1. Background
Multiple sclerosis (MS) is a chronic inflammatory demyelinating autoimmune disease of the central nervous system (1). There are different types of MS including relapsing-remitting, primary progressive, secondary progressive, progressive-relapsing, and benign sensory MS (2). Although the age range of MS patients is 20 to 50, MS mainly affects young people. It is three times more prevalent among women (2). The number of patients with MS in the world, United States, and England has been reported to be around 2.5 million, 400,000, and 85,000, respectively, Moreover, 189 per 100,000 population in Sweden were reported to have MS (3-5). Statistics provided by the Iranian MS Association show that with around 50,000 MS patients, Iran has the first rank in the Middle East (6).
Patients with MS not only suffer from a wide range of physical health problems including diplopia, loss of balance, dizziness, sensorimotor disturbances in the limbs, genitourinary disorders (such as impotence and incontinence), and constipation, but also experience different levels of depression and anxiety (3). Most patients with MS experience depression due to the unpredictable and debilitating relapses of the disease and their effects on their lives (7). Moreover, the suicide rate is significantly high among this patient population due to their social isolation (8, 9). The risk of developing depression is about 30% - 50% among MS-afflicted patients while it is just around 10% - 15% in the general population (10, 11).
Depression and anxiety are among the main factors behind the reduced quality of life. Moreover, depression can reduce the effectiveness of MS treatments (12). Besides, due to the frequent relapses of MS, dependence on others, and inability to fulfill personal needs, patients with MS are usually preoccupied with their self-concept and the meaning of their lives (13).
Spiritual interventions are among the therapies for depression and anxiety (14, 15). Many studies have assessed the correlation of spirituality with life satisfaction, quality of life, psychological well-being, depression, and anxiety (16-18). Religiosity and spirituality have been reported to be the sources of adaptation to stressful life events such as significant losses (8). Rafferty et al. (16) also noted that spirituality is one of the strategies that must be adapted to chronic conditions. Moreover, studies found that after affliction by a chronic painful condition, patients displayed a greater tendency towards religiosity and spirituality (19). As a framework, spirituality provides individuals who experience crises a sense of ultimate goal and meaning in life, stability, support, and guidance (20).
Studies show that education programs can enhance people’s spiritual well-being (21-23). Thus, one of the best ways of enhancing psychological well-being has been reported to be direct education and reflective programming (21). Besides, the most effective teaching strategies were reported to be those that actively engage learners in discussions and activities (24).
Spiritual education is a challenging work (25) due to the complex and abstract nature of spirituality and its difficult quantification (26). Some scholars have attempted to quantify spirituality through subjective concepts such as hope and adaptation (26, 27). However, there are still controversies about its quantification.
Previous studies mainly assessed the effects of spiritual interventions such as reading holy books, listening to the Holy Quran, praying, spiritual discussions, meditation, and virtual spiritual education (28-31). Some other studies also focused on using spiritual psychotherapy for managing depression and anxiety (32, 33) and psychological interventions such as cognitive-behavioral therapy and mindfulness-based cognitive therapy. However, these interventions are usually expensive and time-consuming and thus, people have limited adherence to them (34, 35).
2. Objectives
Consequently, the present study was done to assess the effects of a multi-component spirituality education program on anxiety and depression among patients with MS.
3. Methods
This pretest-posttest two-group randomized-controlled trial was made in 2018 on a convenience sample of 64 patients with MS who referred to Alborz Province MS Association, Karaj, Iran. With a power of 80% and a confidence level of 95%, considering that the standard deviation of the anxiety of two groups according to a study by Bolhari et al. (36), 2012 was 9.42 and 5.1, it was determined that 27 patients were needed for each study group. The selection criteria were a definite diagnosis of MS based on patients’ medical records, having at least one-year history of suffering from MS, having a minimum age of 20 and maximum of 50, obtaining score 16 to 28 from the Beck Depression Inventory (i.e. mild to moderate depression), obtaining score 12 - 26 on the Beck Anxiety Inventory (mild to moderate anxiety), no history of psychotic disorders, dementia, or delirium (based on their medical records), no history of using psychiatric medications (such as anxiolytic, antidepressant, or mood-stabilizing agents) in the past one month, no drug addiction (based on their medical records), no use of psychological therapies, and having an education level of guidance school or higher. Patients were excluded if they started using psychological therapies or experienced a relapse of MS during the course of the study.
