1. Background
Multiple sclerosis (MS) is a chronic autoimmune disease, progressing in central nervous system that typically begins within the age range of 20 to 40 years. More females are diagnosed with MS than males (1). This disease is the third most common cause of neurological disabilities (2). According to the World Health Organization (WHO) report 2008, about 1.3 million people around the globe were diagnosed with MS (3). This number is increasingly growing and from 2008 to 2013, the number increased from 30 to 33 per 100000 (4). The rates of the prevalence of MS vary worldwide. Countries with higher number of diagnosis (more than 30 per 100000 people) are in north of Europe, Northern America, south of Canada, south of Australia, New Zealand, Iran, and Turkey, and the ones with lower rates (less than 5 per 100000) are countries in south of Europe, Japan, China, and Southern America (5). Incidence of MS is particularly high in the north of Scotland (in Orkney Islands) (6). The MS Association of Iran reported about 40000 patients with MS in the country (7). The number of patients with MS is higher in Isfahan than the other parts of the country, and Isfahan with 4250 patients has the highest prevalence in the Iran (8). Etemadifar et al. (9), reported the number of patients with MS in Hamedan province 1100. Patients with MS have many physical and mental problems that limit the presence of patients in health promotion activities and increase the secondary complications and limitations in independent life, which ultimately have a negative impact on patient’s quality of life (10).
Quality of life, with multiple measures such as physical, mental and social aspects, is used as an important indicator resulting from various researches regarding the health of the patients and effectiveness of the treatment process (11).
Chronic diseases such as MS cause various physical challenges such as blue vision, diplopia, muscle weakness, balance and coordination problems, sensory and cognitive disturbances, pain (medium to intense), memory loss, inability to focus, fatigue, tremor, dizziness, bowel problems, bladder and sexual dysfunction (8), swallowing and speech problem, impaired ability to regulate temperature (12), and paralysis of the hands and feet (6). A study by Lotfi et al., (cited by Agha Yousefi et al.) suggested sensory and vision disturbances as the most common symptoms among Iranian young adults with MS (13).
In addition to physical challenges, MS could trigger various psychological and mental illnesses in the patients. More studies found that due to chronic and unpredictable nature of this disease, patients with MS are more liable to depression, stress, and anxiety than the other problems such as cognitive disturbances and extreme irritability from which anxiety, stress, and depression are the most common prevalent ones (14, 15). About 48% of the patients are diagnosed with anxiety, stress, and depression within the first year of diagnosis (16). Stress, by itself, can exacerbate other symptoms caused by MS. It could also threaten other aspects of the patient’s life and lead to divorce, loss of job, and other difficulties in patients’ relationships (15). Depression in such patients could potentially lead to constant unhappiness, loss of hope for future, frequent mental images of disability, constant flow of negative thoughts, and in extreme cases, suicidal behavior (17). All of these negatively affect the patients’ quality of life, which could discourage them to follow treatment process, hence worsening the symptoms (18). The results of some studies showed that stress, anxiety, and depression symptoms in patients with MS were associated with relapse of the disease and a decrease in the quality of life of patients. In addition, having mental health can prevent the development of depression, anxiety, and stress in patients and, consequently, improve their quality of life and satisfaction (19).
According to the many problems of patients with MS, many researchers try to study and develop interventions to control such problems. Due to the urgency of taking measures to control the debilitating problems and improving the patients’ quality of life, drug therapy alone has no effect on the quality of life of such patients (20); therefore, other methods should be employed in addition to drug therapy. Today, many physicians recognize faith and spirituality as an important source of health and well-being; hence, they often know that they should consider patients' spiritual issues in the treatment process (18). Spirituality involves self-perceptions and a combination of personality factors and fundamental beliefs about perceiving meaning in life that these beliefs correlate to various aspects of life including social, physical and mental aspects (18). Spirituality is the aspect of human that shows the connection and unity with the universe and extends him beyond the limits of time and place and material interests (21).
