1. Background
Stroke is the third common cause of death, as well as the cause of severe and long-term inability, in the world (1, 2). In the Global Burden of Disease study, it was estimated that 15 million people suffer from stroke every year, of which 5.5 million people die and 5 million people live with permanent disability (3). Evidence indicates a higher incidence of stroke in Iran than in Western countries.
In addition, a stroke occurs at a younger age in Iran than in other countries (4). The results of a study conducted in Isfahan to assess the hospital admission rate from 2000 to 2003 showed that the rate of admission increased from 84.16 to 103.33 per 100000 population, but the mortality rate remained constant at 32% (4). Following an episode of stroke, 35 to 45% of patients become relatively or completely dependent on other people to meet their needs in daily life (5). For reducing the hospital stay, the families are expected to take more responsibility for patient care in the recovery period (6). Therefore, patients with stroke become dependent on the family after discharge from hospital to meet their physical and emotional needs (7). Indeed, their families play an important role in caring for them (8).
Care by family members has become an integral part of many health systems since most people in the community devote a significant time to care for their loved ones (spouses, parents, and children) (9). The need for economizing the health care system has led to programs that reduce the length of hospitalization. In addition, patients increasingly express that they tend to be cared for at home rather than at the hospital. These factors cause patients to stay home longer before being admitted or return home sooner often with high levels of dependence and disability (10). Although home-based care is effective in terms of cost for the health care system, the increased dependence on family members can cause high levels of chronic stress, which can lead to physical and mental illness to family members (11). Caregivers who have serious health problems often cannot perform long-term care (10). Caring for patients by family members can have a profound effect on all aspects of everyday life. Therefore, many caregivers endure a significant burden, especially when they are engaged in other activities.
Family caregivers become an active member of the healthcare team without preparation or with very little preparation and sometimes they experience severe conditions. These caregivers do not have the resources or skills needed to play this complex and new role, which may include activities related to daily life, giving medication, and financial and mental support (12). Therefore, taking care of patients may be severe and onerous. It has recently been reported that caregivers’ older spouses may have health complaints that increase their risk of death (10). The results of studies indicate that more hours of care are associated with the deterioration of physical and mental health of caregivers and the increased burden of care responsibility (13). Caregivers also experience sleep disorder (14, 15). In addition, long-term care can cause depression, avoidance of community, and lower quality of caregivers’ lives (12).
Caring for a stroke patient is a stressful task for the caregiver. The duration of caring is long and the responsibility of care is wide and extensive, facing many caregivers with multiple problems in caring (16). The results of a study showed that managing daily life activities and patients’ cognitive, behavioral, and emotional changes are some of the important problems of patients’ family. Physical, emotional, cognitive, and behavioral changes in patients are frightening for families and caregivers are skeptical about how to manage these problems (17). The caregivers should quickly adapt to a sudden change in motor status, communication skills, mood, and personality of the patient and the burden of care can be very high for them (18). Patients’ family should be compatible with the shock that an independent and capable person becomes suddenly dependent on others to meet his/her needs. However, due to the acute nature of the disease, caregivers accept this role suddenly with the least readiness (19). The results of studies indicate the decreased quality of life (20), high burden of responsibility (9), decreased physical and emotional health (17, 21, 22), increased depression (20, 23), and the feeling of pressure (24) in caregivers of stroke patients and the decreased marital satisfaction in spouses’ caregivers (25).
Despite the high prevalence of stroke and the important role of caregivers in meeting the needs of patients, the needs of caregivers of stroke patients have not been taken into account so far. Although some studies have been conducted on the caregivers of stroke patients, most of these studies have been conducted with inadequate design and the nature or meaning of life experience and caring for stroke patients has not been studied. According to the important role of nurses in protecting patients and family members and the significant impact of people’s experiences on their lives, the nurses need to be aware of this situation to provide proper care.
2. Objectives
The aim of this study was to review the experiences of stroke patients’ caregivers to attain a deeper understating of caregivers’ experiences and meet their needs by providing nursing care. It can also be a scientific and practical development of nursing.
