1. Background
Epilepsy is one of the most common neurological diseases worldwide that affects about 50 million people of all ages, about 80% of whom live in low and middle-income countries (1). The time and location of epileptic seizures is are not known to be different from other chronic diseases, it makes it difficult to control itself and causes limitations in daily activities (2, 3). On the other hand, according to the International Diabetes Federation, 8.8% of the world’s adult population has diabetes. Only 10% - 15% of all individuals with diabetes have Type 1 Diabetes Mellitus (T1DM) (4). The constant anxiety and fear of acute and long-term complications, as well as the relentless physical and psychological demands of daily treatment, have significant impacts on physical, social, and emotional well-being (5).
Chronic diseases are physical or mental conditions that require frequent medical care and hospitalization. They do not heal spontaneously, but their treatment can take a long time. They even may not be treated and thus may prevent involvement in regular activities such as school attendance (6). Studies of children and adolescents living with different chronic diseases show the importance of social support to face the disease (7). Social support is seen as the perception of protection and assistance from other people and the sense of being part of a supportive social network. Different support providers have been identified. Social support, which is provided by the family, friends, and community, in addition to the support provided by professionals, hospitals, or other institutions, can effectively support the well-being of children. The benefits of social support depend on the relational, personal, situational, and emotional characteristics of the interaction between the supporter and supported person (8).
Diabetes mellitus and epilepsy are common chronic diseases in children. Perceived social support affects the course of the disease in children with DM or epilepsy. This study was conducted to determine the effect of social support in children with T1DM or epilepsy.
2. Objectives
This study was conducted to determine the level of social support in children with T1DM or epilepsy.
3. Methods
In this descriptive study, the study population consisted of children aged 11 - 17, with epilepsy or T1DM, who applied to the Pediatric Endocrinology and Pediatric Neurology Outpatient Clinics of the Department of Pediatrics in Uludag University Health Application and Research Center between April and October 2017. The sample included 50 children with epilepsy and 50 children with T1DM (total of 100 children) who applied to the outpatient clinics for routine medical examinations and accepted to participate in the study. Assent was obtained from the children, and consent was obtained from their parents who agreed to participate in the study. The inclusion criteria included the age of 11 - 17 years, no other chronic illnesses, and studying in the fourth grade or upper in primary schools.
3.1. Instruments
The Child Introductory Form and the Child-Adolescent Social Support Scale were used to collect the data.
Child introductory form: A total of 15 questions were prepared by the researcher on the sociodemographic characteristics of children.
Child-Adolescent Social Support Scale: It was developed by Malecki and Demaray in 2002 (9) to measure perceived social support in children and adolescents. The Turkish validity and reliability study of the scale was performed by Yardimci and Basbakkal (10). It proved to be used to measure children’s and adolescents’ social support for their health behaviors. The scale consisted of 60 items in five sub-groups such as family, teachers, classmates, close friends, and people in the school. The scale is scored in two sections including frequency and significance. The frequency is scored as 1 (never), 2 (rarely), 3 (sometimes), 4 (mostly), 5 (almost always), and 6 (always). The significance is scored as 1 (not important), 2 (important), and 3 (very important). Each subscale consists of 12 items. The lowest score obtained from the frequency section of each subscale is 12, while the highest score is 72. The lowest score obtained from the frequency section of each subscale (12 items) is 12, while the highest score is 36. The lowest score obtained from the frequency section of the scale is 60, while the highest score is 360. The lowest score from the significance section of the scale is 60, while the highest score is 180. As the total score obtained from the frequency and significance sections of the social support scale increases, the level of considering social support as significant increases.
The SPSS 20.0 statistical program was used to evaluate the research data. In the evaluation of the data following the objective of the study, the descriptive information about children with epilepsy and type 1 diabetes was given as numbers and percentage distributions. The Mann Whitney U test and t-test were used to evaluate the data.
Before the study, the ethics committee approval was obtained from the Clinical Research Ethics Committee of Uludag University Medical Faculty. Verbal consent was obtained from children and their families.
