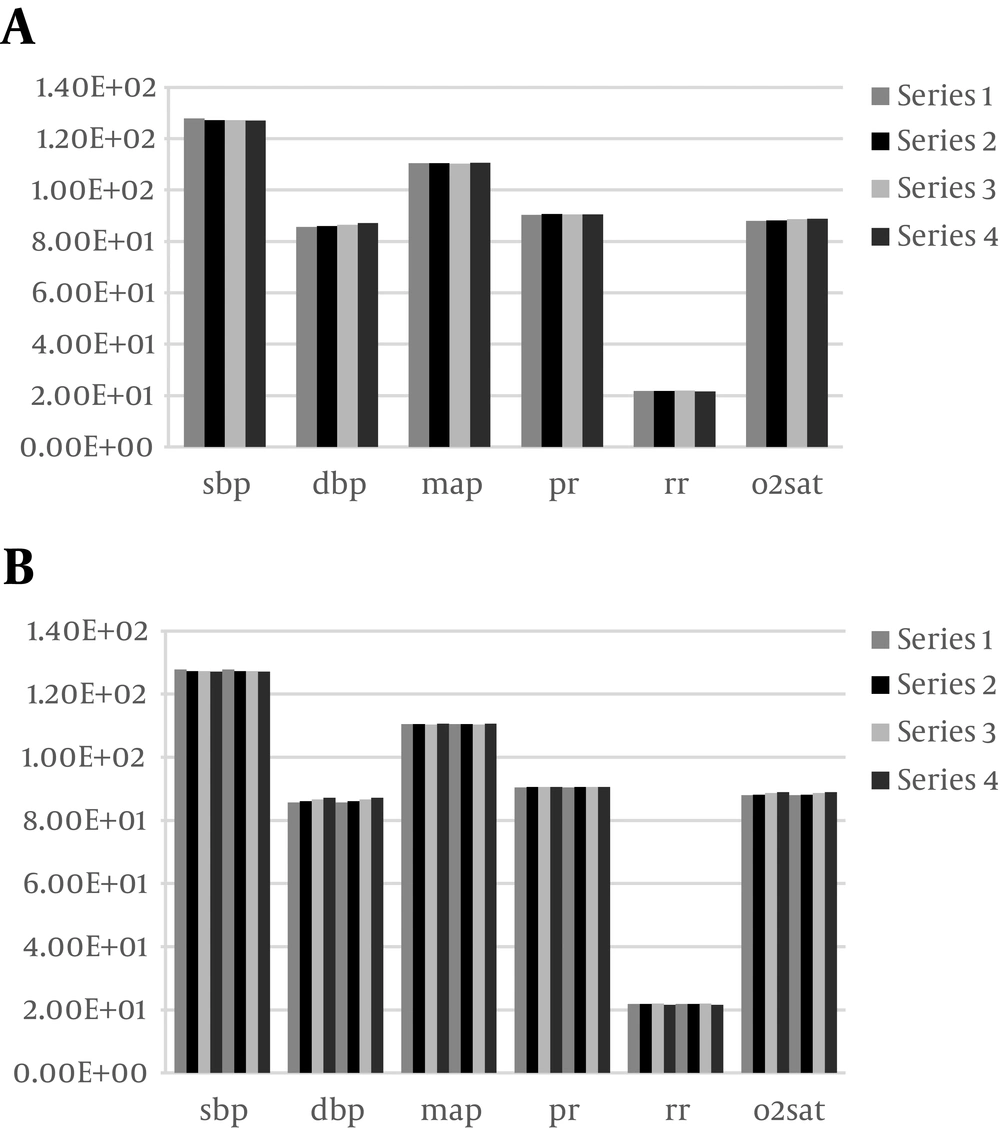
Comparison of the patients’ physiological indices in the control and intervention groups assessed at 3:00 PM showed that no statistically significant difference was observed in any of the visiting hours (P > 0.05), that is, unplanned and limited visitation times did not have much impact on improving patient’s physiological characteristics. However, despite increasing the indices in the subjects of intervention group during visitation times, these parameters showed a significant reduction 10 and 30 minutes after the visitation time (P < 0.05) (Figure 4, Tables 7 and 8).