3. Methods
This is a qualitative descriptive phenomenological study. The study setting included the Internal Departments of Neuroscience at Al-Zahra and Kashani hospitals, as well as Al-Zahra Rehabilitation Center and Neurologists’ offices in Isfahan, Iran. The researchers referred to the settings for the initial selection of participants and selected a place for interviewing with the participants’ consent. Participants in this study were the caregivers of stroke patients. The requirements for participating in the study included a confirmed diagnosis of a family member with stroke by a neurologist, willingness to participate in research, being a family member of the stroke patient, being able to participate in interviews and transfer information and experiences. The caregivers also should have had a major role in caring for the stroke patient. A purposive sampling method was followed to recruit a sample with maximum variation (any stroke, any age, any level of literacy, any occupation, both genders, etc.). To maximize the diversity of participants and gain first-stage and long-term caregiver experiences, the researchers selected the participants from the Internal Neuroscience Departments among those whose patients had been diagnosed with stroke for the first time or referred to the hospital for rehabilitation or follow-up visits. The researchers continued the sampling until data saturation, which reached with the selection of seven participants in this study.
In this study, semi-structured interviews were used to gather information. The researcher referred to Al-Zahra Hospital, Rehabilitation Clinic for stroke patients, and the Physiotherapy Unit at Kashani Hospital after obtaining necessary permissions and receiving a letter from the Faculty of Nursing and Midwifery. In accordance with the criteria for participating in the study, the researcher selected the participants. After obtaining the initial agreement and written consent of the participant, the researcher selected a place and time for the interview with the participant’s agreement and then held the interviews. Kashani Hospital was the place for the interviews. Before the interviews, the researcher, while introducing himself and expressing the purpose of research, stated that their conversations would be recorded, their recordings and personal details would remain confidential to the researcher, and they may withdraw from the interviews at any time they wished. Subsequently, they were allowed to conduct further interviews to clarify the information. Therefore, each of the seven participants was interviewed 3 - 5 times before receiving comprehensive information. Sample interview questions included: (1) What are your experiences of taking care of your family member? and (2) How do you care for your patient? By answering these questions, they described their experiences in this area and explained how they acted after they had accepted the care of their family members. When there was a need to clarify the information in a particular context, other questions were used to get a deeper understanding. The average duration of the interviews was 50 minutes in the range of 20 minutes to 90 minutes.
After completing an interview, the tape was carefully listened by the researchers and transcribed verbatim. After conducting the analysis steps on each interview, to ensure the correctness of the researchers’ interpretation, the researchers contacted the participants again and the correctness of the interpretations was examined with their opinion and, if necessary, the needed changes were made. After the completion of the analysis, the interviews and extracted concepts were given to some colleagues to strengthen the findings.
Data analysis was performed on the basis of Colaizzi’s seven-stage method, as follows:
1. Reading all the descriptions and stories of the participants and sympathy with them.
2. Researchers extracted the words and sentences associated with the phenomenon under study.
3. Conceptualizing the extracted important sentences.
4. Specific categorization of concepts based on related subjects:
- Essential descriptions for the reliability of the content.
- Disregarding materials that were irrelevant to the goals of the study.
5. Combining all the extracted beliefs as a comprehensive description, including all the details of the phenomenon under study.
6. Summarizing the comprehensive description of the phenomenon as a real and concrete description.
7. In the final stage, the researchers referred to the participants in order to clarify the opinions based on the research findings and validate the findings.
The researchers used a long-term involvement to perform validation. In this way, the researchers conducted a telephone interview with a number of participants, in order to provide a deep understanding of each participant. In order to receive feedback from participants, the comments received from each interview were returned to each participant for review. For investigating the peers, the interviews were studied by researchers’ colleagues (5 faculty members (assistant professors) with more than 10 years of experience in neurology and specialist departments). For conformability, the researchers provided the data to their colleagues for verifying the authenticity of the data encoding process. For transfer, the researchers described precisely and purposefully the research process and the activities carried out in the course of research. The dependence of the data was determined in such a way that the data obtained from the interview were also obtained in patients’ observations and narratives. In total, 7 participants were interviewed, each taking an average of 1 - 2 hours.
4. Results
Of seven participants in this study, three were males and four were females aged 27 to 50 years (mean: 38.5 years). There were five married participants and two single participants; four participants were employees and three were housekeepers. All participants were taking care of their patients for more than a month (Table 1).
