1. Background
Neuroblastoma (NB) is a pediatric solid tumor with heterogeneous features, aggressive behavior, and a high mortality rate. The prevalence of this malignancy is 8% to 10% of all common cancers in children (1, 2). Multiple therapeutic approaches have been taken and applied in clinics to cure neuroblastoma, including surgery, radiotherapy, chemotherapy, immunotherapy, stem cell transplant, and retinoids (3-5) Nevertheless, resistance to therapies, being somehow inevitable, occasionally leads to treatment failure and cancer relapse (6). Hence, understanding the mechanisms of minimization of drug sensitivity that leads to therapy resistance and discovering reversal strategies is crucial. These experiments might provide evidence for the application of combinatorial therapy for treatment and prolonged survival of patients with NB, as to the application of chemotherapeutic agents with combination regimens for target therapy.
According to the Epidemiology data, the incidence of NB has been reported higher in high-income countries (HICs) than in low- and middle-income countries (LMICs); though, the limitations of diagnosis and management must be considered in such reports (7). Regarding the heterogeneous nature of NB, scientists suggested to determine the molecular mechanisms underlying tumor progression, metastasis, and drug resistance, further studies must be carried out to understand the tumor biology (7). Based on the scientific data, the increase in the incidence of cancer and neurological disorders, decreased drug sensitivity, and enhancement of treatment side effects are due to metabolic abnormalities (8). Metabolic imbalance induces perturbation of the molecular signaling and cell-microenvironment interactions, resulting in an increased rate of therapeutic failure and mortality (8-10). One of the main factors deregulated in the membrane of most cancer cells is the glycosylation pattern of tumor cells (11). Disruption of sialic acid metabolism drives tumor growth, metastasis, and cancer resistance to chemotherapy (12).
As a platinum-based drug, carboplatin forms highly reactive platinum complexes used in the treatment of NB. Carboplatin binds and crosslinks DNA to prevent the growth of cancer cells and cause cell death (13). Although the intrinsic or acquired resistance caused by complicated mechanisms significantly causes a decrease in the efficacy of the pharmaceutical treatments in drug resistance of cancers (14), the overexpression of efflux transporters might have a role in the active excretion of platinum-based antitumor agents from cancer cells. Besides, cellular platinum accumulation and therapeutic efficacy are deceased (15) and cause a decrease in the anti-cancer activity of carboplatin in cells with inhibited apoptosis signaling. The inactivation of BAX and activation of BCL-2, as apoptotic and anti-apoptotic factors, are known as two main factors involved in the molecular scenario beyond dysregulation of apoptosis (16). Decrease of the BAX/BCL-2 ratio, as an apoptotic marker, and overexpression of the efflux transporter contributes to the decreased therapeutic efficacy of carboplatin (16). MRP1 encoded by ABCC1, prevalent in neuroblastoma, is the multidrug resistance protein (as a transporter protein) important in transporting many chemotherapeutic drugs out of the cells (17).
2. Objectives
In the present study, the effects of Sialic acid, carboplatin, and their combination (Sia-CBDCA) were evaluated on the viability and morphological features of SH-SY5Y cells; moreover, the expression of BAX/BCL2 as apoptotic ratio and ABCC1 were assessed using real-time PCR.
3. Methods
3.1. Chemicals
Sialic acid (N-acetyl neuraminic acid: NANA) and all other chemical reagents were purchased from Qiagen company (Hilden, Germany), Sigma-Aldrich Chemical Company (St. Louis, MO, USA) and Merck Company (Darmstadt, Germany).
3.2. Neuroblastoma SH-SY5Y Cells Culture
The SH-SY5Y cell line was gifted by Sara-Co institute. Using DMEM-F12, the cell culture was performed with 1% penicillin (5000 U/mL)-streptomycin (5000 mg/mL), and 10% fetal bovine serum (FBS). They were incubated at 37°C with 95% humidity and 5% CO2.
