1. Background
Coronary artery disease (CAD) is one of the major causes of mortality and morbidity in industrial societies, for which there are many risk factors (1). Age, sex, smoking, dyslipidemia, diabetes mellitus and hypertension are associated with the severity of coronary lesions in angiography (2). Increased brachial blood pressure is one of the most important risk factors for cardiovascular events in the future. However, the brachial blood pressure does not accurately reflect central aortic blood pressure, as it may indicate a false increase in isolated peripheral systolic blood pressure despite normal aortic blood pressure (3). However, some studies have demonstrated that more than 30% of men and 10% of women with normal brachial blood pressure had central blood pressure similar to individuals with stage 1 hypertension (4). New evidence suggests the central blood pressure may predict cardiovascular events and end-organ damage associated with hypertension better than the brachial pressure (5-7).
Central blood pressure is a useful index for central hemodynamic stress and may be associated with an increased risk of cardiovascular diseases. Moreover, central blood pressure is suggested as a more reliable marker for cardiovascular events rather than the brachial pressure measurement (3, 8). However, the relationship between central blood pressure parameters and the severity of coronary artery disease has not been well addressed (3, 9). Central aortic pressure indices such as pulse pressure (PP), fractional systolic pressure (FSP) and fractional diastolic pressure (FDP) may be associated with an increased risk of cardiovascular disease. Additionally, according to studies, the severity of coronary artery disease can be predicted by measuring FSP and FDP (10). Furthermore, a higher central PP is associated with extensive CAD in angiography (11).
2. Objectives
This study aimed to assess the relationship between the severity of coronary artery disease and central aortic blood pressure. Moreover, the probability of CAD and 3VD has been determined for the first time by using cut-off points based on sensitivity, specificity, NPV, and PPV in an Iranian population.
3. Methods
3.1. Study Population
This study was a hospital-based cross-sectional study conducted at the Center for Elective Diagnostic Coronary Angiography, Ahvaz, Iran. The study population included a total of 300 subjects within an age range of < 18 years old, who were selected, based on the simple random sampling method and the following selection criteria from December 2017 to December 2018.
3.2. Selection Criteria
Patients with the following conditions were excluded from this study: no sinus rhythm, aortic valve stenosis or regurgitation more than mild severity and other valves more than moderate severity, renal impairment with 1.5 < serum creatinine, peripheral artery disease, CABG cases, and contraindications of coronary artery angiography. Moreover, patients who had MI or thromboembolism in the last three months were excluded from the study to prevent any interference with the analysis results. Informed written consent was obtained from all subjects. The study was approved by the ethical review board at Ahvaz University of Medical Sciences (ethical ID number: IR.AJUMS.REC.1397.016).
3.3. Data Collection and Central Blood Pressure Measurements
The main risk factors of CAD were extracted for all patients, based on history, examination, and medical record data. After which they underwent angiography. The central aortic blood pressure of the patients was measured during angiography. An angiographic catheter was placed in an ascending aorta and connected to a pressure transducer with a fluid-filled system to measure central systolic blood pressure (SBP) and central diastolic blood pressure (DBP).
Mean arterial pressure (MAP) and arterial pulse pressure (PP) were obtained to calculate FSP, FDP and FPP, which were FSP = SBP/MAP, FDP = DBP/MAP, FPP = PP/MAP, respectively.
3.4. Determine the Number of Diseased Vessels
The severity of coronary artery disease was also calculated by the cardiologist, and the results were divided into two groups: NO CAD and CAD. The CAD cases were then classified based on the severity of CAD with more than 50% stenosis in the form of one vessel disease (1VD), two-vessel disease (2VD), and three-vessel disease (3VD).
3.5. Statistical Analysis
In order to determine the significance of different parameters, the data collected during the current study were recorded and statistically analyzed by the SPSS program (version 22.0) and Medcalc (version 15.0). Results were expressed as mean ± SD. The Kolmogorov-Smirnov test and Q-Q plot were used to study the normality of the data.
