1. Background
Today, it is believed that major health problems are related to chronic diseases (1). Chronic diseases affect the routine and daily activities of life (2). On the one hand, physiological factors, as well as psychological causes, play a role in the incidence of chronic diseases (3). Furthermore, determining the psychological problems of patients with chronic diseases and trying to solve them are of great importance since they impose high costs on the individual and society (4, 5). Psychological problems of such patients include emotional processing and regulation, as well as the quality of life.
Through emotional processing, emotional or psychological disturbances are absorbed and reduced to the degree that individuals can continue their other experiences and behaviors without any difficulties (6). Four categories of factors may also cause problems in emotional processing: cognitive avoidance (the process in which the mind refuses to accept the events), lack of experience in short-term habit formations, depression, and overvalued ideas (7). The results of previous studies show that people who use weaker cognitive styles, such as rumination, catastrophic thinking, and self-blame, are more vulnerable to emotional problems. However, individuals who use preferred styles, such as positive re-evaluations are less vulnerable (8).
Mund and Mitte (9) indicated that people who suppressed their excitement had a higher risk of developing certain diseases. The disturbing emotions create a bias of attention and cause a disturbance in emotional processing. Research findings show that those who choose ineffective styles during emotional processing are more vulnerable to emotional problems (10-12). Patients with chronic stress and negative excitement, such as fear and anger are very sensitive and have a problem in controlling their stress and regulating their emotions (13). In some psychological trauma, one or more components of emotional processing are disturbed. These disturbances occur in the incidence of emotions. Consequently, the ability of patients to perform one or more adaptive emotional functions is impaired (7).
Emotional processing, one of the most important effective variables in quality of life and mental health, is defined as positive or negative strategies applied by individuals to deal with adverse and stressful life events (14). Based on pieces of evidence, negative strategies inversely correlate with depression, but positive strategies have a significant negative correlation with mental health indicators and quality of life. In other words, individuals’ mental health and quality of life depend on the interaction between the application of certain types of emotional processing strategies and appropriate assessment of stressful situations (15).
The quality of life has been investigated as an important issue in health care research, especially in chronic disease studies. The literature shows that the diagnosis of chronic diseases directly affects the patients’ quality of life and changes their daily lives in different ways (16). Chronic diseases have a negative impact on the patients’ quality of life as a multifactorial issue (17). One of the influential factors on individuals’ quality of life is emotional processing that is a basic concept in psychology (18).
The quality of life, which is defined as the characteristics that people require to maintain their abilities to conduct valuable life activities and chronic diseases, has negative effects on the health and quality of life (19). Today, the quality of life is considered an important issue and consequence of health in treating and taking care of chronic patients (20). The health-related assessment of the quality of life is important for physicians and health policymakers (21). Studies showed that patients with thalassemia had lower quality of life than the control group (22, 23). In this regard, patients with diabetes mellitus had significantly lower levels of mental health and quality of life than the control group (2, 24, 25). Camacho et al. (26) studied the quality of life among patients with diabetes mellitus and concluded that increased severity of diabetes had a significant negative effect on the patients’ quality of life, especially in terms of psychosocial aspects. Similar studies also mentioned that other chronic diseases, such as diabetes mellitus, affect various dimensions of people’s lives and reduce their quality of life (27). As a result, chronic diseases that require hard work for treatment reduce the individuals’ quality of life (1). Over the past two decades, the results of studies showed that the main goal of treatment was not only to eliminate the disease symptoms and signs but also to improve the overall patients’ quality of life. In order to achieve this goal, the psychological and psychosocial consequences of diseases should be taken into consideration (28).
2. Objectives
Considering the results of other similar studies, and the importance of psychological problems in chronic patients, psychological problems, along with physical injuries of these patients should be noted. As a result, the lack of research in this field led the researchers of this study to compare emotional processing and quality of life among patients with thalassemia major and type 2 diabetes mellitus and healthy people. The aim of this study was to provide useful information about these diseases and the current needs in this field to take effective measures in improving patients’ mental and physical health.