3.3. Cell Viability Assay (EC50 and IC-50 Assessment)
MTT assay was performed for cell viability measurements. In short, the SH-SY5Y cancer cells were seeded in a 96‐well plate (0.5 × 104 cells per well) and were incubated for 24 hours under standard conditions. After reaching 70% confluence, the cells were treated for 48 and 72 hours with different concentrations of sialic acid (NANA). For EC50 assessment in 48 and 72 h, cells were treated with 1 - 800 μM 50 - 400 μM sialic acid, respectively. For IC50 assessment, cells were treated with 100 - 2000 μM 100 - 1000 μM sialic acid, respectively. For the IC50 assessment of carboplatin, cells were treated with 20 - 300 μg/mL and 10 - 200 μg/mL carboplatin, respectively. Eventually, for the IC50 changing assessment of carboplatin in combination with sialic acid, the cells were treated with the half-maximal inhibitory concentration of carboplatin in the presence of an enhanced concentration of sialic acid for each time. After this time, 30 μL (3‐[4,5‐Dimethylthiazol‐2‐yl]‐2,5‐diphenyltetrazolium bromide) of MTT solution (0.5 mg/mL reagent in PBS) was replaced with the previous medium, and it was incubated for four hours in a standard condition. Then, 120 μL dimethyl sulfoxide was added, and the solution was incubated for 20 min; finally, the optical absorbance was measured using ELISA Reader (Bio Intellectica Scientific INC, Canada) for each well at a wavelength of 570 nm. The percentage of inhibition concentration was measured as [1- (optical density of test/ optical density of negative control)] × 100. The EC50 value (the concentration of 50% cell effectiveness) and IC50 value (the concentration of 50% cell inhibition) were calculated from the effectiveness and inhibition percentage graph against different concentrations.
3.4. Gene Expression Assay
Cells were divided into 4 groups: Control, sialic acid, carboplatin, and sialic acid + carboplatin. The SH-SY5Y cancer cells were seeded separately into six‐well plates at a density of 1.5 × 105 cells per well and were incubated for 24 hours. The cancer cells were treated with sialic acid, sialic acid/carboplatin, and carboplatin at a concentration close to the effective concentration and IC50 of sialic acid and carboplatin, respectively, for 48 hours. According to the manufacturer's instructions, Qiazol reagent was used for total RNA extraction. RNA quality and quantity were analyzed by electrophoresis on 1% agarose gel and NanoDrop instrument (Thermo ScientificTM NanoDropTM One Microvolume UV-Vis Spectrophotometers). Then, cDNA was synthesized using 2 μg of total RNA by M-MLV RT kit (Yekta Tajhiz Azma). The expression of ABCC1, BAX, and BCL2 was measured using qRT-PCR. The sequence of the primers is listed in Table 1. The RT-PCR reactions were up to 10 μL including 5 μL SYBR Green Master Mix (Yekta Tajhiz, Tehran, Iran), 2 μL cDNA, and 0.8 μL forward and reverse primers (10 μM). The q-RT PCR program was 1 cycle of 94°C for 1 minute, followed by 40 cycles of denaturation and annealing/extension at 94°C for 10 seconds and 60°C for 30 seconds, respectively. The ACTB was used as the housekeeping endogenous control for RT-data normalization. One-step Real-Time PCR Equipment (Applied Biosystems) was utilized for PCR. The calculations were performed by the 2−ΔΔCt (Livak) formula.
| Title | Sequence (5'→3') | Tm | Product Size (bp) |
|---|---|---|---|
| ABCC1 | 128 | ||
| F | GGAGGACACGTCGGAACAA | 59.64 | |
| R | AACTCTCTTTCGGCTGGGC | 60.00 | |
| BCL2 | 133 | ||
| F | CACCCCCTCGTCCAAGAATG | 60.39 | |
| R | TCCCAGAGGAAAAGCAACGG | 60.25 | |
| BAX | 94 | ||
| F | GATGATTGCCGCCGTGGAC | 61.82 | |
| R | CCGGCCCCAGTTGAAGTTG | 61.27 | |
| ACTB | 103 | ||
| F | GAGCATCCCCCAAAGTTCACA | 60.55 | |
| R | GGGACTTCCTGTAACAACGCA | 60.54 |
3.5. Statistical Analysis
All experiments were repeated three times. The data from treated and untreated cells in three independent experiments were presented as mean ± standard deviation. The statistical analyses were performed by the paired-student t-test. Differences with P < 0.05 and P < 0.01 were considered significant (*)and more significant (**).
