1. Background
According to a publication by Yaxley in 2016 (1), the cancers of urinary system are common and include a series of injuries encompassing small benign tumors to destructive neoplasms with high morbidity. The urinary tract is lined by epithelium extending from the renal tubule proximallly to the external urethral orifice distally. These epithelial cells are recognized as the urothelium or transitional cells. They are highly specialized cells with elasticity and variable shape. Any segment of the urothelium can be affected by malignant transformation. In the year 2008, 12.7 million cases with cancer, and 7.6 million cancer-related deaths were reported by Globocan (2). Siegel et al., in 2013 reported (3) that advanced urothelial carcinoma accounts for about 15,000 deaths in the United States annually. The most common malignancy reported is urinary bladder cancer. The report indicates a higher ratio (2:1) of upper tract urothelial carcinoma in men than in women. The main risk factors are occupational exposure, various chemical carcinogens and cigarette smoking (4). Histological tumor classification is an established predictive factor of renal cell carcinoma (5). Cytologically and histologically, overexpression of p16INK4a has been recognized in urothelial malignancies. Therefore, there are potential implications for the clinical management of patients after the conservative treatment of non-muscle-invasive urothelial carcinoma. Furthermore, a long-term assessment of p16/Ki-67 double labeling has been revealed to distinguish high-grade urothelial cancer cells and particular individual development within a 12-month period (6). In a population with clear-cell renal cell carcinoma collecting system invasion is related to lack of prediction (7). Total existence and progression-free survival in patients with urinary system cancer could be associated with high serum levels of lactate dehydrogenase (8). Study of kidney cancer in rural Illinois showed that the kidney and renal pelvis cancer incidence was higher in urban counties whereas mortality was higher in rural counties (9). In Hong Kong in year 2012, a report indicated that 9.6% of new cancer cases were related to urological malignancy (10). Study of 198 patients with bladder cancer (BC) and 396 healthy individuals in Shiraz, Iran mentioned that a potential risk factor could be the use of opium (11).
As the essential knowledge of public health strategy, the use of epidemiologic information associated with urinary systems, is the need to provide a knowledge causes of disease and its pharmacotherapy management.
2. Objectives
As there is considerable variation in the distribution of diseases worldwide, therefore the aim of this study was to show up-to-date estimates of crude rate, incidence rates and differences in rates between men and women of urinary system cancer in Isfahan, Iran.
3. Methods
This retrospective study was conducted to the Isfahan Kidney Transplantation Research Center (IKTRC) and approved by the Isfahan Deputy of Research Committee via the Ethics Committee code number (295115). Cancer data was obtained from the Isfahan Cancer Registry located in deputy of health. The data considered in this study belonged to the years between March 2011 to March 2015. The cancer sites studied were characterized according to the international classification of diseases (ICD-O; third edition). All cancers were defined by topography code. For example, kidney was defined by topography code C64, renal pelvis by the topography code C65, ureter by topography code C66 and bladder by topography code C67. There was not any exclusion criterion. After removing patient name and surname, demographic data such as age and gender, final code for cancer diagnosis and date of reported cancer were recorded. Variables such as gender, being alive/dead, year of the report were expressed by frequency, percentage, period prevalence and incidence rate. The total population of Isfahan city was obtained from the Isfahan/Program and Budget Management Organization. Period prevalence was calculated as the proportion of total cases over the period of the years 2011 - 2015/to populations at risk during the same time period × 100000. Cancer incidence rate (CIR) was calculated as dividing new cases of cancer during a given time period/to populate at risk during the same time period × 100000. Analysis of data was carried out using the statistical package for social science (SPSS® version 20 IBM Corp., Armonk NY, USA). An age that was a continuous variable was expressed by mean ± standard deviation (SD) (12-20).