4. Results
The study included 100 children, 50 of whom were diagnosed with epilepsy and 50 with type 1 diabetes. Besides, 50% of the children were females. The mean age of the children was 14.10 ± 2.03, and the mean duration of the disease was 6.22 ± 4.15 (Table 1).
| Socio-Demographic Characteristics | No. (%) or Mean ± SD |
|---|---|
| Gender | |
| Female | 50 (50) |
| Male | 50 (50) |
| Family income status | |
| Moderate | 69 (69) |
| Good | 31 (31) |
| Mean age | 14.10 ± 2.03 |
| Diagnosis time | 6.22 ± 4.15 |
| Number of siblings | 1.75 ± 1.11 |
| Maternal age | 41.19 ± 4.62 |
| Paternal mean age | 44.82 ± 5.50 |
Concerning the scores of the children on the frequency subscales of the CASSS, scores of the children with epilepsy in all social environment subscales including mother, teachers, classmates, and close friends except for father, were found to be lower than those of the children with type 1 diabetes; showing a statistically significant difference.
There was no significant difference between the groups of type 1 diabetes and epilepsy in the significance subscales of the CASSS (Table 2).
| Type 1 Diabetes Frequency Subscale | Epilepsy Frequency Subscale | Type 1 Diabetes Significance Subscale | Epilepsy Significance Subscale | |
|---|---|---|---|---|
| My mother | 53.14 ± 7.80 | 49.16 ± 9.72 | 28.26 ± 3.59 | 28.44 ± 4.68 |
| Mwu | 946.500 | 1242.000 | ||
| P | < 0.036a | > 0.95 | ||
| My father | 49.66 ± 11.51 | 46.30 ± 11.29 | 27.76 ± 4.90 | 28.70 ± 4.7 |
| Mwu | 1012.500 | 1114.000 | ||
| P | > 0.101 | > 0.347 | ||
| My teachers | 54.46 ± 9.58 | 49.14 ± 10.14 | 28.00 ± 4.46 | 29.38 ± 4.43 |
| Mwu | 874.000 | 1016.000 | ||
| P | < 0.009b | > 0.105 | ||
| Classmates | 49.54 ± 8.17 | 42.92 ± 10.62 | 26.02 ± 5.32 | 26.64 ± 5.39 |
| Mwu | 773.500 | 1199.000 | ||
| P | < 0.001c | > 0.724 | ||
| Close friends | 66.28 ± 8.20 | 54.20 ± 8.44 | 29.72 ± 4.58 | 29.44 ± 4.36 |
| Mwu | 766.500 | 1209.50 | ||
| P | < 0.001c | > 0.779 | ||
| Total | 265.70 ± 37. | 241.64 ± 39.71 | 139.86 ± 17.89 | 142.42 ± 19.33 |
| Mwu | 808.500 | 1155.50 | ||
| P | < 0.002b | > 0.514 | ||
aP < 0.05
bP < 0.01
cP < 0.001
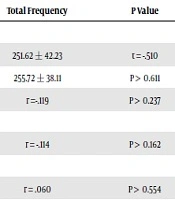
When the total frequency and significance scores were examined according to gender and income level, no statistically significant difference was found between male and female children.
There was a significant negative correlation between child age and social support. There was not significant correlation between the number of siblings, maternal age, and the frequency and significance scores on the CASSS (Table 3).
| Description | Total Frequency | P Value | Total Significance | P Value |
|---|---|---|---|---|
| Gender | ||||
| Female | 251.62 ± 42.23 | t = -0.510 | 142.08 ± 17.00 | t = 0.504 |
| Male | 255.72 ± 38.11 | P > 0.611 | 140.20 ± 20.16 | P > 0.615 |
| Age of the child | r =-0.119 | P > 0.237 | r = -0.198 | P < 0.049a |
| min – max | 11 - 17 | |||
| Number of siblings | r = -0.114 | P > 0.162 | r = 0.087 | P > 0.389 |
| min – max | 0 - 5 | |||
| Maternal age | r = 0.060 | P > 0.554 | r = -0.062 | P > 0.542 |
| min – max | 34 - 53 | |||
| Income level | ||||
| Moderate | 250.23± 42.04 | t = -1.284 | 261.32 ± 34.73 | t = -0.286 |
| Good | 140.78 ± 18.71 | P > 0.202 | 141.93 ± 18.54 | P > 0.776 |
aP < 0.05
5. Discussion
This study aimed to determine social support in children with type 1 diabetes or epilepsy. Concerning the frequency and significance scores of social support in Table 2, the highest scores in both diabetes and epilepsy groups were obtained from close friends and mothers.