4. Results
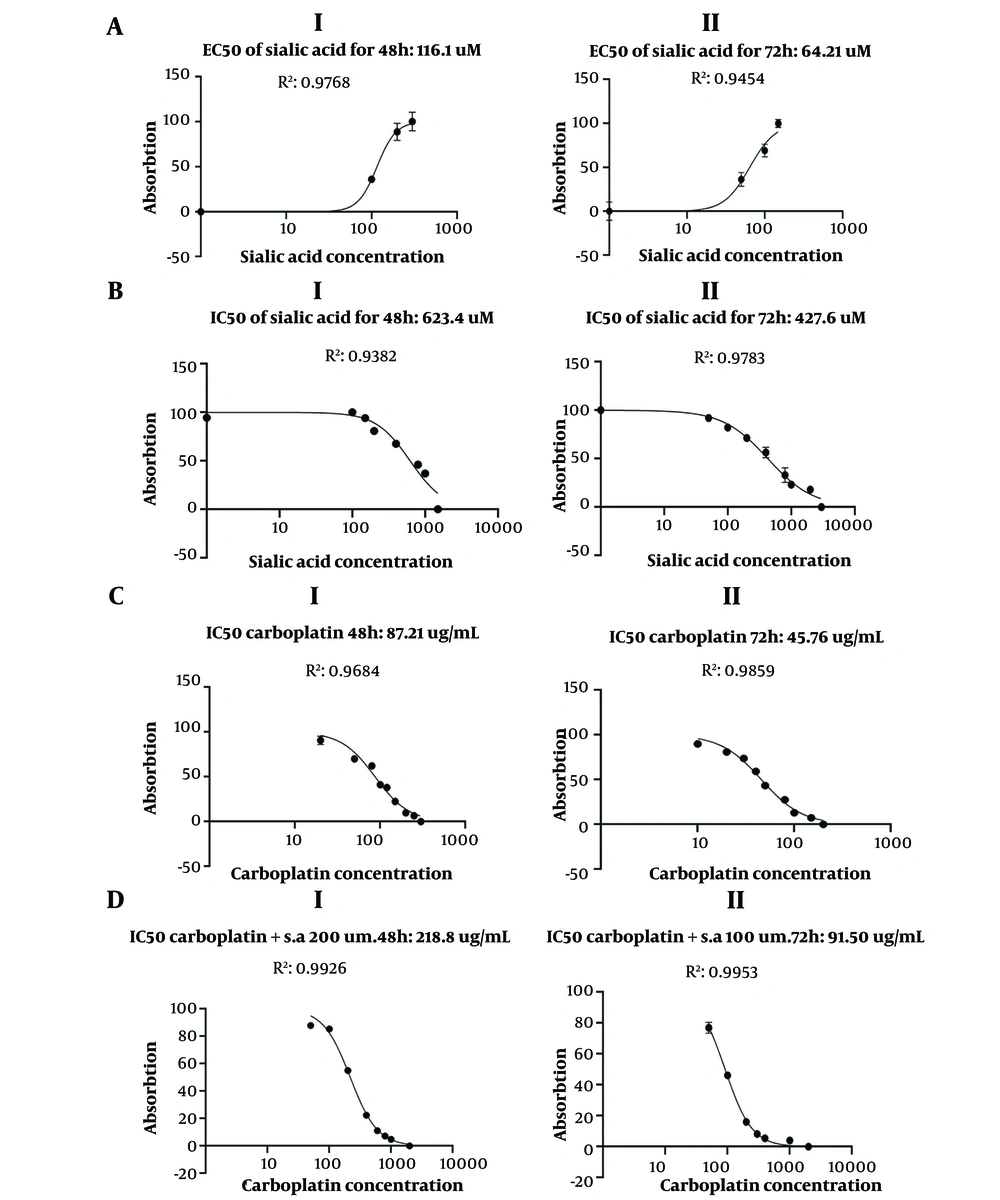
4.1. Cancer Cell Viability
In our study, the half-maximal effective concentration (EC50) of sialic acid was determined depending on the time and concentration manner that reflects the metastatic potency of sialic acid. MTT assessment revealed that sialic acid treatment could significantly increase the cell viability of the neuroblastoma cell line. According to the MTT results, the present study showed that the anticancer effect of carboplatin was in a time- and concentration-dependent manner, modulated with a combination of sialic acid treatment. The enhanced of sialic acid, and inhibited concentrations of sialic acid, carboplatin, and a combination of of sialic acid + carboplatin in the effective concentration in the enhanced concentration + half maximal Inhibitory concentration, respectively, on SH-SY5Y cell line were defined as EC50 = 116.1 μM/ IC50 = 623.4 μM for sialic acid (Figure 1AI and BI), IC50 = 87.21 μg/mL for carboplatin (Figure 1CI) and IC50 = 218.8 μg/mL for carboplatin in combination with sialic acid treatment for 48 h (Figure 1DI) (S1; cell viabilities are illustrated by *, *, *, **, respectively, also, the cytotoxic activities of carboplatin alone and in combination with sialic acid are demonstrated by bidirectional arrow) and EC50 = 64.21 μM/ IC50 = 427.6 μM for sialic acid (Figure 1AII and BII), IC50 = 45.76 μg/mL for carboplatin (Figure 1CII) and IC50 = 91.50 μg/mL for carboplatin in combination with sialic acid treatment (Figure 1DII) for 72 h (S2; cell viabilities are illustrated by *, *, *, **, respectively. Also, the cytotoxic activities of carboplatin alone and in combination with sialic acid are demonstrated by bidirectional arrow). It is important to note that our observations are in concordance with other data indicating that sialic acid promotes cell viability and survival and has no significant cytotoxicity effect on cell lines. It is worth noting that IC50 is merely determined based on a little decrease in absorbance and no significant change in that.