| Measure/Group | Mean ± Std. Error | 95% Confidence Interval | |
|---|---|---|---|
| Lower Bound | Upper Bound | ||
| SBP | |||
| Control | 127.350 ± 1.233 | 124.883 | 129.817 |
| Intervention | 119.600 ± 1.233 | 117.133 | 122.067 |
| DBP | |||
| Control | 86.350 ± 0.735 | 84.879 | 87.821 |
| Intervention | 86.392 ± 0.735 | 84.921 | 87.862 |
| MAP | |||
| Control | 110.483 ± 0.492 | 109.498 | 111.469 |
| Intervention | 105.158 ± 0.492 | 104.173 | 106.144 |
| PR | |||
| Control | 90.517 ± 1.165 | 88.185 | 92.848 |
| Intervention | 87.925 ± 1.165 | 85.594 | 90.256 |
| RR | |||
| Control | 21.808 ± 0.390 | 21.028 | 22.588 |
| Intervention | 20.075 ± 0.390 | 19.295 | 20.855 |
| O2sat | |||
| Control | 88.442 ± 0.398 | 87.644 | 89.239 |
| Intervention | 88.783 ± 0.398 | 87.986 | 89.581 |
Abbreviations: DBP, diastolic blood pressure; O2sat, oxygen saturation; RR, repertory rate; SBP, systolic blood pressure.
| Source/Measure | Type III Sum of Squares | df | Mean Square | F | P Value |
|---|---|---|---|---|---|
| Group | |||||
| SBP | 900.938 | 1 | 900.938 | 19.764 | 0.0001 |
| DBP | 0.026 | 1 | 0.026 | 0.002 | 0.968 |
| MAP | 425.334 | 1 | 425.334 | 58.520 | 0.0001 |
| PR | 100.751 | 1 | 100.751 | 2.476 | 0.121 |
| RR | 45.067 | 1 | 45.067 | 9.897 | 0.003 |
| O2sat | 1.751 | 1 | 1.751 | 0.368 | 0.547 |
| Error | |||||
| SBP | 2643.900 | 58 | 45.584 | - | - |
| DBP | 939.160 | 58 | 16.192 | - | - |
| MAP | 421.552 | 58 | 7.268 | - | - |
| PR | 2360.010 | 58 | 40.690 | - | - |
| RR | 264.104 | 58 | 4.554 | - | - |
| O2sat | 276.177 | 58 | 4.762 | - | - |
Abbreviations: DBP, diastolic blood pressure; df, degree of freedom; O2sat, oxygen saturation; RR, repertory rate; SBP, systolic blood pressure.
aTests of between-subjects effects.
The results of the mean values of the measured indices in 4 different times in both groups at 3:00 PM showed that the mean values of SBP, MAP, and RR were significantly different between the two groups (P < 0.05), while O2sat, PR, and DBP were significantly different between the two groups. The results of paired comparison based on post hoc LSD test are provided in Table 9.
| Measure | (I) Group | (J) Group | Mean Difference (I - J) | Std. Error | P Value | 95% Confidence Interval for Differenceb | |
|---|---|---|---|---|---|---|---|
| Lower Bound | Upper Bound | ||||||
| SBP | Control | Intervention | 7.750 | 1.743 | 0.0001 | 4.260 | 11.240 |
| DBP | Control | Intervention | -0.042 | 1.039 | 0.968 | -2.121 | 2.038 |
| MAP | Control | Intervention | 5.325 | 0.696 | 0.0001 | 3.932 | 6.718 |
| PR | Control | Intervention | 2.592 | 1.647 | 0.121 | -0.705 | 5.889 |
| RR | Control | Intervention | 1.733 | 0.551 | 0.003 | 0.630 | 2.836 |
| O2sat | Control | Intervention | -0.342 | 0.563 | 0.547 | -1.469 | 0.786 |
Abbreviations: DBP, diastolic blood pressure; O2sat, oxygen saturation; RR, repertory rate; SBP, systolic blood pressure.