Spirituality along with religious forces leads to a positive attitude toward the world and helps the individual to accept irreplaceable situations such illness and the individual hopes to improve life (22). They could build foundation for adaptability, hope, and healing for the patient. Spiritual treatment approaches encourage therapists to help the patients according to their religious beliefs and benefit from determinism to help patients (18). In addition, better performance could be achieved if the techniques are implemented in a group. Interaction with other patients helps patients be more aware of own situation (23).
Corey found that the following factors were important in the therapeutic progress:
1. Commonness: Patient does not see him/herself the only person with this disease.
2. Friendship: In a group, the patient perceives meaning when people in the group support each other.
3. Hope: Patients find hope when they see the other people that are at similar or worse conditions, can perceive a meaning in life, and have positive attitudes towards life (24).
Today, along with spirituality, the important issue that attracted the attention of psychologists and mental health professionals over the past few decades is the importance of spiritual health in humans. Spiritual health is one of the important aspects of health and the core of health in humans (25). Spiritual health is the only force that coordinates physical, mental, and social aspects of life and is necessary to adapt to the disease (26). According to the WHO, the human health has four main aspects including physical, mental, social, and spiritual and spiritual health is the most crucial one for development (27). Spiritual health has two aspects of religious health and existential health. Religious health is central to the quality and understanding of one's health from spiritual life, when it is linked with higher power, and existential health is related to the adaptation of individuals to society and themselves and to the social and mental concerns of individuals (28). Individuals with a high spiritual health can adapt to their problems. When spiritual health comes at a serious risk, the person may have mental disorders such as loneliness, anxiety, and feeling of futility (29).
The first research regarding the quality of life of people with MS was published in 1990. Many works are conducted ever since (16). Haresabadi et al. (1), reported in their study that the quality of life of patients with MS admitted to Ghaem Hospital, in Mashhad, was average. Heidari Sureshjani et al. (8), found a lower than average score for the quality of life of patients with MS in Isfahan. Tepavcevic et al. (29), and Bašić Kes et al. (30), reported a lower quality of life for patients with MS patients compared with others. Allahbakhshian et al. (31), showed a relationship between religious beliefs and spiritual health of patients with MS. Spiritual group treatment by Taghizade and Miralaee was very effective in females diagnosed with MS (18). Dehghani et al. (15), reported significantly high levels of stress, anxiety, and depression, which can endanger the health state. Mardani Valdani and Ghafari found in their study that various techniques such as logotherapy (increasing the responsibilities), transforming the patients’ beliefs towards life, and raising hope in life can help the patients with MS improve their quality of life both in physical and mental aspects (32). Khodaveisi et al. (20), showed that the Orem self-care-training model was beneficial in improving the quality of life of patients with MS. Beiske et al. (33), showed that patients with MS exhibited 31.4% and 19.3% depression and stress symptoms, respectively. Therefore, it can be concluded that patients with MS exhibit depression and stress, twice and three times as much as the healthy people, respectively, in Norway. Ashjazade et al. (4), showed that mental aspects of life in patients with MS were considerably lower than those of the healthy individuals. Nasiry Zarrin Ghabaee et al. (34), reported that spiritual health and religious beliefs could play an important role in improving the quality of life of in patients with MS. Akbari and Hossaini showed in their study a non-linear relationship between spiritual health and the areas of quality of life and mental health (35).
Nowadays, governments acknowledge that the improvement of quality of life is essential in socioeconomic development. Therefore, understanding the condition and quality of life features of patients with MS are crucial for intervention and treatment processes (36). Since MS is the second cause of youth disability in Iran (37), it is important to study the quality of life in patients with MS and the factors affecting it; also, studying the nonpharmacological interventions such as spiritual therapy, especially in group therapy, and using its results can help the therapists to deal with such patients. Unfortunately, there are not many studies on spiritual health and nonpharmacological intervention approaches in patients with MS. One of the specific features of the current study was simultaneous examination of group spirituality therapy on two aspects of quality of life and spiritual health of patients with MS.