Univariate data analysis was conducted using an independent t-test, ANOVA test, and Spearman correlation coefficient. Multivariate data analysis was carried out using ordinal regression and logistic regression. Moreover, the ROC curve was used to assess the diagnostic power of variables, and the appropriate cut-off points were obtained based on sensitivity, specificity, positive predictive value, and negative predictive value. The significance level was considered to be 0.05.
4. Results
Out of 300 subjects, the coronary artery angiography of whom was recorded, 211 patients (59.6 years ± 9.6) were classified as CAD and 89 individuals (54.45 years ± 11.9) as NO CAD. There were 163 (54.3%) males and 137 (45.7%) females (data not shown). The mean relative indices of central blood pressure (FPP, FSP, FDP, and FSP/FDP) in NO CAD patients and patients with 1VD, 2VD, and 3VD are presented in Table 1. There were significant differences in all central blood pressure indices in these groups (P < 0.001).
| NO CAD | CAD (1VD, 2VD, 3VD) | 1VD | 2VD | 3VD | P Valuea | |
|---|---|---|---|---|---|---|
| FPP | 0.52 ± 0.10 | 0.76 ± 0.14 | 0.62 ± 0.11 | 0.74 ± 0.10 | 0.88 ± 0.09 | < 0.001 |
| FSP | 1.34 ± 0.07 | 1.50 ± 0.09 | 1.41 ± 0.07 | 1.49 ± 0.06 | 1.59 ± 0.06 | < 0.001 |
| FDP | 0.82 ± 0.03 | 0.74 ± 0.04 | 0.79 ± 0.03 | 0.75 ± 0.03 | 0.70 ± 0.03 | < 0.001 |
| FSP/FDP | 1.63 ± 0.16 | 2.04 ± 0.27 | 1.80 ± 0.19 | 2.00 ± 0.19 | 2.26 ± 0.19 | < 0.001 |
Abbreviations: CAD, coronary artery disease; FDP, fractional diastolic pressure; FPP, fractional pulse pressure; FSP, fractional systolic pressure; 1VD, one vessel disease; 2VD, two vessel disease; 3VD, three vessel disease
aP Value: comparison between NO CAD and CAD
Odds ratio (OR) for the FPP, FSP, FDP, and FSP/FDP was found to be significant (P < 0.001) in CAD and 3VD subjects (Table 2). According to ordinal regression analysis in which variables such as age and sex were matched, there was a relationship between the relative indices of central blood pressure and the number of diseased vessels such that the higher the number of diseased vessels, the higher the FPP, FSP, FSP/FDP and the lower the FDP (P < 0.001) (Table 3).
| OR (%95 CI) | P Value | |
|---|---|---|
| CAD | ||
| FSP/SDP | 2.76 (2.09, 3.64) | < 0.001 |
| FPP | 5.20 (3.34, 8.08) | < 0.001 |
| FSP | 11.84 (6.11, 22.95) | < 0.001 |
| FDP | 0.007 (0.002, 0.03) | < 0.001 |
| 3VD | ||
| FSP/SDP | 2.28 (1.82, 2.85) | < 0.001 |
| FPP | 4.85 (3.15, 7.47) | < 0.001 |
| FSP | 10.68 (5.59, 20.43) | < 0.001 |
| FDP | 0.009 (0.002, 0.032) | < 0.001 |
Abbreviations: CAD, coronary artery disease; CI, confidence interval; FDP, fractional diastolic pressure; FPP, fractional pulse pressure; FSP, fractional systolic pressure; OR, odds ratio; 1VD, one vessel disease; 2VD, two vessel disease; 3VD, three vessel disease
| β | %95 CI | P Value | |
|---|---|---|---|
| FSP/FDP | 9.227 | (7.792, 10.662) | < 0.001 |
| FPP | 16.22 | (13.73, 18.71) | < 0.001 |
| FSP | 24.32 | (20.59, 28.06) | < 0.001 |
| FDP | -48.65 | (-56.12, -41.18) | < 0.001 |
Abbreviations: β, ordinal regression coefficient; CAD, coronary artery disease; CI, confidence interval; FDP, fractional diastolic pressure; FPP, fractional pulse pressure; FSP, fractional systolic pressure; 1VD, one vessel disease; 2VD, two vessel disease; 3VD, three vessel disease
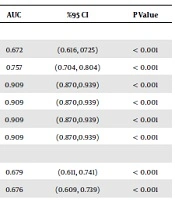
The ROC curve was used to evaluate the predictive power of central blood pressure indices (Table 4). The ROC curve for SBP, DBP, FPP, FSP, FDP and FSP/FDP was 0.672, 0.757, 0.909, 0.909, 0.909, and 0.909 for CAD diagnosis, respectively. All central blood pressure indices (especially relative indices) had predictive power for CAD diagnosis (P < 0.001). Moreover, the ROC curve for central blood pressure indices and the predictive power of the main 3VD was 0.679, 0.676, 0.894, 0.894, 0.894, and 0.894, respectively. Thus, it can be concluded that central blood pressure indices have predictive power for an increase in the number of diseased vessels (P < 0.001). This diagnostic power of 3VD in CAD patients for relative indices of central blood pressure (FPP, FDP, FSP, FSP/FDP) is higher than that of absolute indices (SBP, DBP).
