1. Introduction
The axillary fossa is a complex space containing the neurovascular bundle related to upper limb, lateral branches of the second and sometimes third intercostal nerves, many lymph nodes located in the fat and loose areolar tissue. It acts as a conduit for the vessels, nerves and lymphatics passing between the trunk and the upper limb (1).
Axillary boundary is as follows; the anterior wall pectoralis major, the medial wall serratus anterior, the posterior wall subscapularis and latissimus dorsi muscles and the lateral wall is formed only by fascia known as the axillary fascia. Axillary fascia is in continue with the chest wall fascia in proximal and with that of the upper limb in distal. This fascial layer is continuation of the posterolateral margin of the pectoralis major fascia ended in the fascia of the latissimus dorsi and acts as a tent for covering the contents of the axilla (2).
Existence of an excess slip of tendon, fascia or muscle extending from latissimus dorsi to pectoralis major or generally proximal part of the humorous seems to be the most common variation of the axillary components in men. Ramsay in 1795 first explained this variation and Langer confirmed that in 1864 and nominated it as axillary arch of Langer (3-5).
Among studies performed on the cadaver or clinical reports, almost mostly were unilateral and the incidence was variable among different populations up to 7%, but bilateral type has been reported rarely. Other names of this variation include “Achselbogen”, “axillopectoral muscle”, “axillary arch”, “Langer’s axillary arch” or “muscular axillary arch” (3-5), but in this paper we used “axillary arch” for fluency.
Latissimus dorsi muscle is like a broad aponeurosis, which extends from the spinous process of lower six thoracic vertebrae and the posterior layer of thoracolumbar fascia to the spinous process and supraspinous ligaments of all lumbar vertebrae and sacrum, posterior crest of ilium, lower 3 or 4 ribs and to some extend to the scapula (6). This aponeurosis twists upon itself and ends in the intertubercular groove in front of the pectoralis major tendon (7).
Variation in latissimus dorsi muscle may be seen in origin or insertion; for example, in the number of attachment to the thoracic vertebrae [4 - 7 or 8] or in the number of costal attachments and muscular fibers that reach to iliac crest. The axillary arch is a variable string of latissimus dorsi nearly 7 - 10 cm in length. This arch connects the upper margin of the latissimus dorsi to the tendon of the pectoralis major, the coracobrachialis or the fascia over the biceps brachii. Anyway if presents, it crosses anterior part of the axilla near axillary sheet (8). Axillary arch may be innervated by lateral pectoral nerve, medial pectoral nerve, intercostobrachial nerve or thoracodorsal nerve (3).
The presence of a variant structure in the axillary fossa could make difficulties in the access of the fossa and its contents. However, such variations may confusesur geons during operation. Therefore, recognition and considering the variations is inevitable for examination or operation (8). Clinical relevance of axillary arch has been reported in several cases. Neurovascular compression has the most clinical importance. It may also cause some problems during lymph node biopsy and lymphadenectomy in the staging and treatment of melanoma and breast cancer (1, 9, 10)
Because of the importance of these variations, in this paper we described a case of variant attachment of the latissimus dorsi muscle.
2. Case Presentation
This was a report of the most common variation in the axillary fossa, in a 45 - 50 year old white man cadaver in Mazandaran University of Medical Sciences, anatomical Sciences Department, Sari, Iran (Figure 1). After removal of pectoralis Major and minor during routine left axillary fossa dissection, we encountered an aberrant slip of fascia and muscle protracted from latissimus dorsi to pectoralis major.