3.1. Instruments
The study instruments were the 21-item Beck Depression Inventory (BDI) and the 21-item Beck Anxiety Inventory (BAI). Each item of BDI measures the severity of one aspect or one symptom of depression. The score of each item ranges from 0 (i.e. “no problem”) to 3 (i.e. “the severest state of the problem”). Thus, the total score of BDI can range from 0 to 63. The BDI total score is interpreted as follows: 0 - 15: asymptomatic; 16 -22: mild depression; 23 - 28: moderate depression; 29 - 38: severe depression; and 39 - 63: very severe depression. The Persian version of BDI was reported to have acceptable reliability and validity (37).
The BAI consists of 21 items. Possible answers to BAI items include “never”, “mild”, “moderate”, and “severe” that are scored 0, 1, 2, and 3, respectively. Therefore, the total BAI score may range from 0 to 63. Scores of greater than 12 show affliction by anxiety (38). The total score of BAI was reported to have a significant correlation with the total score of the Hamilton anxiety rating scale (r = 0.72), confirming its criterion validity. Moreover, the test-retest correlation coefficient and Cronbach’s alpha value of the inventory were reported to be 0.83 and 0.92, respectively (38, 39).
3.2. Intervention
To invite patients to the study, we initially hung invitation posters in Alborz MS Association, all healthcare centers, neurologic and rehabilitative care clinics, and pharmacies that sold MS-related medications in Karaj, Iran. Consequently, 224 patients announced their consent for participation in the study. They were asked to complete the study questionnaire and then, 64 eligible patients were recruited to the study. We randomly and evenly allocated them to an experimental group and a control group using a table of random numbers. For patients in the experimental group, a spirituality education program was implemented in eight 90-min weekly sessions in the MS association. The program was developed through reviewing the programs and interventions used in previous studies (15, 28, 29, 31, 32), and contained spirituality-related components such as the goal and meaning in life, patience, reliance on God, forgiveness, beneficence, repentance, praying and benediction, thanksgiving, and meditation (Table 1). Spirituality educations were provided by a clinical psychologist and a counseling psychologist who held master’s degrees and were licensed and experienced in spirituality education. The sessions were organized by the group teaching method and time was given to the participants to ask their questions. Between educational sessions, we were in contact with the patients in the experimental group through social networking to supervise their engagement in spiritual exercises. The control group also was in contact with us separately and asked questions via social media. To facilitate the patients’ participation in the sessions, free transportation services were provided to them. On the other hand, patients in the control group were provided with routine MS-related educations and pamphlets. All patients in both groups were asked to avoid using any pharmacological or non-pharmacological therapies for anxiety and depression. Four weeks after the last educational session, the levels of patients’ anxiety and depression were reassessed in both groups.
| Sessions | Topic | Contents |
|---|---|---|
| 1 | Recognizing goal and meaning in life | Assessment of goal and meaning in life |
| 2 | Patience and reliance on God | Practical methods for relying on God; strategies for promoting patience |
| 3 | Repentance | Principles, conditions, and rites of repentance |
| 4 | Praying and benediction | Effects of praying and benediction on intra and inter-personal relationships |
| 5 | Spiritual meditation | Effects of meditation |
| 6 | Forgiveness | Types of forgiveness; finding the relationship between inability to forgive self and others |
| 7 | Thanksgiving and beneficence | Types of thanksgiving |
| 8 | Review of the previous sessions |
A Summary of the Spirituality Education Program
The SPSS software (V. 21) was employed for data description and analysis through frequency distribution tables and independent-sample t-tests. Moreover, the repeated-measures ANOVA was used to determine the difference between the mean scores of the two groups at the baseline and after the intervention. This study was approved by the Ethics Committee of Alborz University of Medical Sciences, Karaj, Iran. The approval code was abzums.rec.1394.39. The study was registered with IRCT.IR (registration number: IRCT20170404033212N2). Informed consent was obtained from all participants.