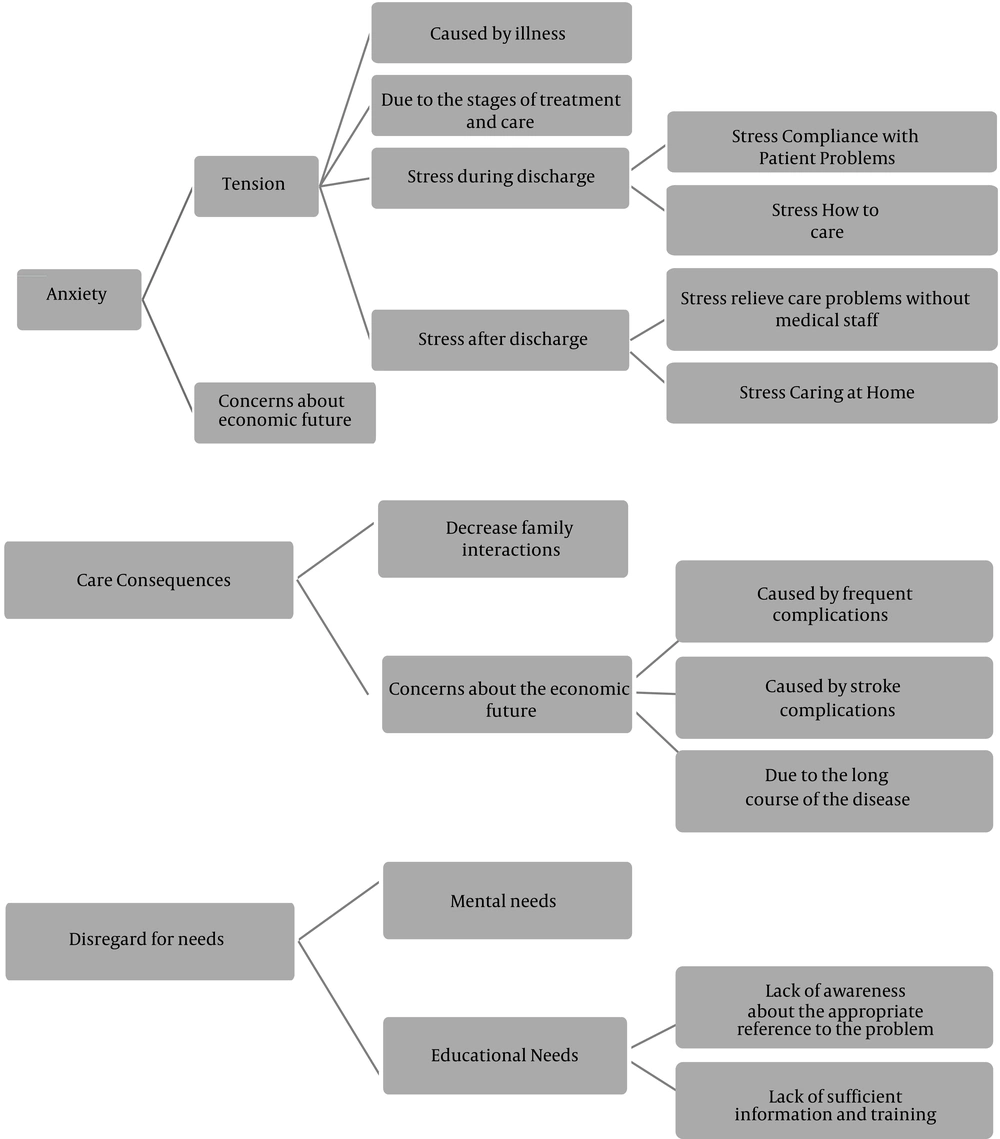
The participants’ experiences in this research reflected their needs and the responses of the treatment team to these needs. The findings of this study were expressed in three main categories of anxiety (stress, anxiety about the economic future), outcomes of care (fatigue, decreased family interactions), and neglected needs (psychological needs, educational needs) (Figure 1).
| Sex | Age | Occupation | Marital Status | Patient’s Relativity with Participant | Duration of Stroke |
|---|---|---|---|---|---|
| Female | 40 | Housewife | Married | Father | Six months |
| Female | 27 | Housewife | Single | Mother | One year |
| Female | 35 | Employee | Married | Mother | Three months |
| Female | 42 | Housewife | Married | Husband | One year |
| Male | 35 | Employee | Married | Father | One year |
| Male | 50 | Employee | Married | Wife | One year |
| Male | 30 | Employee | Single | Father | Seven months |
The Main Characteristics of the Participants in the Study
The present research was conducted with the aim of describing the experiences of caregivers of patients during the care period.