4.2. Gene Expression Assay
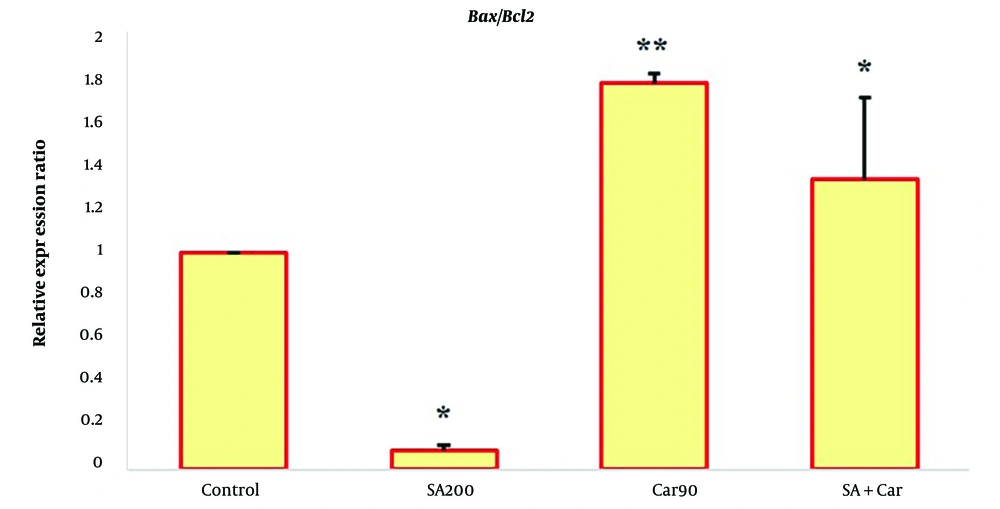
To better understand the metastatic and apoptosis effects of sialic acid, carboplatin, and the combinatorial effect of sialic acid and carboplatin in 2*EC50 of sialic acid and IC50 of carboplatin, we studied the expression of BAX as pro-apoptotic and BCL2, as anti-apoptotic gene expression in these groups. Notably, some research has reported that the BAX/BCL2 ratio, a prognostic marker, determines cell susceptibility to apoptosis. Furthermore, multidrug resistance protein 1 (MRP-1) expression encoded by ABCC1 was studied in these groups.
4.2.1. The Effect of Sialic Acid on the BAX/BCL2 Ratio
After being treated with sialic acid, the BAX expression has remained unchanged. Besides, the BCL2 expression was induced approximately 16-fold. Compared with the untreated cells, a noticeable difference in BCL2 expression was observed in SH-SY5Y treated cells. This increase is associated with other data about cell proliferation and viability verified by MTT assay (Figure 2).
The expression analysis in NBs by qRT-PCR for the BAX and BCL2 gene. Bars were performed in sialic acid, carboplatin, and sialic acid-carbo-treated cells, compared to the untreated cells as control (200 uM and 90 ug/mL as effective concentration and inhibitory concentration of sialic acid and carboplatin, respectively, and 2*EC50 of sialic acid/IC50 of carboplatin on NBs) (*, **, statistical significance and more significance; P < 0.05 and P < 0.01, respectively).
4.2.2. The Effect of Carboplatin on the BAX/BCL2 Ratio
Carboplatin treatment induced the expression of BAX about 11 times. Also, in the case of BCL2, the expression induction was about 9 times higher. The ratio change was 1.74 compared with 1in the control group, proving carboplatin's apoptotic effect (Figure 2).