4. Results
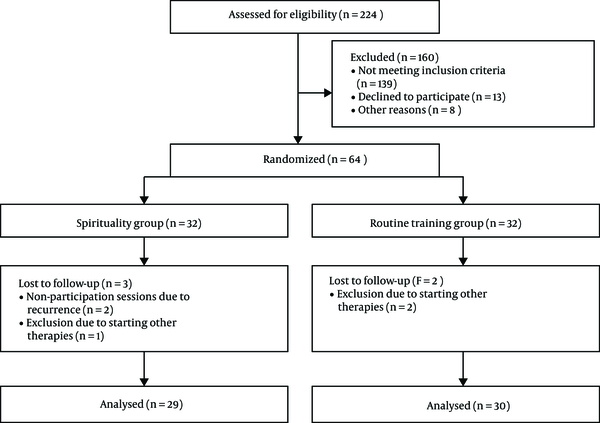
In total, 224 volunteers announced their consent for participation in the study and completed the study questionnaires. Then, 139 were excluded. Moreover, 13 individuals voluntarily withdrew from the study and eight individuals failed to attend educational sessions due to personal or familial problems. During the study, three patients were excluded from the experimental group due to experiencing an acute relapse of MS (two patients) and using psychological therapies (one patient). On the other hand, two patients were excluded from the control group due to using psychological therapies (Figure 1).
All participants were Muslim. Moreover, while 30.8% of the participants had not experienced any relapse of MS during the past year, most of them had experienced one, two, or more than two relapses (36.5%, 15.4%, and 17.3%, respectively).
The results of the Kolmogorov-Smirnov test showed that the distribution of depression and anxiety scores before the intervention was normal. The independent-sample t-test revealed no significant between-group difference regarding the baseline mean scores of depression and anxiety (P > 0.05; Table 2). However, the posttest mean scores of depression and anxiety were significantly lower in the experimental group than in the control group (P < 0.05). Moreover, the results of the repeated-measures ANOVA test illustrated that in the experimental group, the depression score significantly decreased from 22.86 ± 3.86 at baseline to 14.27 ± 4.62 after the intervention (P < 0.001). Additionally, the anxiety score in this group significantly decreased from 20.82 ± 4.26 at baseline to 13.55 ± 4.74 after the intervention (P < 0.001). However, in the control group, the posttest depression and anxiety scores did not significantly differ from the corresponding pretest scores (P > 0.05; Table 3). The result of the analysis of covariance (ANCOVA) for anxiety showed that there was a significant difference between the case and control groups after the deletion of the pretest score effect. After the removal of the effect of the pretest depression scores, there was also a significant difference between the two groups.
