1. Background
Cardiac failure is one of the most common diseases and has a considerable role in the health and treatment field (1). More than five million American people (older than 10 years) are suffering from cardiac failure, which has been expected to increase by 20% by 2030, in comparison with 2013 (2). In addition, the hospital staying rate of the patients has been increased by twice in comparison with the last two decades; today, it is introduced as one of the most important mortality factors between patients (3). According to the improvement of health in developing countries, cardiovascular disease has been considered more than before. In addition, studies show that mortality rates, due to heart disease, accounts for 15% - 30% and 50% in developing countries and industrialized countries of total mortality, respectively (4). Ahmadi et al. suggested that the incidence of heart failure in Iran was greater than other neighborhood countries, thus, the prevalence rate reported for this disease is 8% (5).
Patients are suffering from many disorders like respiratory disease, edema, pain, fatigue, nausea, and sleep disorders (6). All disorders can have an influence on patients performance (7). Quality of life is one of the most important factors in health care setting, especially in chronic diseases, and it is affected by economic condition, personal belief, and environment (8, 9). Quality of life has proven to be an important influence on both medical- and person-centered outcomes in patients with heart failure. Patients’ disability followed by the disease and worse quality of life cause more mortality and readmission rates than those who have a better quality of life (10, 11). Heart failure is potentially a serious disorder (12) and is more effective on the quality of life than other chronic diseases (13).
In last two decades interests in assessment and improvement of patients quality of life with chronic heart failure has been significantly increased (14). The main result of cardiovascular diseases is disabilities, social limitations, and depression (15). The results of Shojaei’s study suggested that cardiac failure has a negative impact on quality of life. Moreover, quality of life improvement, followed by the regular assessment of such patients, should be considered as one of the most important duties of the nursing team (16). Study findings of Khlilzade et al. suggested that patients’ low adjustment with their disease may decrease their quality of life (17).
One of the most important and effective factors, which have been discussed in nursing studies, is self-efficiency (18). Self-efficiency is one of the main structures of social-cognitive theory, which means how much a patient has self-confidence to perform their own abilities (19).
One of the important aspects of a person’s self-efficiency is how one person can have an effect on its own lifes’ outcomes by having control (20). The concept of self-efficacy, which is the main factor in the theory of social learning, was first developed by Bandura’s social psychology. Bandura introduced self-efficacy as a belief in the individual’s ability to organize and implement a series of actions required for reaching special goals (21). In the Bandura theory, four psychological processes, through which self-efficacy belief affects human performance, consists of cognitive, motivational, emotional, and selective processes. According to Banduras’ theory, self-efficacy addresses the judgments about how well a person can apply the methods required to deal with future conditions (22). In other words, although a person may have skills to perform an operation because of weak self-efficacy beliefs he/she will have an unsuccessful performance (23). Therefore, self-efficiency is a valuable tool for nurses in health-care facilities and patient’s self-efficiency assessment can increase the patient’s ability for self-care (24).
Many studies were conducted on the relationship between self-efficiency and quality of life. Kohno et al. suggested the effectiveness of interventions on self-efficacy for gastrointestinal cancer survivors and the influence of psychological factors such as quality of life, anxiety, and depression (25). The result of Middleton et al. showed that rehabilitation strategies may need to concentrate on improving quality of life by targeting factors like low self-efficacy (26). Regarding the results of the study that was conducted by Paryad et al. it seemed that more precise planning is needed to improve the self-efficacy of physical activity in patients with coronary artery disease (27).
Self-efficiency, as an effective factor on quality of life, emphasizes on the persons understanding of own skills for having a successful function (28). Self-efficiency may have an impact on self-care abilities and helps to decrease risk factors (29). In addition, self-efficiency has an important role in management of healthy behavior and compatibility with a healthy lifestyle in patients with chronic disease such as diabetes or cardiac disease (30, 31).
2. Objective
In regards to increase heart failure prevalence and mentioned studies above, understanding the effectiveness of quality of life on patient’s self-efficiency and limited studies that have been conducted on this field in Iran, the present study aimed to determine the relationship between quality of life and cardiovascular self-efficacy in patients with heart failure.
3. Methods
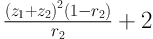
This research was a one-stage descriptive - correlation study that was conducted from February to April 2015 in hospitals affiliated in Isfahan University of Medical Sciences, in Iran. The sample size was calculated using Equation 1 was 227 patients. All 227 patients that were evaluated in the study, suffered from cardiac failure. The patients were randomly assigned to two groups. The inclusion criteria included assignment of consent form, suffering from class two or three of cardiac failure that was confirmed by a cardiologist, patients that were being 18 years or older, passed at least six months after diagnosis of heart failure, non-presence of other threatening physical illnesses such as mental retardation and dementia, self-awareness of their disease, being alert, and familiar with the Persian language (32, 33).
