1. Background
Fatty liver disease is a growing diagnosed condition which is characterized by abnormal fat accumulation in the hepatocytes (more than 5% of the liver weight). The pathologic features are similar to those of the alcoholic liver disease but it involves people without history of excessive alcohol consumption. It is considered as the most common cause of liver enzyme abnormality in the west (1). Fatty liver disease causes a wide spectrum of liver disorders ranging from simple steatosis to liver cirrhosis and hepatocellular carcinoma (2). It is suggested that NAFLD increases all causes of death especially in patients with diabetes (3). The pathogenesis of NAFLD linked to the insulin resistance and hyperinsulinemia diabetes mellitus is reported in 18% - 45% of them; on the other hand NAFLD is observed in 49% - 75% of patients with diabetes (4, 5). NAFLD is closely related to metabolic syndrome, which increases its importance especially for systemic disorders and specifically cardiovascular diseases. Some studies showed evidence of subclinical atherosclerosis in patients with NAFLD including increased intimal media thickness of carotid arteries and abnormal vasodilatory response to changes in the rate of flow (5). But some other studies did not prove calcium increase in carotid arteries or increased intimal-media thickness (IMT) in such patients (6-8). However, a systematic review which evaluated results of seven observational studies with 3,497 patients confirmed that carotid plaques and IMT are significantly associated with increased alanine aminotransferase (ALT) and fatty liver on sonography (9). Several studies using sonography to diagnose NAFLD showed increased coronary atherosclerosis in diabetics with fatty liver disease (10, 11). In a large cohort including 3000 patients with diabetes, ischemic heart disease (IHD) was more common in NAFLD patients and it was introduced as an independent risk factor for IHD (11). Another cohort including 2083 male workers revealed increased risk of IHD in sonographically diagnosed NAFLD patients and it was an independent risk factor (12); still one more cohort using unexplained elevated ALT as suspected NAFLD revealed elevated mortality secondary to cardiovascular events in this group of patients (13). In spite of growing body of observational evidences addressing increased cardiovascular disease and mortality in patients with NAFLD, it is a matter of debate if it is an independent risk factor since other risk factors such as obesity, hyperlipidemia and diabetes mellitus are prevalent in this group of patients. An observational study randomly selected 623 patients with type 2 diabetes to evaluate the correlation between steatosis (using liver: spleen attenuation ratio of < 1.0 on computed tomography (CT) scan as diagnostic criteria) and indicators of cardiovascular diseases. NAFLD was associated with low high-density lipoproteins (HDL) cholesterol and higher triglycerides and C-reactive protein (CRP), but was not associated with coronary atherosclerosis (14).
2. Objectives
In order to assess the relationship between NAFLD and coronary atherosclerosis, the current study aimed to evaluate the prevalence of suspected NAFLD in patients with different degrees of coronary disorders by angiography.
3. Patients and Methods
3.1. Subjects
The patients were selected from the cases referred to angiography ward of Imam hospital of Ahvaz Jundishapur University due to suspected coronary heart disease. All of the participants were requested to sign an informed consent form and if they agreed to participate in the study, first a comprehensive history about past medical course of the subject was taken including the history of viral, metabolic, autoimmune and drug related chronic liver diseases. A detailed history about drug and drinking habits of the subjects was also taken. After a complete physical examination of all subjects, the body mass index (BMI) was calculated by dividing weight in kg by square of height in meter (m) at standing position (kg/m2). Obesity was defined as BMI ≥ 30.
Hypertension was considered in the subjects with systolic blood pressure over 140 mmHg and or diastolic pressure over 90 mmHg. Meticulous abdominal exam of chronic liver disease evidence was performed on all subjects.