3. Methods
This causal-comparative study was conducted on all patients with thalassemia and type 2 diabetes mellitus and healthy people who referred to health care centers of Saravan City for examination and treatment in 2017 - 2018. Considering the limited number of the statistical population in this research, the available sampling method was used, and all people who referred to the health centers (n = 153) were selected by the Morgan sampling table. The participants included 53 patients with thalassemia major, 50 patients with type 2 diabetes mellitus, and 50 healthy individuals, who were matched in terms of age and gender. The study was carried out within a six-month period. The inclusion criteria were passing at least one year from the onset of chronic disease, diagnosing the disease by the physician, having the age of 16 and over, having the reading and writing skills, having no psychiatric and cognitive problems, having consent to participate in the study, and having no chronic diseases for the healthy people. The participants were explained about the study objectives, were asked to carefully read the questions and select the responses according to their characteristics, and were also required to answer all the questions. The questionnaires were completed individually. Patients with acute conditions and those who could not complete the questionnaire were not included in the research. The exclusion criteria were reception of psychiatric treatment, reluctance to participate in the study, and incomplete questionnaires.
Data collection tools consisted of two questionnaires:
1) Emotional Processing Questionnaire: This scale, developed by Baker et al. (8) in 2010, has 25 items and aims at evaluating the components of emotional processing (suppression, uncontrollable emotions, emotional experiences, signs of unprocessed emotions, and avoidance). The questionnaire items should be scored based on a five-point Likert scale (totally disagree = 1, disagree = 2, no idea = 3, agree = 4, totally agree = 5). The minimum and maximum attainable scores are 25 and 125, respectively. Scores of 25 - 50 represent poor emotional processing, 50 - 75 show moderate emotional processing, and 75 - 125 indicate very high emotional processing. With regard to this questionnaire, Cronbach’s alpha coefficient was 0.92, and its test re-test reliability coefficient was calculated as 0.79 (8). Cronbach’s alpha coefficient of this scale was reported as 0.95 in the previous research (Lotfi et al., 2012) (29). Cronbach’s alpha coefficient was calculated as 0.73 in the present study.
2) Quality of Life Questionnaire: It was designed by Michael Friesch in 1992 to measure each individual’s quality of life. The questionnaire is a self-report scale, assesses the importance that individuals give to every 16 domains of life quality, and shows their recent satisfaction in each area. This tool is completed very quickly and is useful for evaluating the outcomes of the treatment and mental therapy plans. The four sub-scales of self (health, self-esteem, goals and values, and living standards), personal gain (job, entertainment, learning, creativity, service), relationships (love, friendships, relationships of children, relationship with relatives), and environmental factors (home, neighborhood, community) are scored on a three-point Likert scale (0 = not at all important, 1 = important, 2 = very important). Regarding each area, the importance score is multiplied by the satisfaction score, and the satisfaction value is achieved. These scores are then summed and determine the individuals’ quality of life. Higher scores represent a higher quality of life. This questionnaire is standardized in the adult community and among the clinical and non-clinical groups. Based on three clinical and non-clinical samples, the validity of this scale was in the range of 0.87 - 0.91 and its internal reliability varied from 0.77 to 0.89 (30). In our study, the reliability of this questionnaire was calculated as 0.71 using Cronbach’s alpha.
3.1. Ethical Considerations
The participants were explained about the study purpose and received the required instructions about completing the questionnaires. Later, they were asked to sign the informed consent forms. In answering the questionnaires, the researcher provided the participants with the required clarifications in the case that they had any questions in understanding the items. It should be noted that these explanations were provided to avoid any kind of ambiguity or prejudice. In order to ensure the confidentiality of the data, a code was dedicated to each participant, and the information was interpreted based on these codes. The code of Ethics for the present study was 254047. This code is the code approved by the dissertation because it did not have the Ethics Committee at the time of the university’s dissertation approval.