The information gathering tool was comprised of three parts: the first one containing the questions about demographic subjects and information related to the patient (including age, sex, and occupation, marital status, and education level, duration of illness, hospitalization times, and ejection fraction of the heart, diabetes, hypertension, and cholesterol disorders). The second one includes Sullivan’s self-efficacy questionnaire. This questionnaire is a 16-item scale with a score for each question ranging from zero to four and assesses the level of confidence and self-efficacy of patients about care, controlling disorders symptoms (0 = not at all confident, 1 = somewhat confident; 2 = moderately confident, 3 = very confident, and 4 = completely confident).
The cardiac self-efficiency with changing to appropriate variables were turned into 0-100 and its score was classified in three main groups of 0 - 33 (low), 34 - 66 (medium), and 67 - 100 (high). The cardiac self-efficiency of Sullivan is a valid and reliable questionnaire that has been approved by studies. In the study by Shamsizadeh the validity of this tool was approved and the internal consistency reliability was estimated using Cronbach’s alpha (0.977) (34). In recent studies, the Cronbach’s alpha coefficient of this tool was determined as 0.87 - 0.90 (35) and 0.77 (36).
The third part of the tool was the Ferrans and Powers quality of life index (1999), where its questions are arranged in two parts: measuring the importance and satisfaction of health and functioning, social and economic, psychological/spiritual, and family with values ranging from one to six. In the first part, the scale ranges from very unsatisfied [1] to very satisfied [6]. In the second part, the scale ranges from without any importance [1] to very important [6]. Every section contains 35 questions and the questions related to the importance and consensus was similar. The 35 items are distributed into the four subscales: health/functioning (15 items), social and economic (eight items), psychological/spiritual (seven items), and family (five items) (16, 37, 38). To determine the score for the quality of life level, first, the satisfaction scores must be recoded with the purpose of centering the scale of zero. This is done by subtracting 3.5 from satisfaction responses, which results in the following scores: -2.5, -1.5, -0.5, +0.5, +1.5, and +2.5 for scores that were originally 1, 2, 3, 4, 5, and 6, respectively. Second, the recoded satisfaction scores are weighted by their corresponding importance items, multiplying each item’s recoded value by the raw importance score (1, 2, 3, 4, 5, 6). Next, the total score is calculated by adding the weighted values of every response and then dividing by the total number of answered items. Up to this stage, the possible variation is from -15 to +15. To avoid the final score having a negative number, we add 15 to the obtained values, resulting in the total score of the instrument, which can vary from zero to 30. Accordingly, the score of nine-zero is considered as unfavorable quality of life, 19 - 10 is relatively favorable, and 20 - 30 is considered desirable (16). In recent studies, the Cronbach’s alpha coefficient of the Ferrans and Powers quality of life index was determined as 0.86 - 0.9 (16, 38).
The method of study conduction was so that the researcher, after acquiring the introduction issue from Nursing and Midwifery Faculty of Isfahan University of Medical Science, will refer to cardiovascular medical science university hospital-associated clinics. After presenting the introduction letter and explaining the study aim to the heads of the center and taking their agreements starts to making samples, the researcher goes to study the environment and after taking permissions from heads, if the patients were suitable to study, they were explained the purpose of this study and they would make their agreement to attend in the study. The completion of the three-part questionnaire for collecting patients’ information required an average 20 minutes. It should be noted that participants did not exchange any comments when answering questions. The present study was approved by the Research Council of the faculty of Nursing and Midwifery and the Ethics Committee of Isfahan University of Medical Sciences with code 293270. Objectives and methodology were explained for patients and informed consent was obtained.
3.1. Statistical Analysis
Data were analyzed by descriptive-analytic statistics using SPSS software version 22. In order to analyze the data, parametric tests, such as independent t test, One-way ANOVA, pearson correlation coefficient, and simple linear regression analysis were used. The significance level for statistical tests was equal to or less than 0.05. The independent t test is used to determine whether there is a statistically significant difference between the means in two different groups. The one-way analysis of variance (ANOVA) is used to determine whether there are any statistically significant differences between the means of two groups. Pearson correlation coefficient was a measure of the strength of a linear association between the scores of quality of life dimensions and the score of cardiac self-efficacy and drew a line of best fit through the data of two variables. Simple linear regression was a statistical method that allowed us to summarize and study relationships between two mentioned (quantitative) variables.