Fasting blood was taken for laboratory measurements including: fasting blood glucose, triglycerides, total cholesterol, low-density lipoprotein (LDL) and high-density lipoprotein (HDL). When total serum cholesterol level was more than 200 mg/dL the patient was considered as a hypercholesterolemia case. Hypertriglyceridemia was defined as serum triglyceride level of 150 mg/dL or higher. A subject was labeled as a case of diabetes mellitus when being treated for diabetes mellitus or had fasting blood glucose more than 125 mg/dL or two hours post prandial glucose more than 200 mg/dL (or impaired glucose tolerance). Alanine aminotransferase (ALT) and aspartate aminotransferase (AST) were all measured by auto-analyzers (Hitachi 7050; Hitachi ltd, Tokyo, Japan). The level of 40 U/L was considered as the upper limit of normal for ALT and AST. If the patient had elevated liver enzyme another sample was selected to be checked for hepatitis B surface antigen (HBSAg), hepatitis B core antibody (HBCAb), hepatitis C virus antibody (HCV Ab), serum iron, total iron binding capacity (TIBC), serum ferritin, anti-smooth muscle Ab (ASMA), antinuclear Ab (ANA) and serum gamma globulin level (g/dL).
Serum ceruloplasmin was measured in subjects under 40 years old. Subjects were referred for liver sonography if they met the fallowing inclusion criteria: age over 18, no definite hepatic disorder and compliant for performing liver sonography.
Subjects taking ethanol or hepatotoxic drugs or known cases of viral, metabolic and autoimmune liver diseases were excluded. Subjects with any positive lab data indicating possibility of other potential liver diseases were also excluded.
3.2. Sonography
All subjects underwent abdominal sonography by an expert radiologist, unaware of their history using a Hitachi 3,500 sonography device (Hitachi ltd, Tokyo, Japan). Diagnosis of fatty liver was made if at least two of the fallowing criteria were met: 1- increased hepato-renal contrast; 2- deep attenuation; 3-brightness of liver and 4- blurring of liver vascular pattern (15, 16). Sonography reported a sensitivity of 89% and specificity of 93% for diagnosis of fatty liver disease (17). Subjects were labeled as suspected steatohepatitis if they had unexplained elevated ALT (> 40 U/L) and sonographic findings in favor of fatty liver.
3.3. Angiography
All subjects underwent coronary angiography using a Siemens Auixium device (Siemens ltd, 2006, Germany) and when more than 50% of a major coronary artery lumen was occluded the case was labeled as a subject with CAD. Subjects with CAD were divided into two groups: 1- mild CAD, if less than three major vessels were involved and the degree of stenosis was less than 70%; 2- severe CAD, if at least three vessels were stenotic or one or two vessels with more than 70% were stenosis (18).
3.4. Statistical Analysis
According to the angiography results, the subjects were divided into three groups: normal, mild and severe CAD. According to sonography and liver enzyme status subjects were divided into two groups of suspected of NAFLD and non-NAFLD. There was no significant difference regarding the basic characteristics of the subjects among the groups. Continues variable was reported as mean values ± standard deviation (SD) and compared between the groups using two-sample T-test. Categorical variable was reported as frequencies and compared using Chi-square test. P values of less than 0.05 were considered as significant.
4. Results
A total of 314 subjects were eligible for study; 161 (51.3%) of them were male and 153 (48.7%) were female. The mean age was 55.8 ± 9.4 years and mean body mass index (BMI) was 28.33 ± 3.15. Overall, sonography findings indicated that 93 subjects (29.6%) had fatty liver and 221 (70.4%) were normal. With the inclusion of elevated ALT, 68 (21.65%) of the subjects had NAFLD and 246 (78.34%) were normal. Means of triglyceride were 290 ± 10 and 230 ± 10 mg /dL in the NAFLD and without NAFLD (P = 0.03) groups, respectively. Means of LDL cholesterol were 170 ± 10 and 130 ± 10 mg/dL for the subjects with NAFLD and without NAFLD (P = 0.01), respectively (Table 1). A significantly greater number of subjects in the NAFLD group had hypertriglyceridemia, hypercholesterolemia and low HDL level compared to the subjects without NAFLD (Table 2).