3.2. Statistical Analysis
Data were analyzed by SPSS version 23 using descriptive statistics (mean, standard deviation) and inferential statistics, including MANOVA and Tukey post hoc test.
4. Results
Based on the demographic data of 153 participants (53 patients with thalassemia major, 50 patients with type 2 diabetes mellitus, and 50 healthy participants), the participants’ age ranged from 16 to 59 years. In the thalassemic group, 50.9% of the participants were women, while in the groups with type II diabetes and healthy groups, 54% and 58% of the individuals were male, respectively.
In Table 1, the mean and standard deviation of study variables are presented for all study groups, i.e., thalassemia, type 2 diabetes mellitus, and healthy.
| Variable | Thalassemia (N = 53) | Type 2 Diabetes (N = 50) | Healthy (N = 50) |
|---|---|---|---|
| Emotional processing | |||
| Suppression | 16.15 ± 3.98 | 14.52 ± 2.73 | 12.96 ± 4.34 |
| Uncontrollable emotions | 13.30 ± 3.98 | 13.96 ± 2.11 | 13.28 ± 2.79 |
| Emotional experiences | 13/44 ± 3.57 | 13.68 ± 2.49 | 12.06 ± 4.60 |
| Signs of unprocessed emotions | 15.00 ± 4.03 | 15.50 ± 2.40 | 13.36 ± 3.79 |
| Avoidance | 17.49 ± 4.07 | 16.82 ± 2.35 | 16.78 ± 3.63 |
| Total emotional processing score | 75.41 ± 11.29 | 74.48 ± 7.32 | 68.44 ± 14.49 |
| Quality of life | |||
| Self | 36.20 ± 17.16 | 33.74 ± 13.40 | 37.56 ± 12.16 |
| Personal gain | 94.37 ± 41.28 | 85.86 ± 33.39 | 121.40 ± 39.94 |
| Relationships | 40.72 ± 17.51 | 46.40 ± 19.43 | 73.69 ± 25.29 |
| Environmental factors | 34.35 ± 13.51 | 28.94 ± 15.85 | 40.28 ± 10.84 |
| Total quality of life score | 189.26 ± 58.74 | 238.64 ± 64.05 | 245.64 ± 56.75 |
aValues are expressed as mean ± SD.
The results of Table 1 indicate that the mean of emotional processing and its subscales (suppression, uncontrollable emotions, emotional experiences, signs of unprocessed emotions, and avoidance) decreased in the healthy group compared to the groups with diabetes and thalassemia. However, the mean quality of life and its subscales (self, personal gains, relationships, and environmental factors) increased in the healthy group compared to the other two groups. In order to compare the effect of one independent variable on more than one dependent variable, multivariate analysis of variance (MANOVA) should be used. So, was used MANOVA to investigate differences among the three groups with regard to emotional processing and quality of life.
The type of group had a significant effect on the linear composition of emotional processing (Eta = 0.97, P = 0.002, F = 2.93) and quality of life (Eta = 0.26, P = 0.001, F = 13.41). In order to study the effect of group on emotional processing and quality of life, multivariate analysis of variance was carried out.
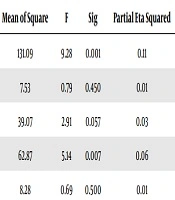
Table 2 shows the difference among groups with regard to emotional processing. The observed F value shows that only subscales of suppression and signs of unprocessed emotions, among emotional processing components were significantly different among the three groups. Tukey’s post hoc test was used to determine the difference between the groups. According to the results of the Tukey test, the mean score of suppression was significantly lower in the healthy individuals (12.96) than that of the thalassemia group (16.15) (P = 0.001). Furthermore, a significant difference was observed among the mean scores of the signs of unprocessed emotions for the healthy participants (13.36), patients with diabetes (15.00), and patients with thalassemia (15.00). The mean score of the healthy group was lower than the groups of patients with diabetes and thalassemia.