4. Results
The age average of research units was 59.47 with a standard deviation of 13.01 years. The average duration of the diseases was 7.25 ± 8.19, the average frequency of hospital-stay was 3.95 ± 2.76, and the average of ejection-fraction percent was 36.20 ± 12.90. Demographic characteristics of the patients were shown in Table 1.
| Demographic Characteristics and Disease Information | No. (%) |
|---|---|
| Sex | |
| Female | 77 (33.9) |
| Male | 150 (66.1) |
| Occupation | |
| Employee | 8 (3.5) |
| Freer | 65 (28.6) |
| Retired | 41 (18.1) |
| Manual worker | 5 (2.2) |
| Housewife | 52 (22.9) |
| Out of service | 18 (7.9) |
| Unemployed | 8 (3.5) |
| Others | 30 (13.2) |
| Marital status | |
| Single | 11 (4.8) |
| Married | 174 (76.7) |
| Divorst | 5 (2.2) |
| Died wife | 37 (16.3) |
| Level of education | |
| Illiterate | 95 (41.9) |
| Under the diploma | 86 (37.9) |
| Diploma | 33 (14.5) |
| Academic | 13 (5.7) |
| History of diabetes, hypertension and dyslipidemia | |
| Yes | 68 (29.9) |
| No | 159 (70.1) |
Frequency Distribution of Demographic Characteristics and Disease Information Units
The average score of cardiac self-efficiency was 58.45 ± 25.92, the average score of quality of life in importance aspect was 69.73 ± 18.72, and 82.76 ± 15.46 in the satisfaction aspect.
The results of this study suggested that there is a direct relation between quality of life score and cardiac self-efficiency (P < 0.001). In addition, Pearson correlation coefficients showed a direct and significant correlation between the scores of quality of life dimensions and the score of cardiac self-efficacy (in all cases, P < 0.001) (Table 2).
| Quality of Life Score and its Dimensions | Cardiac Self-Efficacy Score | |
|---|---|---|
| r | P Value | |
| Satisfaction | 0.409 | < 0.001 |
| Importance | 0.465 | < 0.001 |
Pearson Correlation Coefficients Between Cardiac Self-Efficacy Score with Quality of Life Score and its Dimensions
5. Discussion
This study with an attempt to determine the relation between quality of life with cardiac self-efficiency in patients with heart failure. The results of this study indicate that the cardiac self-efficiency average score was 58.45 ± 25.92, quality of life average score in importance aspect was 69.73 ± 18.72, and 82.76 ± 15.46 in the satisfaction aspect, which indicates the average level of cardiac self-efficiency between patients of heart failure. Results of the study indicated that by improving quality of life, the cardiac self-efficiency is also improved and that it has been confirmed by Middleton et al. They investigated the relation between quality of life and cardiac self-efficiency in patients with spinal injury and found that there is a direct relation between low level of quality of life and decreased self-efficiency in addition severity of pain. They also advised the necessity of quality of life to improve self-efficiency (26).
In addition, according to the results of this study, there is a direct relation between quality of life aspects and cardiac self-efficiency score. In this regard, the study results of Bagheri Saveh et al. suggested that there is a direct and significant relation between self-efficiency and self-care measures in patients with cardiac failure (39). In addition, the results of the study conducted by Boroumand et al. in attempt to determine the self-efficiency rate and relating factors in ischemic patients, suggested that there is a positive and significant relation between self-efficiency of ischemic patients with their regular participation in screening schedules (P = 0.03) (33).
Some studies investigate the self-efficiency as an effective factor on improving self-care behaviors (31, 40, 41). Holloway and Watson believed that self-efficacy is effective in modifying the health behaviors of a patient with cardiovascular disease (42). Findings of this study showed that self-efficiency has an indirect effect on quality of life, which was confirmed by Nekouei et al. who suggested that supportive factors such as general self-efficiency have positive effects on quality of life, however, psychological risk factors, such as stress, has negative effects on quality of life in patients with coronary diseases (43).
According to the findings of the present study, the participants have a medium self-efficiency rate, which was confirmed by the study of Hoseinzadeh et al. (44). In addition, results of the other studies indicate the relation between self-efficiency rate with quality of life of cardiac patients; the results of Smaeli et al. indicates that there is a significant correlation between quality of life and self-efficiency in patients with cardiac diseases (45). Furthermore, the results of the study of Shafiei et al. suggested that by increasing quality of life, self-efficiency also increases (46). Moreover, Jalilian et al. in their study, commented some appropriate mediating actions in order to increase the self-efficiency in cardiovascular patients in order to increase their quality of life and compatibility with disease (47).
However, the results of Chlebowy and Garvin studies suggested no significant relation between self-efficiency and self-care actions in diabetes patients (48).
Recent studies suggested that education with certain structures leads to promotion in cardiovascular patients’ self-efficiency. As the Baljani et al. study suggested, in order to research the effects of education in promoting cardiovascular, patients suggested the positive impact of education in overall score and self-efficient subgroups (24).
5.1. Limitation
The limitation of this study is in limited numbers of participants and the method of acquiring the investigable samples should made accessibly. For this purpose, we suggested that to generalize the findings to the community, patients with heart failure should be included in the future with randomized sampling and sample size.
The results of the present study suggested that the quality of life of patients with cardiac failure have positive and meaningful relation with their cardiac failure. Thus, by considering the significant role of the nursing team in taking care of patients with cardiovascular diseases, by planning and performing appropriate meditations, they are able to help them improve their quality of life by using meditations like targeted educations in order to promote their cardiac self-efficiency.