| Variable | With NAFLD (N = 68) | Without NAFLD (N = 246) | P Value |
|---|---|---|---|
| Age, y | 55.2 ± 7.3 | 55.8 ± 9.4 | 0.2 |
| BMI, kg/m2 | 28.45 ± 3 | 27.7 ± 4 | 0.472 |
| Blood pressure, mmHg | 130/70 ± 1.5 | 135/78 ± 1.4 | 0.11 |
| Total cholesterol, mg/dL | 240 ± 8.5 | 250 ± 10.5 | 0.38.7 |
| LDL cholesterol, mg/dL | 170 ± 10 | 130 ± 10 | 0.01 |
| HDL cholesterol, mg/dL | 37 ± 10 | 35 ± 10 | 0.392 |
| Triglyceride, mg/dL | 290 ± 10 | 230 ± 12.5 | 0.03 |
| Fasting blood glucose, mg/dL | 160 ± 10 | 145 ± 10 | 0.361 |
Abbreviation: NAFLD, non-alcoholic fatty liver disease.
| Variable | With NAFLD (N = 68) | Without NAFLD (N = 246) | P Value |
|---|---|---|---|
| Diabetes mellitus | 32.35 | 27.24 | 0.407 |
| Male gender | 60.29 | 48.78 | 0.93 |
| Hypertriglyceridemia | 67.64 | 42.68 | 0.0001 |
| Hypercholesterolemia | 54.41 | 34.14 | 0.002 |
| LDL level > 100 mg/dL | 97.05 | 88.21 | 0.03 |
| LDL level > 130 mg/dL | 73.51 | 39.83 | 0.0001 |
| HDL level < 40 mg/Dl | 63.23 | 48.78 | 0.035 |
Abbreviation: NAFLD, non-alcoholic fatty liver disease.
After coronary angiography, 236 subjects (75.1%) had coronary artery disease and 78 subjects (24.9%) had normal coronary arteries. In the group of subjects with fatty liver, metabolic parameters were compared among those with normal coronary arteries and the subjects with CAD. In the group of subjects with CAD and fatty liver, the mean values of triglyceride, LDL cholesterol and FBS were 240 ± 10.5, 160 ± 6.9 and 170 ± 10.2 mg /dL, respectively. All of the factors were significantly greater in the subjects with CAD compared with the normal ones (P values < 0.05, < 0.02 and < 0.03 respectively) (Table 3). Prevalence of hypertension, low HDL level, diabetes and hypertriglyceridemia was significantly lower in subjects with coronary artery disease. When the subjects were compared in the normal and abnormal coronary artery groups, although NAFLD was more prevalent in the CAD group (23.3% vs. 16.66%), the difference was not statistically significant (P = 0.119) (Table 4).
| Variable | Fatty Liver Without CAD (N = 27) | Fatty Liver With CAD, (N = 66) | P Value |
|---|---|---|---|
| BMIa | 3.15 ± 28.3 | 3 ± 28.35 | 0.723 |
| Age, y | 7.3 ± 55.2 | 9 ± 55.8 | 0.63 |
| TGb, mg/dL | 9.5 ± 220 | 10.5 ± 240 | 0.05 |
| LDLc, mg/dL | 7.8 ± 130 | 6.9 ± 160 | 0.02 |
| FBSd, mg/dL | 10.4 ± 135 | 10.2 ± 170 | 0.03 |
Abbreviations: BMI, body mass index; FBS, fasting blood sugar; LDL, low-density lipoproteins; NAFLD, non-alcoholic fatty liver disease; TG, triglyceride.
| Variable | With CAD (N = 236) | Without CAD (N = 78) | P Value |
|---|---|---|---|
| Diabetes | 70.4 | 48.15 | 0.03 |
| Hypertension | 51.5 | 34.2 | 0.009 |
| Hypertriglyceridemia | 55.75 | 40.54 | 0.022 |
| Low HDL level | 53.23 | 37.09 | 0.013 |
| Suspected NAFLD | 23.3 | 16.66 | 0.119 |
Abbreviations: HDL, high-density lipoproteins; NAFLD, non-alcoholic fatty liver disease.
aValues are expressed as %.