4.1. Anxiety
Some experiences of the caregivers of stroke patients were about caregivers’ anxiety, categorized into two subclasses of tension and economic future anxiety.
4.1.1. Tension and Stress
Family care of patients suffering from stroke, similar to taking care of other chronic debilitating diseases, creates much stress for the caregiver and the patient’s family because the patient’s biological, social, and mental needs overtake the caregiver’s needs.
One of the causes of tension in caregivers was exposure to a patient as a family member. Caregivers of stroke patients experienced much stress in the onset of symptoms and signs of the disease due to the acute nature of the disease.
“First, I told myself why this happened to us ... I just was taken aback ... My father had been talking to me about an hour before.” (A 40-year-old woman caring for a patient with stroke for six months).
“When I got into the room, I met my mother’s lifelessness a moment and my world was broken ... I did not know for a while what I was doing ... I was overshadowed” (A 27-year-old woman caring for a patient with stroke for a year).
The stress was induced in the caregivers at the patient’s hospitalization and discharge. At the time of the patient’s admission to the hospital, performing diagnostic procedures or caring by family members caused stress to caregivers.
“At the hospital, some nights my mother and I did not have a problem; meanwhile, the tests frightened us, mornings when to change the bedsheets.” (A 35-year-old woman caring for a patient with stroke for three months).
On the other hand, at the discharge time, caring and compatibility with the patient’s problems caused stress to caregivers.
“When we wanted to be discharged, I was frightened about what to do with his eating ... How to move? ... How do we get the car?” (A 35-year-old women caring for a patient with stroke for a year).
The proper taking care of the patient at home and the possible problems were other concerns for caregivers.
“After we went home, I was careful about everything that was happening every day and that everything was right. The nights were so bad. On the one hand, I wanted to sleep and on the other hand, I was afraid that something would happen.” (A 40-year-old woman caring for a patient with stroke for six months).
4.1.2. Concerns about Economic Future
In addition to the cost of the main treatment (specialist physician, physiotherapist) for improving the motor status, preventing deformity and limb pain, skin health, eliminating perceptual limitations, preventing respiratory infections, and controlling urination and stools, the patient caregivers are also forced to pay frequent expenses, while the family itself has its own everyday needs. Since there is no support system, caregivers are worried about economic needs.
“... since he had a stroke, he became very weak; I cared a lot, but his lungs were infected ... His back was bruised ... One man goes to dress, one for physiotherapy; its cost is high, these months all the savings are spending. Then, I’ll decide what to do.” (A 42-year-old woman caring for a patient with stroke for a year).
4.2. Care Consequences
Following taking care of a patient, the caregivers experience some problems that were classified under the subclasses of fatigue and family interaction decrease.
4.2.1. Fatigue
Due to the prolonged course of stroke and the complications caused by the disease in all systems of the body, the caregivers will get tired as a result of caring for the patient, the events that occur and the knowledge they have reached about the steps should be taken for recovery.
“When my mom gets a lung infection, the doctor should come and go ... I take medication ... physiotherapy ... then she gets a little better. I need to be careful with her to eat well to remain in good condition; when she gets sick again or I see suddenly she’s got a wound on the back, I just want to weep mournfully. I'm so tired.” (A 27-year-old woman caring for a patient with stroke for a year).
4.2.2. Decreased Family Interactions
Due to patient conditions, the special diet, motor system defects, urinary and stool control, special effects of stroke (respiratory diseases, etc.) and patient proximity to caregivers, the caregivers somewhat advocate for the current situation and reduce family interaction as much as possible to maintain patient recovery conditions and prevent the patient from getting worse.
“Because my mom needs to use the toilet with my help, and she only feels comfortable at my house, and actually, it troubles less, we often go at long intervals to see our families for too short.” (A 27-year-old woman caring for an old stroke patient).
“... since a stroke occurred for him, he has a headache in disturbance, we go at long intervals to parties” (a 40-year-old woman caring for a patient with stroke for six months).
“People who have a stroke get tired in the crowd ... It’s very difficult for them to sleep. We do not bring them anywhere for their being comfortable.” (A 42-year-old woman caring for a stroke patient for a year).