| AUC | %95 CI | P Value | |
|---|---|---|---|
| CAD | |||
| SBP | 0.672 | (0.616, 0725) | < 0.001 |
| DBP | 0.757 | (0.704, 0.804) | < 0.001 |
| FSP/FDP | 0.909 | (0.870,0.939) | < 0.001 |
| FPP | 0.909 | (0.870,0.939) | < 0.001 |
| FSP | 0.909 | (0.870,0.939) | < 0.001 |
| FDP | 0.909 | (0.870,0.939) | < 0.001 |
| 3VD | |||
| SBP | 0.679 | (0.611, 0.741) | < 0.001 |
| DBP | 0.676 | (0.609, 0.739) | < 0.001 |
| FSP/FDP | 0.894 | (0.845, 0.932) | < 0.001 |
| FPP | 0.894 | (0.845, 0.932) | < 0.001 |
| FSP | 0.894 | (0.845, 0.932) | < 0.001 |
| FDP | 0.894 | (0.845, 0.932) | < 0.001 |
Abbreviations: AUC, area of ROC curve; CAD, coronary artery disease; CI, confidence interval; FDP, fractional diastolic pressure; FPP, fractional pulse pressure; FSP, fractional systolic pressure; 1VD, one vessel disease; 2VD, two vessel disease; 3VD, three vessel disease
Regarding the significant relationship between central blood pressure indices, CAD and 3VD, two cut-off points were determined; once with high sensitivity and the next time with high specificity, positive predictive value (PPV) and negative predictive value (NPV) at both cut-off points (Table 5). For example, the cut-off point of the FSP index for CAD group (all patients with 1VD, 2VD, and 3VD) was ≤ 1.373 based on 92% sensitivity, and 74% specificity. Another cut-off point of the same index was ≤ 1.421 with a sensitivity of about 77%, but a specificity of about 93%.