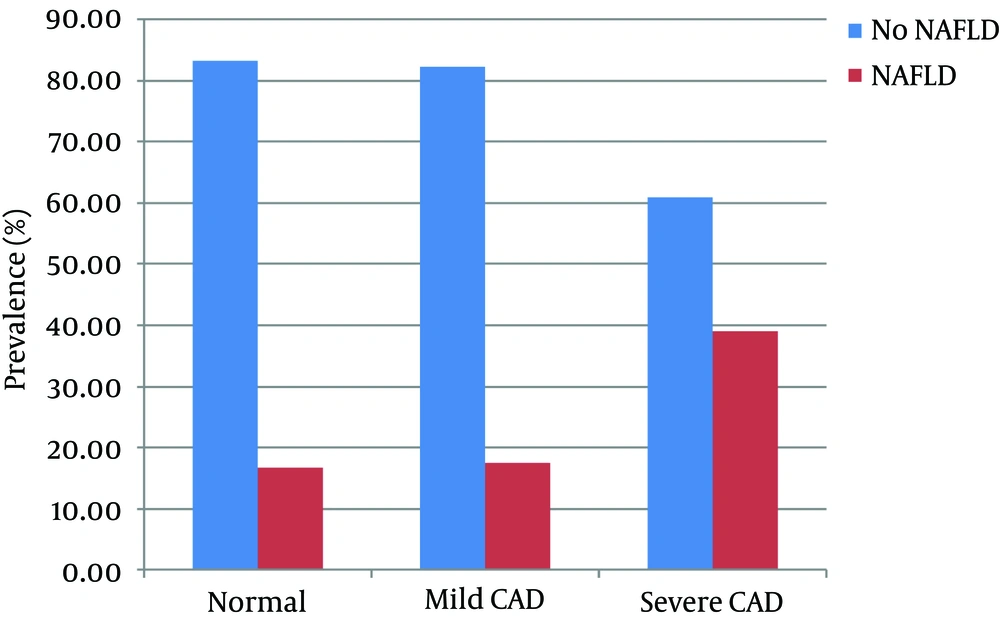
After ranking the subjects according to the degree of coronary artery stenosis, 78 subjects had no coronary disease and 13 (16.7%) were suspected of NAFLD, 172 cases had mild CAD that 17.44% of them had suspected NAFLD which was not significant compared to the subjects without CAD (P = 0.914; odd ratios = 1.0401; 95% CI: 0.5090 - 2.1253) but in 64 subjects with three vessel involvement (severe CAD) there were 39.1% NAFLD subjects which showed a significant difference in the prevalence of suspected NAFLD compared with normal coronary arteries group (P = 0.003, odd ratios = 3.1558; 95% CI: 1.4473 - 6.8812) (Figure 1).
5. Discussion
Non-alcoholic fatty liver disease (NAFLD) is a common disorder which has involved about 15% - 20% of general population and 70% - 90% of people with obesity and diabetes (1, 19). There is no doubt about negative effect of NAFLD on life expectancy (20, 21). Among patients with NAFLD the risk of coronary artery disease (CAD) is reported higher than that of general population in several studies (22). On the other hand, the risk factors for NAFLD and CAD are similar. In both groups the factors are associated with diabetes, obesity, hyperlipidemia and metabolic syndrome; therefore, risk of CAD may be an incidental phenomenon in these patients (23, 24).