4. Results
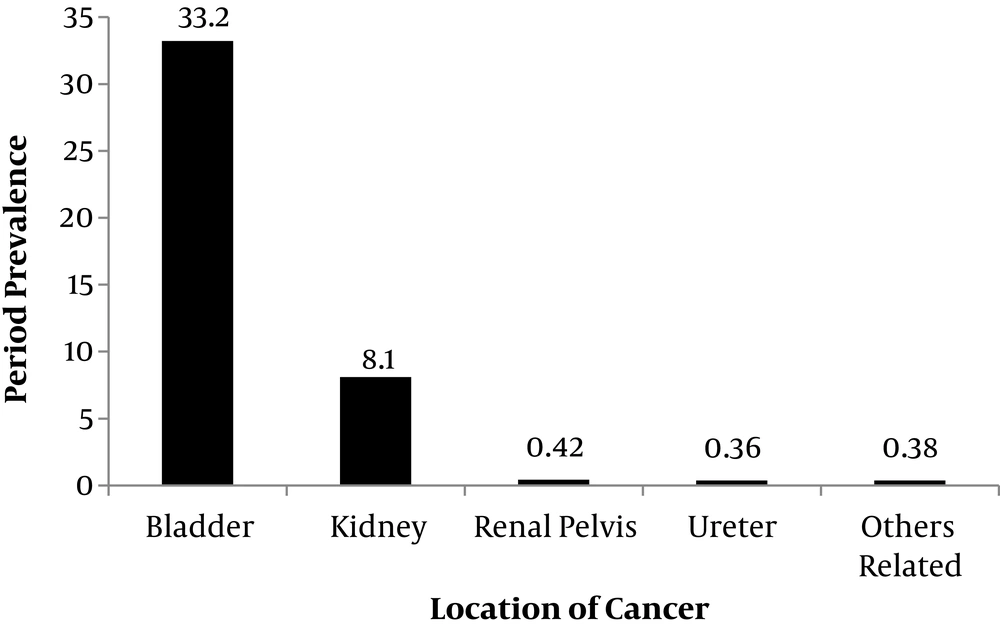
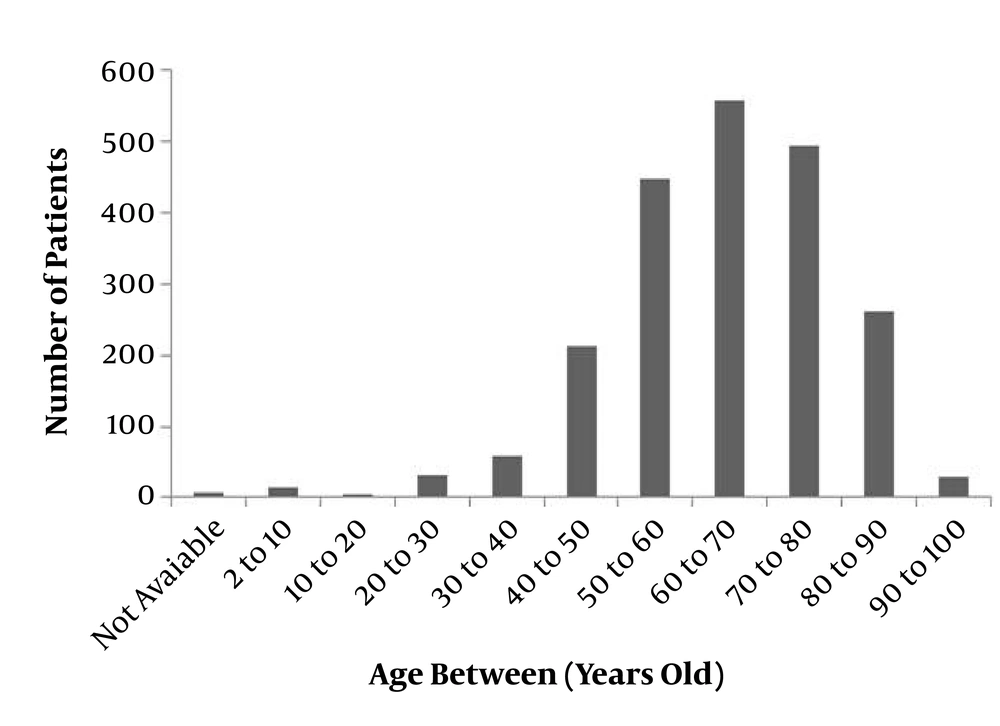
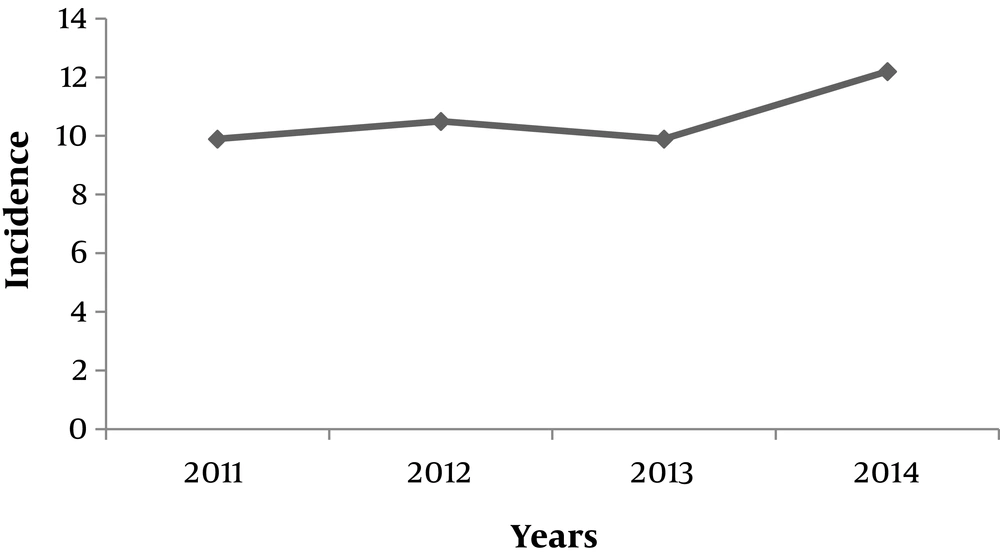
Table 1 shows demographic and epidemiological characteristic in 2117 patients with urinary system cancers. The study population comprised of 440 females and 1677 males. The total period prevalence was calculated as 42.5 per 100000 persons (Figure 1) that corresponded to: 33.2 for bladder, 8.1 for a kidney, 0.42 for renal pelvis, 0.4 for ureter and 0.8 for other and unspecified urinary organs. With the mean age ± standard deviation of 63.6 ± 14.9 years, age related to urinary system cancers in 1%, 62% and 37% were related to age under 20, between 20 to 70 and 70 to 100 years of life respectively (Figure 2). Death reported-data was associated with 11% of total cases. The rate of males to females was 83% for bladder, 77% for kidney, 62% for renal pelvis, 94% for ureter and 74% for other and unspecified urinary organs. Incidences of urinary system cancer were calculated as: 9.9 (2011 to 2012), 10.5 (2012 to 2013), 9.9 (2013 to 2014) and 12.2 (2014 to 2015) per 100000 persons (Figure 3).