As already mentioned, the current study aimed at investigating the effect of group spirituality therapy on quality of life of patients with MS in Ahvaz. The study hypotheses were as follows:
1. Group spirituality therapy improves the quality of life of patients with MS.
2. Group spirituality therapy improves the physical quality of life of patients with MS.
3. Group spirituality therapy improves the mental quality of life of patients with MS.
4. Group spirituality therapy improves the spiritual health of patients with MS.
2. Methods
The current semi-empirical study included experimental, control, and follow-up groups. Statistical population of the study consisted of all patients diagnosed with MS, but not in acute stage of the disease. The formula below was used to calculate the sample size. Accordingly, the sample size was set to 80 persons.
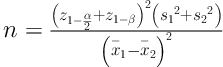
α = 0.05, β = 0.1,
Inclusion criteria were acquaintance with Farsi, age 18 years and older, diagnosed with MS by a physician at least three months prior to the study, scored low in quality of life and spiritual health, no signs of cognitive disturbances or other chronic diseases, and always accessible for the study. Exclusion criteria were participation in spiritual classes before entering the study, relapse during a hospitalization, and absence more than one session from the classes. The selected subjects were randomly divided into two experimental and control groups, each of which with 40 subjects.
2.1. Research Tools
Two questionnaires were employed; Msis-29 (The Multiple Sclerosis Impact Scale) and the Paloutzian-Ellison spiritual health (Paloutzian and Ellison's Spiritual Health Scale (1982)). Msis-29 is the only questionnaire specifically designed for patients with MS based on standard methods. It includes 29 questions in two subscales; the first 20 questions are on physical effects and the last nine questions on mental effects of MS on the patients. The scoring method of this questionnaire is based on a five-point Likert scale, ordered as never, very little, medium, relatively great, great (scored from 1 to 5) (4). Therefore, minimum and maximum scores are 29 and 145, respectively. A higher score shows a lower health state as well as quality of life. The overall score is categorized into the levels of quality of life; low (29 - 58), medium (58 - 87) and high (higher than 87). High reliability and validity of Msis-29 are proved in multiple studies. Ayatollahi et al. (38), obtained reliability of 0.95 and 0.85, for physical and mental aspects of Msis-29, respectively, using Cronbach’s alpha. Sadeghi et al. (39), obtained reliability of 0.92, 0.93, and 0.89 for overall, physical, and mental scales, respectively, using Cronbach’s alpha and 0.83, 0.92, and 0.89 for overall, physical, and mental scales, respectively, using compilation method.
The Paloutzian-Ellison Spiritual Health Scale consists of 20 questions that measures religious and existential health, each of which include 10 questions. Higher scores show both better religious and existential health. The scoring method of this questionnaire is based on a six-point Likert scale; totally disagree, disagree, fairly disagree, fairly agree, agree, totally agree, (scored from 1 to 6). This order is reversed in questions 1, 2, 5, 6, 9, 12, 13, 16, and 18; scores of ‘totally disagree’ and ‘totally agree’ correspond to 6 and 1, respectively. Therefore, the highest and lowest scores for each section are 10 and 60, respectively. As for the overall score, the minimum and maximum are 20 and 120, respectively. The scoring levels are divided into three categories, which are low (20 - 40), medium (41 - 99), and high (100 - 120) (40).
Validity and reliability of the Paloutzian-Ellison Scale were verified in various studies. Seyed Fatemi et al. (40), and Allahbakhshian et al. (31), verified the validity of this scale according to content validity. Seyed Fatemi et al. (40), obtained a Cronbach’s alpha of 0.82 for the reliability of the test. Dehshiri et al. (41), calculated Cronbach’s alpha for overall, religious, and existential health as 0.90, 0.82, and 0.87, respectively, and using re-examination calculated 0.85, 0.78, and 0.81, respectively.