4.3. Disregard Needs
A part of the caregivers’ experiences was related to their neglected needs by the health system, classified into two subclasses of psychological needs and educational needs.
4.3.1. Psychological Needs
One of the needs of caregivers was emotional support from health employees, but neglected. Participants in this research pointed out their patient’s stroke as a sudden experience with stress and anxiety. They pointed to the need for hope, sympathy and support, and indicated that the need for care was ignored by the treatment staff. They also said they experienced disregard instead of a supportive relationship.
“I was dying in the emergency room from the fright of the word stroke; the nurse told me what I had to go after. When I regained consciousness, I said what? Could you say again? She looked at me so that I said sorry.” (A 35-year-old woman caring for a patient with stroke for three months).
“Nurses came to my mother's bed, like checking a car without saying what they wanted to do and then went ... When I spoke, I asked for something, or I was sad for all of it, they were indifferent as if I was not talking to them.” (A 27-year-old woman caring for a patient with stroke for a year).
“... the doctor seemed to be speaking with me as if I had made a stroke for my father ... the compassion did not make the meaning.” (A 35-year-old man caring for a patient with stroke for a year).
“Sometimes when I am at home with my mom and we lose our interest, I think if God did not give me patience, how I came out with the situation that nobody is going to get to anyone.” (A 27-year-old woman caring for a patient with stroke for a year).
4.3.2. Educational Needs
Part of the caregivers’ experiences was on neglecting their educational needs for care. Issues that caregivers had experienced in this area included confusion in decision making for regimen therapy (nutrition, drug treatment, rehabilitation), lack of awareness of the appropriate authority for resolving problems, and lack of information and education.
The confusion in decision making was one of the issues experienced by caregivers. The use of simple and understandable tools and methods for training to facilitate the understanding of family and patient regarding the dietary regimen plays a significant role in improving compliance with diet therapy. Participants have stated that at the moment of discharge from the hospital, the medical care staff has given up the patient and his family by saying a couple of general words.
“… It’s better to get which kind of walker; I say to a doctor, he says a foreign word and speaks so fast I do not understand ...” (A 50-year-old man caring for a patient with stroke for a year).
“... my father’s mouth gets bruised, I do not know what his body lacks. Sometimes, his body does shake once, I do not know it is better to give him sugar; it does not get worse for him! ... when I say to his doctor, only mouthwashes he prescribes, without use” (A 30-year-old man caring for a patient with stroke for seven months).
“We’re going to the doctor for my mummy by three; sometimes by two or three we go to the office; you know why? Because the doctor is talking fast and with big words.” (A 35-year-old woman caring for a patient with stroke for three months).
4.4. Lack of Awareness About the Appropriate Authority for Resolving the Problem
During the care of the patient, his family needs an understanding of the disease and ways to resolve the problem in an emergency. Caregivers may face difficulties when they are unaware of the lack of access to the appropriate center or reference.
“When mom became so bad, I was very afraid and rung emergency. It became late so that I called for a taxi. Thank God ... We had a narrow escape. Sometimes, if I took a chance, I would get a doctor fast ... Recently a private doctor visits at home, but he takes a lot of money ...” (A 27-year-old woman caring for a patient with stroke for a year).
“If there was a book or a movie that taught some work to us, it would be very good ... When he’s bad, I really do not know what to do ... Because I do not understand its language when I search it on the Internet” (A 42-year-old woman caring for a patient with stroke for a year).
4.5. Lack of Sufficient Information and Education
Considering that family-based care and supporting stroke-affected patients by treatment staff are poor in Iran and that the families of patients with stroke do not receive any training in the field of rehabilitation and care in this regard, which is very simple and applicable, they refer to private places for rehabilitation. Participants in this research experienced the need to be aware of the patient’s condition, how to improve motor status, prevent respiratory infection, control urination and stool, prevent deformity and limb pain, modify thinking, skin health and treatment and care program, education on how to participate in the care and also lack of information and adequate training, which were accompanied by increased tension.
“I’ve seen the suction in the department, which the nurse does, but I did not know exactly when it was ... It’s uncomfortable. But whenever I do it, he is relieved of pain. But before learning it, I was afraid. The nurse was expecting to learn it once and for all, I did not learn there. I went to a relative, he taught me with a simple language; many times he came to see my doing, so I learned it finally.” (A 27-year-old woman caring for a patient with stroke for a year).