Repeated measures analysis of the intervention group’s variances at different hours indicated a significant difference in the measured parameters in various hours (9:00 AM, 12:00 PM, 3:00 PM) (the Greenhouse- Geisser test, P < 0.001).
5. Discussion
The results of the present study showed that the two studied groups were homogenous before performing the study regarding age, marital status, life style, education, occupation, income level, sex, diagnosis, underlying diseases, smoking, and alcohol and drugs abuse.
Our results suggested no significant difference in physiological indices of the patients before applying visitation plans in both control and intervention groups (P > 0.05) that was consistent with the findings of Comruni (16).
According to the results of the evaluations during the first (9:00 AM), second (12:00 PM) and third visitation stages (3:00 PM), the participants in the intervention group showed improvements in physiological indices (including heart rate, respiratory rate, systolic and diastolic blood pressures, and mean arterial pressure) during the visitation (P < 0.05), but no significant effect was reported on arterial oxygen saturation, namely, the difference was not statistically significant (P > 0.05). In the control group, however, mean values of all physiological indices showed no significant difference during the first visitation stage (9:00 AM), the second one (12:00 PM) where visitation was not allowed, and even in the third step where visitation was allowed (P > 0.05). Thus, no remarkable improvement was observed in physiological indices of the patients.
Rahmani et al. (17) concluded that scheduled visitation may decrease physiological parameters and improve treatment results (P < 0.05). However, Salavati and Oshvandi (18) found that scheduling time for families and friends to visit the patient makes no clinical significant improvement in cardiovascular indices (P > 0.05). In their study, no statistically significant difference was observed between the control and intervention groups, which is completely opposing the results of the present study. Also, findings of the study by Comruni et al. (16) suggested significant improvement in physiological indices of the patients in the intervention group.
In addition, physiological indices of the participants showed statistically significant differences 10 and 30 minutes after visitation (P < 0.05) as these parameters decreased, that is, increasing visitation time improved physiological indices of the patients. However, the difference was not significant in the control group.
In the study of Azimi Lolaty et al. (19), increased visitation time significantly improved the feel of comfort, decreased anxiety and enhanced patient’s physiological indices (including systolic and diastolic blood pressure, heart and respiratory rates, and O2sat) (P < 0.001) that is consistent with the findings of the present study.
Also, the research carried out by Zwernman (20) suggested no statistically significant difference among mean arterial pressures measured before, during and after visitation (P > 0.05), while the above-mentioned study proved the positive effect of visiting of relatives on the patient’s mean arterial pressure. In addition, Gerber (21) revealed that respiratory rates showed no statistically significant difference in measurements before, during, and after visitation (P > 0.05) that was due to the differences in the duration of visitation times. While, increased duration of visitation times significantly improved the respiratory status of the patients in this study.
5.1. Conclusions
Findings of the present study show that increased visitation time can lower the mean values of the physiological indices. Therefore, it is recommended that nurses working in the ICUs plan and schedule visitation times focusing on individual, social, and patient-related factors and do not merely consider the hospital principles. Rather, they can help accelerate the patient’s recovery seeking help of their family members.
Although the results of similar studies confirm the results of the present study to a large extent, the indices studied here including systolic and diastolic blood pressure, mean arterial pressure, heart rate, respiratory rate, and O2sat have not been investigated in previous research.
5.2. Limitations
Since intervention studies are conducted on a limited number of subjects, one of the limitations of this study, like other intervention studies, was low number of subjects. Another limitation of the present study was the reluctance of some nursing staff of the ward to participate in this study. However, they were persuaded to participate in the program being explained the importance of the study and illustrating its benefits for patients and health providers. Therefore, it is recommended that the research be carried out in other ICUs such as CCU to achieve more definitive results.