4.2.3. The Effect of Sia-Carbo (CBDCA) on the BAX/BCL2 Ratio
Carboplatin treatment in sialic acid's presence induced BAX's expression about 46.36 times higher. This expression induction for BCL2 was about 52.17 times. The BAX/BCL2 ratio, which is an indicator of apoptosis, changed from 1/1 in control cells to 46/52.17 in the treated cells, which proved the anti-apoptotic effect and resistance to apoptosis of SH-SY5Y cells reflecting the metastatic and anti-apoptotic effect of the sialic acid. In the case of treatment with carboplatin, this ratio was 11/9, which, by comparing the ratio of 46/52.17, i.e., 1.22 to 0.88, decreased the apoptotic index in the presence of sialic acid. An important case is to examine the expression at the protein level for further confirmation (Figure 2).
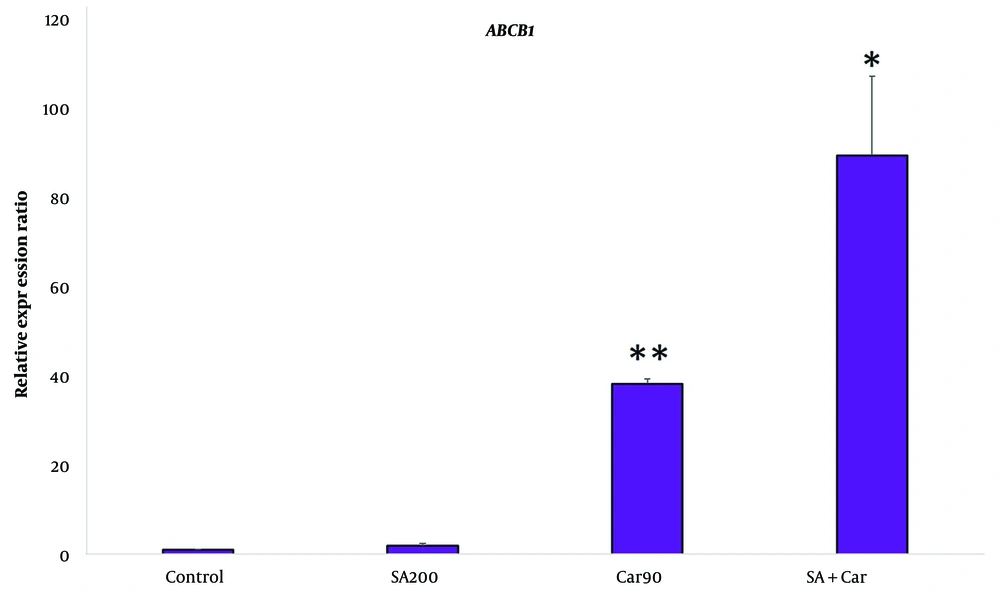
4.2.4. The Effect of Sialic Acid, Carboplatin, and Sia-Carbo Treatment on ABCC-1 mRNA Expression
Real-time PCR was used to measure the differences in the ABCC1 mRNA expression level in sialic acid, carboplatin, and Sia-Carbo-treated (treated by sialic acid in combination with carboplatin) neuroblastoma compared to the untreated cells. As shown in Figure 3, the ABCC1 mRNA expression level in the treated cells was approximately 2.5, 40, and 90 times more than in untreated cells (Figure 3).
The expression analysis in NBs by qRT-PCR for the ABCC-1 gene. Bars were performed in sialic acid, carboplatin, and sialic acid-carbo-treated cells, compared to the untreated cells as control (200 uM and 90 ug/mL as effective concentration and inhibitory concentration of sialic acid and carboplatin, respectively, and 2*EC50 of sialic acid/IC50 of carboplatin on NBs) (*, **, statistical significance and more significance; P < 0.05 and P < 0.01, respectively).
5. Discussion
One of the biggest obstacles in cancer treatment is drug resistance. Scientists have suggested that intrinsic resistance might cause the initial response to therapy, such as specific cell membrane transporter proteins. The acquired genetic and epigenetic modifications in cancer cells could impart in drug resistance development (6). One of the main intrinsic factors deregulated in the cancer cell membrane is the sialic acid involved in the interplay between the tumor microenvironment and cancer cells, physically and chemically (18). Sialic acid can mask cell membranes and antigens, evading immune response (19). It can also trigger the underlying mechanisms involved in cell proliferation, angiogenesis, and metastasis, especially with the upregulation of CDCP1 as a metastatic marker (manuscript under revision). Having a significant role in tumor genesis and cell proliferation, metastasis induction, immune evasion, and drug resistance, hypersialylation is a beneficial target for cancer therapy, i.e., the development of sialyltransferase blocking and strategies to block Siglecs and selectins as its receptors (20).