Table 3 represents the results of the multivariate analysis of variance among the groups. The observed rate of F-value for the subscales of the quality of life shows a significant difference among the three groups with regard to the subscales of personal gains, relationships, and environmental factors. Tukey’s post hoc test was run to determine the difference among groups. The results showed that the differences among the mean scores of healthy individuals (12.12) as well as patients with diabetes mellitus (85.86) and thalassemia (94.37) were significant with regard to the personal gain. Moreover, a significant difference was observed between the two groups with thalassemia and diabetes. Considering the subscale of relationships, the mean score of healthy people (73.69) was significantly different from those of patients with thalassemia (40.72) and diabetes (46.41). The mean score of environmental factors was higher in the healthy group (40.28) than the diabetic group (28.94).
5. Discussion
The purpose of this study was to evaluate emotional processing and quality of life among patients with major thalassemia, type 2 diabetes mellitus, and healthy individuals. The findings showed a significant difference between the three groups in terms of emotional processing and quality of life (Tables 2 and 3). The results of this study were confirmed partially by some previous studies (10-12, 25, 31-43).
| Source | Dependent Variable | Sum of Squares | df | Mean of Square | F | Sig | Partial Eta Squared |
|---|---|---|---|---|---|---|---|
| Groups | Suppression | 262.19 | 2 | 131.09 | 9.28 | 0.001 | 0.11 |
| Uncontrollable emotions | 15.06 | 2 | 7.53 | 0.79 | 0.450 | 0.01 | |
| Emotional experiences | 78.15 | 2 | 39.07 | 2.91 | 0.057 | 0.03 | |
| Signs of the unprocessed emotions | 125.74 | 2 | 62.87 | 5.14 | 0.007 | 0.06 | |
| Avoidance | 16.55 | 2 | 8.28 | 0.69 | 0.500 | 0.01 |
| Source | Dependent Variable | Sum of Squares | df | Mean of Square | F | Sig | Partial Eta Squared |
|---|---|---|---|---|---|---|---|
| Groups | Self | 375.57 | 2 | 187.78 | 0.89 | 0.41 | 0.01 |
| Personal gain | 34542.91 | 2 | 17271.45 | 36.23 | 0.001 | 0.32 | |
| Relationships | 32270.75 | 2 | 16135.37 | 11.96 | 0.001 | 0.13 | |
| Environmental factors | 3217.08 | 2 | 1608.54 | 8.74 | 0.001 | 0.10 |
The results of studies showed that patients with diabetes had poorer emotional regulation than the control group (31, 32). People who chose inappropriate styles during emotional processing were more vulnerable to emotional problems (10-12). People who suppress their emotions have a higher risk of developing certain diseases. As a result, the disease has the potential to bring about plenty of emotional complications. So, effective psychological interventions should be conducted to reduce distress and help cognition challenges. People who suppress emotions do not experience strong negative emotions. They exercise great control over their emotions and behaviors and avoid threatening information defensively (33). The stress responses of suppressive people are as large as or greater than those who welcome their distress (34, 35). These individuals are prone to physical illnesses in the long-term and experience more health problems (33). If emotions are regulated by suppression, they will cause harmful effects on health (36). People with chronic diseases recognize negative images more than those with positive images. Therefore, people with chronic diseases should be educated to increase their tolerance by neglecting negative stimuli and improve their emotional regulation significantly (33).
Compared with healthy individuals, patients with chronic diseases experience higher levels of emotional and mood problems, which can affect the disease course and prognosis. Emotional processing training is of great importance for patients with chronic diseases because it works specifically to regulate their excitement and mood (38). Emotional processing along with techniques and skills, such as mindfulness, endurance tolerance, and interpersonal communication, provide people with new solutions and help them to adjust the effects of distressing conditions caused by diseases such as diabetes mellitus, major thalassemia, and related excitements better (37).