2.2. Research Methodology
The study protocol was approved by the Ethics Committee of Research Department of Nursery and Midwifery, Ahvaz Jundishapour University (ethical code: IR.AJUMS.REC.1395.59). A total of 80 patients with MS were selected according to the inclusion and exclusion criteria from the patients in the MS association. First, the demographic, quality of life, and spiritual health questionnaires were provided to all selected patients in a pre-test stage; then the subjects were randomly divided into two groups of 40 subjects (experimental and control). Patients were assured that ethical considerations are respected and demographic information and research results remain confidential. According to the experts (religious experts, psychologists, and counselling experts) and obtained pre-test results, an intervention was developed for the experimental group. The intervention included face-to-face lectures and question-and-answer sessions. Educational interventions were performed to improve the subjects’ quality of life in five 60-minute sessions (Table 1).
| Session No. | Topic |
|---|---|
| First | Introduction to spiritual interventions and orientation |
| Second | Relationship with a higher being: spirituality and remembering the higher being (logotherapy with a religious approach, meaning of goals and understanding pain and life, concept of death, prayer and its effect on health, direct connection with the core of universe, mutual effect of body and mind on each other) with the help of a religious expert. |
| Third | Relationship with self: the role of spirituality in adapting with mental stress |
| Fourth | Relationship with nature and other people; spirituality and happiness |
| Fifth | Conclusion: explaining the experience of spiritual therapy and its effect, preparing the members to leave the group and utilizing the findings |
After group spirituality therapy sessions, the quality of life and spiritual health questionnaires were again provided both to the experimental and control groups in the form of post-test stage. After three months, as a follow-up procedure, patients were tested again (quality of life and spiritual health).
2.3. Data Analyse
Data were statistically analyzed by descriptive (frequency, mean, standard deviation) and inferential statistics (repeated measures ANOVA) with SPSS version 19.
3. Results
The demographic characteristics of the sample are shown in Table 2. The analysis of Table 2 showed that the most frequent demographic features were: 88.8% female, 46.3% aged 40 to 60 years, 65% married, 40% secondary-school education, 52.5% housewives, 27.5% diagnosed for less than two years, and 55% with average economic status.
| Variable | Frequency | Percent |
|---|---|---|
| Gender | ||
| Female | 71 | 88.8 |
| Male | 9 | 11.2 |
| Age, y | ||
| 20 - 30 | 24 | 30.0 |
| 31 - 40 | 37 | 46.3 |
| 41 - 50 | 16 | 20.0 |
| above 50 | 3 | 3.8 |
| Marital status | ||
| Single | 22 | 27.5 |
| Married | 52 | 65.0 |
| Divorced | 4 | 5.0 |
| Widowed | 2 | 2.5 |
| Education | ||
| Illiterate | 1 | 1.3 |
| Elementary school | 7 | 8.8 |
| High school | 32 | 40.0 |
| Diploma | 19 | 23.8 |
| Bachelor | 18 | 22.5 |
| Master’s degree | 3 | 3.8 |
| Job | ||
| Labourer | 1 | 1.3 |
| Clerk | 20 | 25 |
| Housewife | 42 | 52.5 |
| Jobless | 4 | 5 |
| Self-employed | 4 | 5 |
| Others | 9 | 11.3 |
| Disease duration, mn | ||
| < 1 | 17 | 21.3 |
| < 2 | 22 | 27.5 |
| < 5 | 13 | 16.3 |
| < 6 | 21 | 26.3 |
| Others | 7 | 8.8 |
| Economic status | ||
| Weak | 27 | 33.8 |
| Average | 44 | 55.0 |
| Good | 9 | 11.3 |
| Excellent | 0 | 0 |
Results of central tendency and measures of variability of the experimental and control groups are shown in Table 3. This table indicated the average score for quality of life of the experimental group in pre-test as 49.32, which was in the low level quality of life (score 29 - 58), but, after the educational intervention, they scored 59.66 and 59.32, in post-test and follow-up, respectively, which fell into the medium level of quality of life (score 58 - 87).