| Sites of Cancers | Total Cases | Period Prevalence | Estimated Living Cases | Estimated Deaths | ||||
|---|---|---|---|---|---|---|---|---|
| Both Sexes | Females | Males | Both Sexes | Females | Males | |||
| Urinary system | 2117 | 42.5 | 1881 | 368 | 1513 | 236 | 72 | 164 |
| Bladder | 1655 | 33.2 | 1499 | 239 | 1260 | 156 | 41 | 115 |
| Kidney | 404 | 8.1 | 348 | 72 | 276 | 56 | 21 | 35 |
| Renal pelvis | 21 | 0.42 | 9 | 2 | 7 | 12 | 6 | 6 |
| Ureter | 18 | 0.36 | 18 | 1 | 17 | 0 | 0 | 0 |
| Other and unspecified urinary organs | 19 | 0.38 | 7 | 1 | 6 | 12 | 4 | 8 |
5. Discussion
Urinary system cancers are common and impose an important cost, weight on the health system. Previous publications reported that BC and kidney cancers are the most common tumors of the urinary system, that make up to 5% of all cancers globally (21). As there has been diminutive evidence-based data associated with occurrence of urinary system cancers in the Iranian/Isfahan population, therefore this study conducted an analysis obtained from the population-based cancer registry.
In agreement with previous studies of western countries which specified an increasing trend toward incidence of urinary bladder and kidney cancers (22), in this study incidence of urinary system cancers 23.2% was increased between 2011 and 2015. Previous publications confirmed that, there is a change to older-in-age scattering in Iran as a developing country (23). In agreement with previous publications that mentioned the mean age of diagnosis of 65 years (24), in this study also the mean age of patients was also 63.6 years old.
The result of this study is in agreement with the Australian Institute of Health and Welfare report that confirmed bladder cancer as the most common cancers with a rise in incidence (25). De et al. in 2014 studied (26) incidence of kidney cancer between 1986 and 2007. The age-standardized incidence rate per 100,000 rose from 13.4 to 17.9 in males and 7.7 to 10.3 in females. In this study the period prevalence was ranked for BC with a value of 33.2 and 8.1 for kidney per 100000 persons respectively. The PP, among males and females was significantly different (66.4 vs. 17.9, P < 0.001).
The estimated deaths correlated to 236 out of 2117 (11.1%) patients with urinary system cancers. Reported mortality in cancer of renal pelvis was 57.2% and this is in agreement with a published report from Bailey et al. in 2017, declaring that among patients with clear-cell renal cell carcinoma, collecting system invasion is associated with poor prognosis (6).
The results of this study showed that urinary bladder, kidney cancer followed an increasing trend in incidence, mortality and prevalence in Isfahan, Iran (14-20, 26-32). The implications of this investigation could be mentioned as the following suggestions: (1) the health care system should provide a model-based strategy to improve access to specialized medical, pharmacological and surgical facilities; (2) consideration is needed toward the reality for scheduling health system improvements, particularly referral systems; (3) preventing significant difficulties by equality of management for patient satisfaction; (4) attention toward financial management by study of epidemiology and pharmacotherapy.
5.1. Conclusions
From the year 2011 to 2015, there were 2117 patients with urinary system cancers in Isfahan Province. The mean age ± SD was 63.6 ± 14.9 years. In 62% of total population age ranged between 20 and 70 years. The PP was 42.5 per 100000 persons. Total PP corresponded to 66.4 for males versus 17.9 for females (P < 0.001). The PP was 33.2 for bladder, 8.1 for a kidney, 0.42 for renal pelvis, 0.36 for ureter and 0.38 for other unspecified related organs. There were living cases comprised of 368 females and 1513 males. There was a 23.2% increase in the Irs over the study period.
An appropriate judgment and discussion about the trends and changes are needed to investigate the incidence of urologic cancers over time. For future plans additional research toward drug-management associated with urinary system cancers in Iran recommended.