To explain this finding, it can be mentioned that the relationship between emotions and health has a fundamental place in the field of psychology of health. In this regard, experiencing emotions and expressing them can play a vital role in a person’s health. Efforts to suppress negative emotions are one of the main components in the formation and development of a variety of physical illnesses. Suppressed negative emotions can lead to serious diseases. For this reason, emotion regulation and expression have an important role in adapting to chronic diseases and understanding emotions, which can help the patients’ mental health. Therefore, patients with chronic diseases can adapt to the problems and opportunities that they face in life using emotion processing. They can also inhibit or reduce the negative emotions by employing psychological skills to counteract negative emotions effectively. Psychological skills training can lead to better adaptation, higher life satisfaction, and better life quality.
The literature showed that patients’ quality of life with chronic diseases was lower than that of healthy people. In fact, physical impairments and symptoms had a direct effect on all aspects of the quality of life (39). Complications of chronic diseases, reduced life expectancy, and increased mortality rates impose a large burden on the individual, family, and society. They also affect the individuals’ and families’ quality of life (40). Lack of attention to individuals’ quality of life can lead to disappointment, lack of motivation, as well as reduction of economic, social, and health activities. In a deeper dimension, it can affect the socio-economic development of a country (41). Patients with thalassemia had low scores in all aspects of quality of life. Impaired quality of life in these patients had a negative impact on their social, family, work, and leisure activities and increased the risk of hospitalization and mortality caused by this disease (42).
Thus, it can be said that the chronic and tiring nature of chronic diseases affects the patients’ quality of life (25). In order to control such diseases appropriately, the patients’ quality of life should be improved, which also reduces health care costs (43).
The findings showed that patients with diabetes mellitus and major thalassemia had a lower quality of life than healthy people. So, determining psychological damages of such diseases provides healthcare professionals with more related information and helps them benefit from a more comprehensive approach in the treatment process. Consequently, the treatment process of these patients should not be limited to physiological approaches. In other words, considering the role of psychological variables in the treatments will improve their efficiency and facilitate further comprehensive steps in the treatment of mental disorders.
Consequently, people with chronic illnesses consider that these diseases are associated with the feeling of hopelessness and bad health status compared with other people, which leads to a decrease in their general health and quality of life. Low quality of life scores for these patients and the need for better adjustment of these patients to their illnesses require psychological counseling and psychosocial support services.
5.1. Conclusions
Chronic diseases such as major thalassemia and type 2 diabetes mellitus are considered the most important problems in today’s societies and decrease the patients’ quality of life and mental health of the community depending on their severity and frequency. Considering the findings of this research and other similar studies, a significant difference was observed among patients with major thalassemia, type 2 diabetes mellitus, and healthy individuals with regard to emotional processing and quality of life. Emotional processing had the highest mean score in the thalassemia group; whereas, the mean of thalassemia group in the quality of life was lower than the other groups. Therefore, consideration of the physiological approach is not enough in patients’ treatment process. In the case of considering the role of psychological variables in the etiology and treatment area, the therapeutic process and effects will be more efficient and long-term. Therefore, investigation of the effective psychological factors in the occurrence of these diseases is of great importance. For this reason, emotion regulation interventions provide this opportunity for chronic patients to reassess their life goals and priorities. By simultaneous implementation of the psychological therapies and medical treatments, an increasing number of chronic patients can improve and return to the community. With the cooperation of physicians and psychologists, more comprehensive measures should be taken to treat psychosomatic disorders. In this regard, comprehensive and preventive programs should be implemented by health centers to improve the individuals’ mental health.
5.2. Limitations
Some limitations of the present research included its cross-sectional design and patients’ lack of concentration due to the crowded environment of the hospital. Furthermore, specific types of thalassemia and diabetes were not studied; so, we recommend that researchers compare the quality of life and emotional processing in specific types of thalassemia and diabetes mellitus. Moreover, patients with other diseases should be investigated so that the comparison of the results can result in more comprehensive and accurate findings. Other researchers can also focus on these diseases’ aspects and psychological effects at all levels of treatment and hold regular training courses on positivism and emotion regulation for the staff working in special disease centers. The results of such pre- and post-intervention findings can enhance the generalizability and richness of the obtained information and provide more accurate explanations about the extent and type of relationship between these variables.