| Group | Number | Pre-Treatment Test | Post-Treatment Test | Follow-Up |
|---|---|---|---|---|
| Experimental | ||||
| Physical aspect | 40 | 31.15 ± 6.323 | 38.13 ± 6.039 | 36.92 ± 5.876 |
| Mental aspect | 40 | 18.17 ± 5.272 | 21.53 ± 4.867 | 22.40 ± 4.361 |
| Quality of life | 40 | 49.32 ± 4.745 | 59.66 ± 3.286 | 59.32 ± 5.802 |
| Spiritual health | 40 | 73.70 ± 8.870 | 82.00 ± 10.286 | 80.10 ± 10.789 |
| Control | ||||
| Physical aspect | 40 | 32.28 ± 7.035 | 31.98 ± 4.371 | 32.73 ± 9.287 |
| Mental aspect | 40 | 18.30 ± 4.794 | 18.18 ± 4.825 | 16.70 ± 2.803 |
| Quality of life | 40 | 50.58 ± 6.553 | 50.16 ± 5.029 | 49.43 ± 5.611 |
| Spiritual health | 40 | 75.88 ± 10.564 | 76.50 ± 8.659 | 72.85 ± 6.146 |
a Values are expressed as mean ± SD.
The average score of spiritual health in the experimental group showed that the average score of post-test (82.00) and follow-up (80.10) were more than that of the pre-test (73.70); average scores of the pre-test, post-test, and follow-up were at the moderate level (scores 41 - 99).
Results of central tendency and measures of variability of the control group showed the average quality of life scores 50.58, 50.16, and 49.43 for pre-test, post-test, and follow-up, respectively, which fell in the low level (scores 29 - 58).
The average score of spiritual health in the control group showed that the average scores of 75.88, 76.50, and 72.85 for the pre-test, post-test, and follow-up, respectively, fell in the moderate level (scores 41 - 99).
In order to compare the quality of life test results between the experimental and control groups in pre-test, post-test, and follow-up, analysis of repeated measures ANOVA was employed (Table 4). Table 5 indicated a significant difference between quality of life of the experimental group in the pre-test with those of post-test and follow-up (F = 18.698 and P < 0.05); therefore, it can be concluded with 95% confidence interval that the group spirituality therapy had a significant effect on the quality of life of the patients with MS. This conclusion verified the first hypothesis.
| Group | Stage of the Study | Repeated Measures ANOVA | |||
|---|---|---|---|---|---|
| Pre-Treatment Test | Post-Treatment Test | Follow-Up | F | P Value | |
| Experimental | |||||
| Quality of life | 49.32 ± /4.745 | 59.66 ± 3.286 | 5.802 ± 59.32 | 18.698 | 0.013a |
| Physical aspect | 31.15 ± 6.323 | 38.13 ± 6.039 | 36.92 ± 5.876 | 35.289 | 0.001a |
| Mental aspect | 18.17 ± 5.272 | 21.53 ± 4.867 | 4.361 ± 22.40 | 33.835 | 0.001a |
| Control | |||||
| Quality of life | 50.58 ± 6.553 | 50.16 ± 5.029 | 5.611 ± 49.43 | 2.536 | 0.338 |
| Physical aspect | 32.28 ± 7.035 | 31.98 ± 4.371 | 32.73 ± 9.287 | 1.636 | 0.201 |
| Mental aspect | 18.30 ± 4.794 | 18.18 ± 4.825 | 2.803 ± 16.70 | 14.453 | 0.105 |
a P value < 0.05.
| Group | Stage of the Study | Repeated Measures ANOVA | |||
|---|---|---|---|---|---|
| Pre-Treatment Test | Post-Treatment Test | Follow-Up | F | P Value | |
| Experimental | 73.70 ± 8.870 | 82.00 ± 10.286 | 80.10 ± 10.789 | 13.909 | 0.001a |
| Control | 75.88 ± 10.564 | 76.50 ± 8.659 | 72.85 ± 6.146 | 2.472 | 0.091 |
a P value < 0.05.