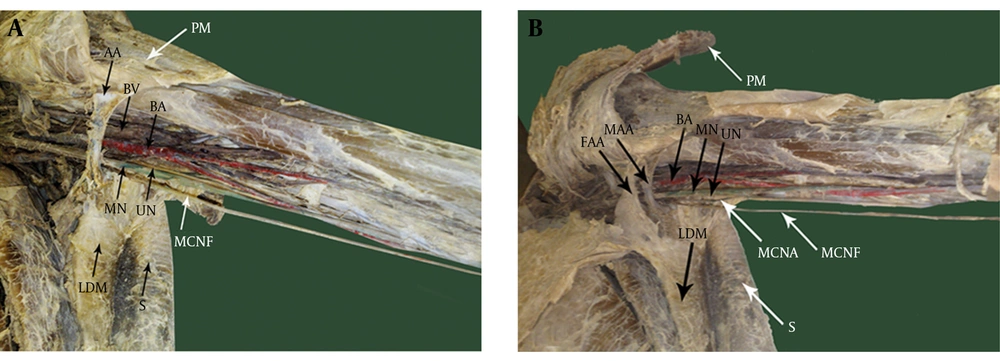
A: Axillary Arch and Other Components in the Axilla, Fascial Layer Was Cut and the Muscular Part Remained. B: Axillary Arch Shows Fascial (FAA) and Muscular (MAA) Parts of the Axillary Arch. Note That a Slip of Latissimus Dorsi Muscle (LDM) and its Deep Fascia Prolonged to Pectoralis Major (PM). BA, Brachial Artery; MN, Median Nerve; UN, Ulnar Nerve; MCNA, Medial Cutaneous Nerve of Arm; MCNF: Medial Cutaneous Nerve of Forearm; S, Skin
This muscular slip was 7 cm long and 1 cm diameter in the extremes and 7 mm in the middle. It is innervated by a branch of thoracodorsal nerve. It was prolonged from the anterior margin of latissimus dorsi, next to the insertion to pectoralis major muscle. Furthermore, the fascia of the muscular slip arrived to deep part of the fascia of pectoralis major. This axillary arch crosses the neurovascular bundle of the upper limb and the lymph nodes.
There were some vascular variations in the cadaver, but there was no other variation in the muscle. An example was lack of the cephalic vein, and the brachial artery was divided in higher distance instead of the cubital fossa.
3. Discussion
We reported a variation in axillary fossa as axillary arch with two muscular and fascial parts. The axillary arch muscle (AAM) or ‘axillary arch of langer’ (Langer’ser Achselbogen) first described in 1846 (2), is the most common variation of the axilla with an incidence of 7% - 8% (11). This arch, also called ‘the axillopectoral muscle’ is a flat muscle that arises from the anterior axillary part of the latissimus dorsi (12-14). Variations of this muscle commonly involve a bidirectional slip with one origin and one insertion. Few cases have been described with complex muscles connections inserting at multiple sites (11). Vaulted forme variations in the axilla could be divided in two groups, muscular (type I) and tendinous (type II) ones. Also there are different subtypes according to their origin, insertion and nerve supplies (15).
They may arise from the latissimus dorsi, pectoralis major, thoracic fascia or external oblique aponeurosis or even ribs and costal cartilages. They are commonly inserted at the pectoral tendon, upper humerus or coracoid process. Sometimes they may insert into the fascia of the arm and extend to flexor muscles of the arm. Occasionally it extends down as far as the medial epicondyle called as the ‘chondroepitrochlearis muscle’ (15, 16).
However, axillary arches could be classified as superficial and deep arch groups in clinic. Superficial group arches cross in front of the vessels and nerves, like as this report. In such cases, veins might be entrapped and obstruction of the axillary vein occurs. The second type arches cross the posterior or lateral walls of the axilla (2, 3). These arches usually cross only parts of the neurovascular bundle, so axillary or radial nerves may be probably implicated (3).
Anyway, the muscular arch may result in intermittent compression of the axillary vein and may lead to axillary venous thrombosis (12-14). It has also been implicated in the hyper abduction syndrome (17).
Recognition of these anomalies is important for surgeons to perform safe axillary operation (2, 9), for example in axillary lymphadenectomy, because some lymph nodes may hide under and lateral to the axillary arch if it is present.
It may also cause several surgical and medical problems such as axillary vein entrapment syndrome, establishment of lymph edema of the upper limb following breast surgery, upper limb neurovascular symptoms or even presents like an axillary mass mistaken by axillary lymph nodes (3).