“... I think that this nurse is not in good spirits with all these strokes.” (A 35-year-old woman caring for a patient with stroke for three months).
“I ask the nurse about when I get him in the bathroom, what he should eat, when these tubes go outside, when he should go, etc. She says you should ask his doctor; I ask the doctor he says whether someone does not tell you what in the department; then he says a few English words, he does not look you more, he has not any time. I learned finally from my other companions.” (A 30-year-old man caring for a patient with stroke for seven months).
“... I want to be a very humorous person and tell me in my language what I should do for him.” (A 50-year-old man caring for a patient with stroke for a year).
Considering that family-based care and support for families of patients with stroke are poor by the treatment staff, the care is taken to improve motor status, prevent deformity and limb pain, modify the thinking process, achieve a suitable method for communication, remove sense, perceptual and cognitive deprivations, and skin health, prevent respiratory infection, and control urination and feces.
5. Discussion
Family exposure to the phenomenon of caring for patients with stroke, similar to taking care of other chronic disabling diseases, appears to create much tension for the caregiver and family of the patients. The main caregivers are especially exposed to stress because the patients’ biological, social, and psychological needs exceed their own needs. According to a study conducted by Dalvandi et al. in Iran about the experiences of patients and their families after a stroke, many families stated that due to the lack of social and financial support, lack of educational programs, lack of access to rehabilitation services, and the physical and mental problems of their patients, they had many problems in caring the patient.
According to researchers, the caregivers of patients with stroke do not receive the necessary training in the field of rehabilitation and the related issues, and thus they refer to private centers for rehabilitation. However, the number of these institutions is low and the cost of rehabilitation is very high. Therefore, most caregivers take care of their patients at home according to their own knowledge and the knowledge of people surrounding them, which is not in accordance with the principles of proper rehabilitation and may lead to many complications in the patients.
Nayeri et al. (26) conducted a study in Iran on families of patients with stroke; which showed the families had a low level of knowledge about care in different areas and there was the neglected rehabilitation, diet, and drug regimens. This will lead to complications or prolonged complications. In research by Khatibian et al. (27), entitled “The effect of education on self-esteem of caregivers of patients with stroke”, the results showed that people who received nutrition education along with the family after hospitalization had a significant difference from the control group in knowledge and awareness of low-fat diet.
Genes sees family-based educational programs in the field of patient drug regimen as a factor effective in improving the interaction between the patient and his/her family and ultimately, observing it (27). He noted that the use of simple and understandable means and methods for training, which would facilitate the understanding of the patient and family in the context of the drug regimen, as well as the presentation of practical and essential points, played a significant role in improving adherence to the drug regimen. It is expected that treatment staff improves the quality and continuity of care in partnership with family-based care.
In this regard, Navidian et al. believe that interventions such as education, family therapy, and group therapy should be used to reduce the burden on caregivers and improve both the quality of patient care and the physical and mental health of the caregiver as a hidden patient. The importance of caring empowerment is prioritized. Since care is a specialty and nurses are in a unique position to interact with people and family members, they can provide the knowledge, skills, and support required for maintaining the quality of care at home. In the care of a patient, his/her family needs a correct understanding of the disease, and the nurse’s duty, along with patient care, is to help the family to increase safety and trust; this approach will improve the health and wellbeing of the family.
5.1. Conclusions
Given the chronic nature of stroke that puts the family in trouble and causes serious complications, the ability of a family element can affect the overall ability of the family to access health goals; the ability of families leads to their beneficial and useful efficacy in providing care, as well. Health care providers can provide adequate training for improving the motor status, preventing deformity and limb pain, modifying the thinking process, finding ways to communicate in an appropriate manner, removing sense, perceptual and cognitive deprivation, skin health, ways to prevent respiratory infection, and ways to control urination and defecation. They will be able to deal with the problems of families of patients after a stroke. The researchers suggest that the experiences of caregivers of stroke patients be improved using several training sessions, training manuals, and sensitivity following the ongoing pursuit of telephone care programs. It is best to evaluate the care programs after the end of each training session with the question and answer method and observing the care provided by the patients’ caregivers. It is suggested that family empowerment be implemented separately for each patient and his primary caregiver following the need assessment phase.