| Cut Points | SN (%95 CI) | SP (%95 CI) | PPV (%95 CI) | NPV (%95 CI) | ||||
|---|---|---|---|---|---|---|---|---|
| FSP/FDP | FPP | FSP | FDP | |||||
| CAD | ||||||||
| ≥ 1.688 | ≥ 0.559 | ≥ 1.373 | ≤ 0.811 | 91.94 (87.4, 95.2) | 74.16 (63.8, 82.9) | 89.4 (84.5, 93.2) | 79.5 (69.2, 87.6) | |
| ≥ 1.800 | ≥ 0.632 | ≥ 1.421 | ≤ 0.787 | 77.25 (71.0, 82.7) | 93.26 (85.9, 97.5) | 96.4 (92.4, 97.7) | 63.4 (54.5, 71.6) | |
| 3VD | ||||||||
| ≥ 2.000 | ≥ 0.750 | ≥ 1.500 | ≤ 0.740 | 86.08 (76.5, 92.8) | 79.55 (71.7, 86.1) | 71.6 (61.4, 80.4) | 90.5 (83.7, 95.2) | |
| ≥ 2.154 | ≥ 0.833 | ≥ 1.556 | ≤ 0.720 | 69.62 (58.2, 79.5) | 87.88 (81.1, 92.9) | 77.5 (66, 86.5) | 82.9 (75.6, 88.7) | |
Abbreviations: CAD, coronary artery disease; CI, confidence interval; FDP, fractional diastolic pressure; FPP, fractional pulse pressure; FSP, fractional systolic pressure; NPV, negative predictive value; PPV, positive predictive value; SN, sensitivity; SP, specificity; 3VD, three vessel disease
5. Discussion
Studies have been conducted on central aortic blood pressure indices such as FPP, FSP and FDP, and their association with cardiovascular outcomes, confirming the association of these indices with the increased risk of cardiovascular disease and an increase in the severity of coronary artery disease (10, 12, 13). Previous studies have reported the association between central blood pressure and cardiovascular diseases (3, 5, 6). Moreover, Jankowski et al. showed that PP, FSP, and FDP of the central aorta were associated with the risk of 3VD in CAD patients. They stated that the risk of 3VD increases by 15%, 28%, and 39% per 10 mmHg increases in the central PP, per 0.1 increases in FSP and per 0.1 reductions in FDP, respectively (14). As observed in this study, there was a significant association between increased FPP, FSP and FSP/FDP, decreased FDP, and the higher risk of 3VD (FPP 4.85, FSP 10.68, FDP 0.009 and FSP/FDP 2.28) (P < 0.001). Moreover, there was a significant correlation between increases in central blood pressure indices (FSP/FDP, FSP, FPP), reduction of FDP as well as increases in the number of diseased vessels. However, both odds ratio (11.84; 95% CI: 6.11 - 22.95; P < 0.001) and ROC analysis (AUC: 0.909; 95% CI: 0.870 - 0.939; P < 0.001) showed FSP as the strongest predictor of CAD. In another study, Nakayama et al. showed that FDP, but not FSP, is independently associated with CAD risk in patients undergoing coronary angiography (11). In our study, it was shown that lower FDP values, as well as higher FSP values, are associated with an increased risk of CAD. It means that a lower level of FDP accompanied by increases in other central blood pressure indices could be a suitable marker for predicting the number of involved vessels.
Moreover, it was shown that there is an association between the central blood pressure indices, in particular, its relative indices (FPP, FDP, FSP, and FSP/FDP), in patients undergoing CAD and an increase in the number of diseased vessels (P < 0.001). Furthermore, The ROC curve suggested that FPP, FDP, FSP, FSP/FDP have higher predictive power than absolute indices (SBP and DBP) for the occurrence of CAD and also an increase in the number of diseased vessels (P < 0.001) (Table 4).
In this study, the probability of CAD and 3VD was predicted for the first time by using cut-off points based on sensitivity, specificity, NPV, and PPV. The cut-off points of the FSP (≥ 1.373), FDP (≤ 0.811), FPP (≥ 0.559) and FSP/FDP (≥ 1.688) for CAD were determined in this study based on 92% sensitivity and 74% specificity. Additionally, cut-off points of FSP (≥1.500), FDP (≤ 0.740), FPP (≥ 0.750) and FSP/FDP (≥ 2.000) were determined for 3VD with 86% sensitivity and 80% specificity.
5.1. Conclusions
Central blood pressure indices, such as FPP, FDP, FSP, FSP/FDP may be associated with increased diseased vessels in CAD. However, FSP has been shown as the strongest predictor of CAD in Iranian populations. Therefore, the quality of life may be improved by the management of blood pressure treatment based on central blood pressure control and using cut-off points.
5.2. Study Limitations
1. There were a limited number of patients, and we used a small group who were referred for elective CAG.
2. A fluid-filled system was used to record coronary BP, while the use of a high-fidelity pressure transducer can increase the accuracy of the recorded pressure in this study. So, high-fidelity pressure transducer might be used as an advanced pressure measurement device in future clinical studies.