1. Introduction
Penetrating keratoplasty (PKP) is the most successful organ transplantation in humans. Corneal graft rejection is one of the most important complications following PKP and the major cause of graft failure in the intermediate and late postoperative period (1, 2).
Following allograft PKP all the three layers of the cornea, (epithelium, stroma, and endothelium) may undergo rejection. In epithelial graft rejection, the eye is generally asymptomatic. It is usually seen early in the postoperative period with an average onset of three months. Clinically, an epithelial rejection begins at the graft-host junction in a linear pattern, which advances toward the center across the donor epithelium over several days and may last up to several weeks (3).
This type of rejection usually subsides in six to ten days and is usually self-limited. However, it's important since it may herald the onset of other types of rejection in 74% of cases. Epithelial rejection may be associated with a persistent epithelial defect; moreover, epithelial rejection rings may develop (4). Herein, we reported a new presentation of epithelial graft rejection, which responded well to steroid therapy.
2. Case Presentation
A 23-year-old man developed corneal ulcer in his left eye after photorefractive keratectomy for myopic correction. The results of smear and culture of cornel ulcer were negative and treatment with topical antibiotics initiated. After improvement of corneal ulcer, he underwent PKP for corneal scar and severe corneal irregularity. Thereafter, his best corrected visual acuity (BCVA) increased to 20/40 and corneal graft remained clear.
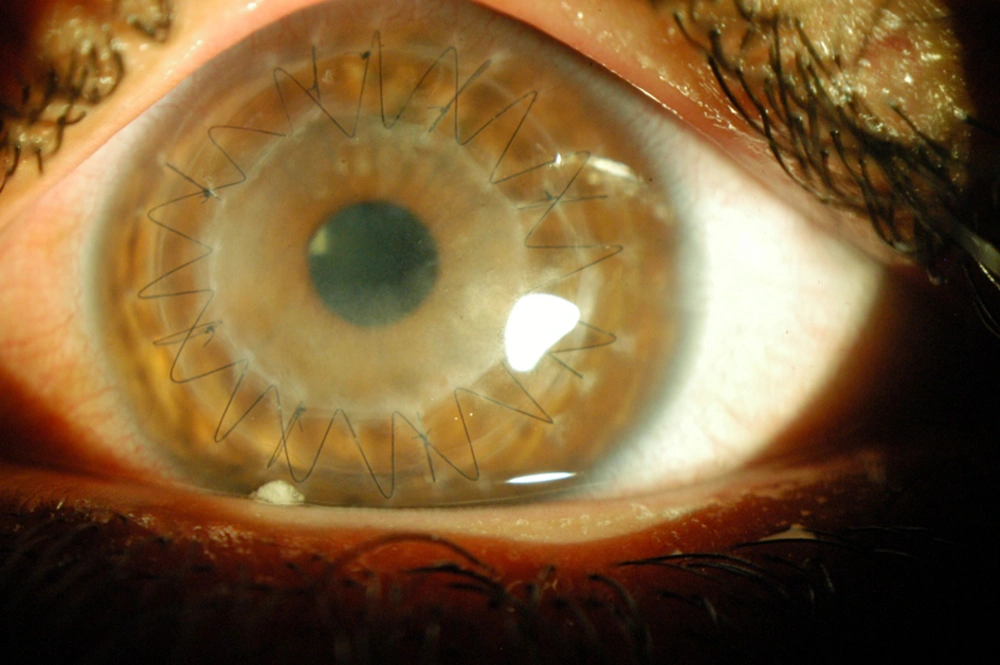
After two month, he complained of decreased vision in his left eye. Slit lamp examination revealed superficial haziness of the graft. BCVA had decreased to 20/200. Slit lamp examination revealed white, sharply demarcated, diffuse epithelial opacity in corneal graft with peripheral sparing. Cornea in between suture lines was clear, sutures were not loose and donor-recipient junction had normal appearance (Figure 1). No stromal and endothelial abnormalities were observed. Anterior chamber was clear. No corneal edema, keratic precipitates, or corneal infiltration were seen. He was treated with systemic prednisolone (25 mg, daily) and fluoromethalone eye drop (every four hours), which tapered gradually over four weeks. The density of opacity decreased after initiation of therapy and graft was clear after one month.
3. Discussion
Due to its immune privileged status, corneal graft is the most successful tissue transplantation in humans (5). About one-third of all corneal graft failures are due to graft rejection (6). The reported rate of rejection episodes varies considerably from 2.3% to 68% (7, 8). Graft survival rate after PKP is estimated to be 86% at one year, 73% at five years, and 62% at ten years, mostly because of corneal allograft rejection (9).
Corneal graft rejection is a complex immune process in which the host’s immune system recognizes the foreign antigens of the corneal graft; it leads to an efferent-afferent immune response against the allograft and finally epithelial and/or endothelial rejection line, stromal rejection band, anterior chamber reaction with keratic precipitates, and corneal edema develop (10).
If recognized early and treated aggressively with corticosteroids, most episodes of graft rejection do not cause irreversible graft failure. Each layer of the cornea may undergo rejection, with endothelial rejection being the most severe form. Typically, epithelial graft rejection begins as an elevated, epithelial ridge often near the graft-host junction and progresses centripetally, leaving a hazy irregular epithelium behind that will be finally replaced by host epithelium (3). This rejection is marked by the elevated epithelial rejection line, representing damaged donor epithelial cells. It is usually seen in the periphery and stains with fluorescein or Rose Bengal (3, 8). The hazy epithelium behind the rejection line is gradually replaced by recipient epithelium. Over days to several weeks, superficial epithelial infiltrates (Kaye’s dots) may appear near the suture lines and progress centripetally (3).
Persistent epithelial defect and epithelial rejection rings may also develop (3). In epithelial rejection, the eye is generally quiet and asymptomatic or may be mildly inflamed. Edema, keratic precipitates, and infiltrates are not seen. This type of rejection is usually self-limited and subsides within weeks as the donor epithelium is replaced by host epithelium; however, it is important due to high association with other types of rejection (3).
Our patient showed a new atypical presentation of epithelial graft rejection. It presented as a disc-shaped superficial haziness of the epithelium that was limited by the suture lines, sparing peripheral graft as well as the graft-host junction. This presentation, although different from typical linear pattern, responded well to corticosteroid therapy.