| Group Characteristics | Experimental (N = 29) | Control (N = 30) | Sig. (χ2) |
|---|---|---|---|
| Age, mean | 33.88 | 33.85 | 0.23 |
| Gender | 0.536 | ||
| Male | 9 (31) | 20 (69) | |
| Female | 10 (33.3) | 20 (66.7) | |
| Marital status | 0.448 | ||
| Single/widowed/divorced | 16 (55.2) | 14 (46.6) | |
| Married | 13 (44.8) | 16 (53.4) | |
| Educational status | 0.395 | ||
| Guidance school | 3 (10.3) | 7 (23.3) | |
| Diploma and associate degree | 18 (62.1) | 15 (50) | |
| Bachelor’s and higher degrees | 8 (27.6) | 8 (26.7) | |
| Length of suffering MS | 0.517 | ||
| 1 - 3 years | 10 (34.5) | 10 (33.3) | |
| 3 - 5 years | 8 (27.6) | 5 (16.7) | |
| 5 - 10 years | 8 (27.6) | 8 (26.7) | |
| > 10 years | 3 (10.3) | 7 (23.3) | |
| Employment status | 0.262 | ||
| Employed | 13 (44.2) | 10 (33.3) | |
| Unemployed | 16 (55.8) | 20 (66.7) | |
| Depression before | |||
| Mild (16 - 22) | 13 (44.8) | 15 (50) | |
| Moderate (23 - 28) | 16 (55.2) | 15 (50) | |
| Anxiety before | |||
| Mild (8 - 15) | 4 (13.8) | 2 (6.7) | |
| Moderate (16 - 25) | 25 (86.2) | 28 (93.3) |
Baseline Demographic Characteristicsa
5. Discussion
The aim of this study was to assess the effects of a multi-component spirituality education program on anxiety and depression among patients with MS. The findings revealed that after the eight-session spirituality education program, the mean scores of depression and anxiety decreased significantly (P < 0.001). We were going to study the long-term outcomes of spiritual education. Given that many factors can affect anxiety and depression, it was not possible to control and monitor them, as previous studies showed that the effects of education decreased after eight weeks (40). Therefore, four weeks after intervention were considered as the appropriate time for measurement. Similarly, McCauley et al. (39) carried out a study to assess the effectiveness of a spirituality-based intervention on chronically ill patients’ health and found that their intervention was effective in reducing depressive symptoms and promoting adaptation. Moreover, Zamaniyan et al. (28) reported the effectiveness of spiritual group therapy in enhancing the quality of life and the psychological well-being of patients with breast cancer. In addition, Rickhi et al. (40) found that their spirituality education program significantly reduced the depression severity and increased the depression response and remission rates during a six-month follow-up period. The response rate in their study was as high as 56% - 64% (40). Previous studies indicated that the recovery rates of antidepressant agents were 44% - 71% while the recovery rates of cognitive-behavioral therapies were 36% - 44% (41, 42). All these findings showed the great effectiveness of spirituality education in reducing the symptoms of depression and anxiety. Other studies also reported the positive effects of spirituality-based interventions on the outcomes of patients with schizophrenia, chronic renal diseases, cancer, and irritable bowel syndrome (16, 17, 28, 31, 43).
Most patients with depression and anxiety have poor adherence to their pharmacological treatments due to the side effects of antidepressant and anxiolytic agents. Some antidepressants, such as selective serotonin reuptake inhibitors (SSRIs), can exacerbate the complications of MS such as fatigue and sexual dysfunction (44). In addition, the choice of medication varies from person to person due to differences in the type of problem and course of the disease (45). On the other hand, cognitive therapies do not pay attention to the spiritual dimensions of patients despite being costly and time-consuming. Thus, spirituality education can be used as an appropriate complementary therapy along with pharmacological and cognitive-behavioral therapies, which are used to manage depression and anxiety in people with MS.
5.1. Study Limitations
We could not completely separate the patients in the study groups and prevent them from contacting each other. Moreover, the study was done in a short period only on patients with mild and moderate depression and anxiety. Another point, which may limit the generalizability of the findings, is the fact that most of our participants were women aged 30 - 40. Therefore, our findings may not be generalizable to all patients and it requires further research.
5.2. Conclusions
The findings of the present study showed that spirituality education was effective in reducing the symptoms of depression and anxiety among patients with MS. Thus, spirituality education programs need to be implemented by MS associations to support patients with MS and reduce their depression and anxiety. Moreover, given the positive effects of spirituality-related components such as praying, benediction, and repentance, clergies can be invited for providing spirituality educations.