Young people see their families as the most important social support providers in their lives (11). Emotional, physical, and social demands accompanied by having a chronically ill child create additional stress in addition to the role of parenting. These children need additional support in their daily lives in terms of basic needs and participation in domestic and social life. During a severe disease, especially during the time of relapse (11), adolescents identify good social relationships with their parents as the most important social support (12). More specifically, Haluska et al. (13) found that young cancer patients were generally satisfied with perceived social support and valued their parents’ support more than did their healthy peers. Mothers are mostly considered to be great support providers because they are the most interested in primary care for school-aged children and are more emotionally related to the child (12).
It is also important to establish close, supportive relationships with peers (12). Cullum et al. (14) found that close friends and mothers are seen as the most important sources of social support for adolescents with type 2 diabetes. The need for friend support is emphasized during the acute treatment phase. However, it has been reported to decrease over time (12).
Children tend to reduce the negative effects of the disease when they perceive higher social support (15). Specifically, it was found that social support from classmates had a positive effect on ensuring better self-confidence and reducing anxiety about the disease and depressive symptoms when attending to social school settings (16). In addition, perceived social support from parents, peers, and teachers were found to be negatively correlated with psychological distress and positively correlated with self-esteem (17). Therefore, perceived support is very important for positive well-being and development in childhood.
The frequency score of social support was lower in children with epilepsy than in children with diabetes. This result may be due to the decrease in the need for social support due to the alleviation of epilepsy seizures with the selection of appropriate drugs.
In Table 3, gender, the number of siblings, maternal age, and income level did not affect the frequency and severity scores on the CASSS. Similarly, Young et al. (18) found that the difference between the scores of primary school students and high school students on the perceived social support scale was not significant according to their gender. In a study, Erdeger (19) determined that the students’ social support levels did not change according to their family income levels. The results of these studies support the current study. Tam et al. (20) conducted a study with adolescents and Bokhorst et al. (21) conducted a study with individuals at the ages of 9 - 18 years. They found that the perceived social support scores of girls were higher than those of boys.
In a study, a significant correlation was found between the social support importance scores and the age of the adolescents (Table 3). As the age of the adolescents increased, their social support significance score decreased. Cheng and Chan (22) and Jackson et al. (23) found that the relationship between age and perceived social support was significant; as the age increased, the level of perceived social support decreased. The decrease in family support as the age increased possibly because the group of adolescents cares about their friends more than their families as a source of social support. Adolescents should be evaluated according to their developmental stages (early, middle, and late adolescence). In early adolescence, the beginning of breaking the ties between parents and adolescents, they search for belonging in their peers. However, adolescents in this age group do not write off their mothers and other adults from their lives. Peer interactions are more important than relationships with parents for adolescents (24). Adolescents with diabetes have to maintain close relationships with their parents to successfully manage the disease. If these ties break early, this condition may lead to inadequate disease management (25).
5.1. Study Limitations
The study was limited to children with epilepsy and type 1 diabetes who were at the ages of 11 - 17 years and applied to the Pediatric Endocrinology and Pediatric Neurology Outpatient Clinics of the Department of Pediatrics in a hospital. Therefore, the results obtained from the study can only be generalized to children with epilepsy and type 1 diabetes in this study group.
5.2. Conclusion
Children with epilepsy had lower social support scores than children with type 1 diabetes when the children’s scores on the frequency subscale of the CASSS were examined. As the ages of the children decreased, the significance of social support increased. According to these results, nurses should especially talk with chronically ill children about the sources of social support and should give information to them to facilitate their access to these resources.