Moreover, Table 4 indicated no difference between the quality of life of the control group in pre-test, and those of the post-test and follow-up (F = 2.536 and P > 0.05).
In order to compare the test results for physical aspect of quality of life between the experimental and control groups in the pre-test, post-test, and follow-up, analysis of repeated measures ANOVA was employed (Table 4). Results of this table indicated significant difference in physical aspect of the quality of life in the experimental group between pre-test, post-test, and follow-up (F = 35.289 and P < 0.05); therefore, it can be concluded with 95% CI that the group spirituality therapy had a significant effect on physical aspect of quality of life in the patients with MS. This result verified the second hypothesis. Also, other results in this table showed no difference regarding the physical aspect of the quality of life of the control group in the pre-test, post-test, an follow-up (F = 1.636 and P > 0.05).
Repeated measures ANOVA analysis was implemented to compare the mental aspects of patients’ quality of life (Table 4). Results of this table indicated significant difference in mental aspect of the quality of life in the experimental group between pre-test, post-test, and follow-up (F = 33.835 and P < 0.05); therefore, it can be concluded with 95% CI that the group spirituality therapy had a significant effect on mental aspect of quality of life in patients with MS. This result verified the third hypothesis. Also, other results in this table showed no difference in the mental aspect of quality of life in the control group based on pre-test, post-test, and follow-up results (F = 14.453 and P > 0.05).
In order to compare the test results of spiritual health of patients in the experimental and control groups in pre-test, post-test, and follow-up, repeated measures ANOVA was employed (Table 5). Table 5 indicated a significant difference in spiritual health of the experimental group among pre-test, post-test, and follow-up results (F = 13.909 and P < 0.05); thus, it can be concluded with 95% CI that the group spirituality therapy had a significant effect on spiritual health. This result verified the fourth hypothesis. Also, other results in this table showed no significant difference in the spiritual health of the control group among pre-test, post-test, and follow-up results (F = 2.472 and P > 0.05).
4. Discussion
Results of the current study showed that the quality of life of the patients with MS under study as well as their spiritual health was average. Physical aspect of the quality of life had a higher average than that of the mental aspect.
Regarding the first hypothesis, results showed a significant difference between average scores of quality of life in pre-test, post-test, and follow-up of experimental and control groups (P < 0.05); hence, it verified the hypothesis. Thus, it suggested the positive impact of the group spirituality therapy on improving the quality of life of the patients in the experimental group. It was in accordance with the results of other studies such as Pirasteh Motlagh and Nikmanesh (42), Taghizade and Miralaee (18), Kamian et al. (43), Cunningham (44), Finkelstein et al. (45), and Basavaraj et al. (46).
Therefore, it can be concluded that one of the most effective methods to improve the quality of life in patients with MS is spiritual therapy. Today, many physicians acknowledge spiritual beliefs of the patients as an important source to improve the patients’ health, and therefore, attempt to address them in their patients (18). Spirituality consists of self-esteem, a combination of personality traits and fundamental beliefs about perceiving a meaning in life. These beliefs are linked to various aspects of life such as social, physical, and mental (14). Since MS is the second most common cause of disability in young adults in Iran (37), non-medicinal methods such as spiritual therapy, along with medicinal treatment, could play a significant role to improve the quality of life in patients with MS. This statement was verified by the current and other studies.
Regarding the second hypothesis, results showed a significant difference between the average score of physical aspect of quality of life in the pre-test, post-test, and follow-up of experimental and control groups (P < 0.05); hence the hypothesis was verified. Thus, it suggested that the group spirituality therapy had positive impact on the physical aspect of quality of life of the patients in the experimental group. The results of current study were in accordance with those of the studies conducted by Taraghi et al. (36) and Haresabadi et al. (1).