It has been well documented that ST6Gal-I sialyltransferase activity blocked cell death induced by cisplatin in ovarian tumor cells (21). Recently, overcoming drug resistance and combating tumor progression and metastasis in cancer cells using combination therapy has attracted great attention, especially regarding the whole exome sequencing and transcriptome data through targeting various mechanisms contributing to cell proliferation, progression, metastasis, and drug resistance (22).
Depending on the type of cancer, carboplatin can be used by itself or in combination with other chemotherapy drugs. Although multidrug transporters, especially in childhood neuroblastoma, the ATP-binding cassette, subfamily C (ABCC) transporters, have been reported to play an important role in cytotoxic drug efflux and mediating drug resistance. It is noted that decreasing the apoptotic ratio (BAX/BCL2 ratio as pro-apoptotic/anti-apoptotic ratio) can cause drug resistance (23).
In the present study, we compared the metastatic, anticancer activity and drug sensitivity modulation with a 48 hours treatment of the sialic acid (200 uM), carboplatin (90 uM), And Sia-Carbo (200 - 90 uM) combination in SH-SY5Y cells and possible involved mechanisms. The results revealed that the treatment of sialic acid caused a significant decrease in the BAX/BCL2 ratio in neuroblastoma, which agrees with the other studies that showed the metastatic effect of sialic acid in different cancer cells. Furthermore, our study showed a sialic acid reduction in the anti-cancer activity of carboplatin on SH-SY5Y cells by induction of viability and metastatic and anti-apoptosis induction, which was shown by an increase in IC50 of carboplatin. These facts suggest that sialic acid can be a major drug response challenge and cause drug failure.
Reduction of drug sensitivity and anti-apoptosis are important mechanisms of therapy failure in various cancer cells. The results revealed that the reduction and modulation of apoptosis rate of SH-SY5Y cancer cells was increased following the treatment with Sia-Carboplatin, significantly more than carboplatin. This reflects sialic acid's neutralizing effect and chemotherapy toxicity prevention. Previous studies have reported that sialic acid can induce drug resistance in various cancer cells. One of the main factors involved in drug resistance is P-glycoprotein transporters. MDR1 is a primary active transporter that pumps various compounds out of the cells using ATP hydrolysis. Its activity impacts clinical outcomes and toxicity. Providing resistance to cancer chemotherapeutic agents, multidrug resistance protein 1 is considered a major cause of treatment failures. As MDR1 transports a wide range of chemotherapy drugs, such as anthracyclines, vinca alkaloids, taxanes, etoposide, mitoxantrone, bisantrene, and the histone deacetylase inhibitor depsipeptide (24, 25), targeting inhibition of MDR1 could theoretically improve the clinical outcomes for many cancers. Early studies identified MDR1 expression as a significant prognostic indicator in several childhood cancers (26), and more recent studies have linked MDR1 expression to poor outcomes in leukemias and breast cancer. By the decrease of sensitized NB to carboplatin, the ABC transporter inducer increases proliferation and metastasis. Therefore, we evaluated the mRNA expression of the MDR1 gene in SH-SY5Y with sialic acid, carboplatin, and Sia-Carbo. The results showed that sialic acid treatment can upregulate ABCC1 expression, which is more upregulated in carboplatin treatment and might reflect drug resistance induction. As demonstrated, sialic acid, in combination with carboplatin, can cause an evaluation of ABCC1 expression significantly, and synergistically, drug resistance is increased. We can demonstrate that the combinational treatment of Sia-Carbo neutrally favored the anti-apoptotic pattern of BCL-2 and BAX expression. According to the results, the apoptotic, anti-metastatic activity and the efficacy of chemotherapy significantly decreased in carboplatin treatment in combination with sialic in SH-SY5Y cells. Our results are consistent with the previous reports about the role of hyper-sialylation in promoting cancer development.
5.1. Conclusions
This study demonstrated that sialic acid, by inducing intrinsic anti-apoptotic pathways and SH-SY5Y proliferation, decreased the anticancer effects of carboplatin. It might be suggested that targeting aberrant sialylation could be beneficial for treating patients with Neuroblastoma. Basically, it recommended that further protein-level research need to be carried out to evaluate and support these in vitro outcomes. However, further studies are needed to clarify the molecular mechanisms and pharmacokinetics behind the drug-resistance effects of this compound.