The gold standard to diagnose NAFLD is liver biopsy. NAFLD is the cause of elevated liver enzyme in more than 80% of cases and if other potential etiologies are ruled out, the sensitivity of combining sonography and liver enzyme to diagnose NAFLD will increase (25). Moreover, NAFLD may reflect more advanced disorders than simple steatosis with more systemic complication (26). Results of the current case control study showed that subjects with CAD had higher mean fasting blood sugar, triglyceride and LDL cholesterol level than subjects without CAD. The prevalence of hypertension, hypertriglyceridemia and hypercholesterolemia was higher in subjects with CAD. On the other hand, subjects with suspected NAFLD had higher mean triglyceride and LDL-cholesterol levels than the control group. The prevalence of obesity, hypertriglyceridemia, hypercholesterolemia and low LDL-cholesterol were significantly higher in subjects with suspected NAFLD than the controls. After performing coronary angiography, 23.3% and 16.66% of the subjects with and without CAD respectively, had NAFLD. Although NAFLD seemed to be more prevalent in subjects with CAD, the difference was not significant. After ranking the subjects according to the degree of coronary artery involvement it was observed that compared with the control group the prevalence of suspected NAFLD was much higher in subjects with severe or three vessels involved CAD. But the prevalence of NAFLD in mild CAD group was lower and the difference was not statistically significant.
Most studies on the relationship between NAFLD and CAD arise from population studies and follow the complication of CAD. There were only few studies which directly evaluated the prevalence of angiographically proven CAD in subjects with NAFLD and a substantial body of evidence which used direct variables for cardiovascular involvement did not prove NAFLD as an independent risk factor. In a case –controlled study, Assay et al. reported higher prevalence of CAD in patients with NAFLD. They used CT scan to diagnose NAFLD and CT angiography to diagnose CAD (27). Petit et al. evaluated the correlation between NAFLD and carotid intimal- media thickness (IMT) in subjects with diabetes using magnetic resonance imaging (MRI) to measure liver fat content. They did not observe a correlation between liver fat content and carotid IMT and concluded that NAFLD is not a specific risk factor for cardiovascular disorder which is close to the current study observation (6). Another observation by McKimmie et al. using CT scan to evaluate coronary artery status, aortic and carotid calcium showed that NAFLD per se was not a risk factor for CAD but it reflected the consequences of general fat accumulation and subsequent inflammatory response. In that observation, similar to the current study, the patients with NAFLD showed higher percentage of hypercholesterolemia and hypertriglyceridemia (14). Several mechanisms are proposed for possible risk of CAD in patients with NAFLD including endothelial damage and dysfunction and oxidative stress; however, some studies that suggested NAFLD as a risk factor for CAD did not show increased markers of oxidative stress in such subjects (5, 28). The other possible mechanism is systemic inflammatory reactions. It is suggested that hepatic steatosis causes hepatic damage and secondary activation of n-Fk pathway which is responsible for increased inflammatory mediators such as interleukin 6 and tumor necrosis factors. These mediators have a substantial role on necroinflammatory process of non-alcoholic steatohepatitis (NASH) and may have a role in cardiovascular disease (29, 30). Some data suggested that the risk of CVD increases with the worsening of NAFLD necroinflammatory condition (31, 32). The current study did not perform biopsy to evaluate the increased risk of CAD in the study. However, in the group of subjects with severe CAD the prevalence of suspected NAFLD was greater than that of the subjects with normal angiography or mild CAD and the prevalence of NAFLD increased with progression in the severity of CAD (Figure 1). This observation may support the theory of common inflammatory response in liver and arteries.
In conclusion, the current study confirmed that NAFLD and CAD have common risk factors such as metabolic syndrome. Elevation in the prevalence of NAFLD was observed with progression in severity of CAD. However, the difference in the prevalence of NAFLD among subjects with mild CAD was not statistically significant. Therefore, further studies are necessary to clarify if the NAFLD is an independent risk factor or an epiphenomenon in the CAD setting.
The subjects had no liver biopsy specimen; therefore, the diagnosis of NASH cannot be definitely confirmed. Another problem was the small sample size of subjects with normal angiography compared to the subjects with CAD, since subjects were selected at a tertiary center from a group who had a high pretest probability for CAD.