Furthermore, several other studies showed that patients with chronic diseases use spirituality as a way to adapt to the disease, create a sense of meaning and purpose in life, and reduce the sense of suffering caused by the disease (15).
Spirituality along with religious forces leads to a positive attitude toward the world and helps individuals to accept irreplaceable situations such as illness and they hope for a better life. Spiritual support and religious resources and their strong interrelationship can improve the quality of life and interpersonal support and reduce the severity of symptoms, which has beneficial results for medical and therapeutic care (47). Therefore, according to the current and other studies, it can be deduced that spiritual therapy could have significant impact on improving physical aspect of quality of life in patients with MS.
Regarding the third hypothesis, the obtained results showed a significant difference between average score of mental aspect of quality of life in pre-test, post-test, and follow-up of the experimental and control groups (P < 0.05); hence, the hypothesis was verified. Thus, the positive impact of the group spirituality therapy on the mental aspect of quality of life of the patients in experimental group was suggested. The current study result was in accordance with those of other studies such as Seyed Fatemi et al. (40), Allahbakhshian et al. (31), Madrani Valndai and Ghafari (32), Nasiry Zarrin Ghabaee et al. (34), Ghahari et al. (48), and Bolhari et al. (23).
Chronic diseases such as MS, in addition to physical difficulties, cause mental disorders in patients (14). Studies show that 50% - 60% of patients with MS have depression and 37% - 40% of them have stress, which greatly affect the quality of life of such patients (7). Stress could exacerbate the symptoms, threaten the patients’ personal life, and lead to divorce, loss of job, and family conflicts (15).
The results of some researches showed that stress, anxiety, and depression symptoms in patients with MS correlate with the relapse of disease and reduced quality of life. Moreover, mental health can prevent depression, anxiety, and stress in patients and improve their quality of life and satisfaction (49).
As referred to earlier, one of the effective methods to increase the quality of life in patients with MS is spiritual therapy. Spirituality is an aspect of human beings that helps the person find connection with the world and be integrated with it. It gives them hope (20). It can help the person cope with difficult situations; it is a source of power, healing, and hope, and can help the patients perceive their illness as an inevitable experience they should endure. By assisting the patient to imagine positive pictures of their illness, it helps the patients adapt to challenges of their illness (18).
The results of the current and other studies could deduce that using spiritual therapy could be beneficial for patients with MS by improving their quality of life, especially in mental aspect.
Regarding the third hypothesis, results showed a significant difference between average scores of mental aspect of quality of life in pre-test, post-test and follow-up of experimental and control groups (P < 0.05); hence, the hypothesis was verified. Thus, the positive impact of the group spirituality therapy on the mental aspect of quality of life was observed in the experimental group subjects. This is in accordance with other studies such as Rezaei et al. (50) and Fouladvandi et al. (51).
Patients with improved spiritual health could effectively adapt with their disease, even with the last stages of their disease. Some believe that without spiritual health, other aspects of health state cannot emerge well and the developing disturbances could cause mental disorders, depression and futility, which hinder the patient to reach higher levels of quality of life (50). According to Fouladvani et al. (51), there is a tight correlation between spiritual health and the patients’ tendency toward receiving spiritual care. A positive attitude towards spiritual care correlates with spiritual health.
Spiritual health along with other facets of health state (physical, mental, and social), acts as a driving force to integrate all inner powers and could eventually help patients adapt with the disease (51). Therefore, spiritual therapy, as an effective means, could improve spiritual health of patients with chronic diseases such as MS. Findings of the current study, along with other studies, indicated that using spiritual therapy could significantly affect spiritual health of patients with MS.
4.1. Conclusion
The overall conclusion of the current study indicated that group spirituality training can improve the quality of life and spiritual health of patients with MS.
4.2. Limitations
Since the research was performed on patients with MS, taking samples and teaching them was one of the main limitations as well the lack of cooperation of patients to complete the questionnaires.
