1. Introduction
Salivary gland tumors represent 1% to 4% of all human neoplasias (1). Pleomorphic adenoma (PA) is the most common tumor that affects the aforementioned glands (1-3). Among salivary gland neoplasms, metastasizing pleomorphic adenoma (MPA) constitutes an extremely rare group of tumors (2, 3). Metastasizing pleomorphic adenoma has neither age or sex predilection nor any association with race or geographic location. The World Health Organization (WHO) defines MPA as a “histologically benign pleomorphic adenoma that inexplicably manifests local or distant metastasis” (4). Although apparently benign, the MPA-associated mortality could be as high as 22% (5). The most common initial tumor site in MPA is the parotid gland (74%), followed by minor salivary glands (17%) and submandibular glands (10%). Most patients (81%) with MPA have a history of at least one local recurrence of PA prior to the detection of distant metastasis. In only 17% of patients the detection of MPA resulted from the medical evaluation of a local recurrent PA. Nevertheless, many authors have reported cases of metastasizing salivary pleomorphic adenomas without prior evidence of local recurrence (6-8). The most common site for metastasis was the bone (45%), followed by the head and neck (43%), lungs (36%), and abdominal viscera (10%). Within the head and neck area, only 17% of cases metastasized to regional lymph nodes. Histologic examination of the excised tissue from the primary site and the metastases usually shows a pleomorphic adenoma without any signs of malignancy and with abundant chondromyxoid stroma (7).
2. Case Presentation
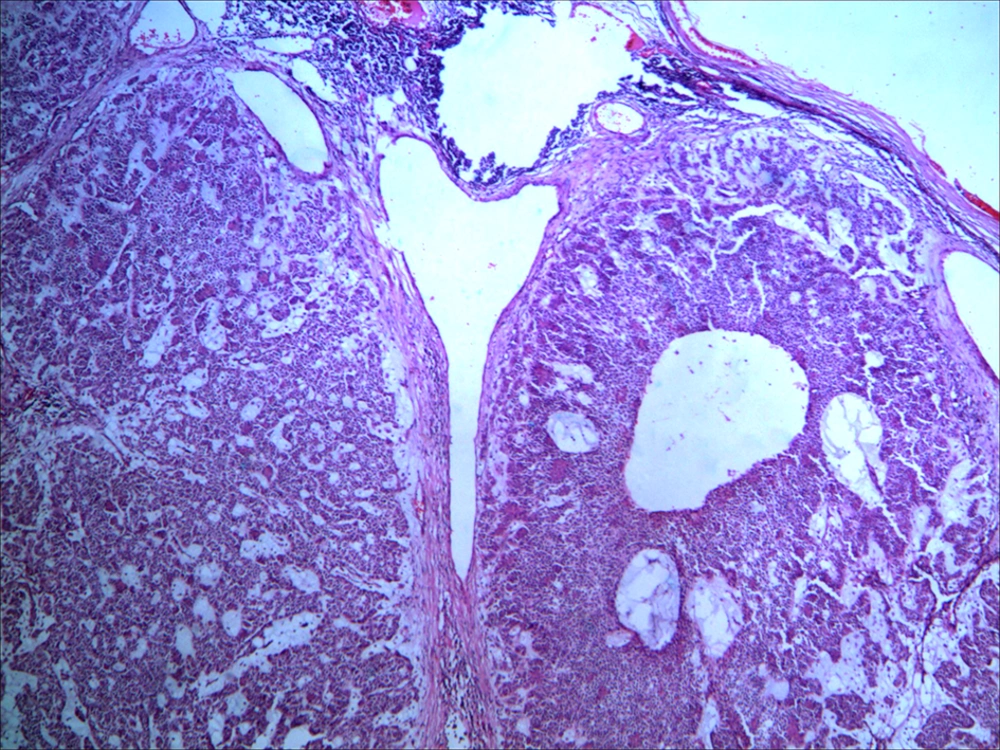
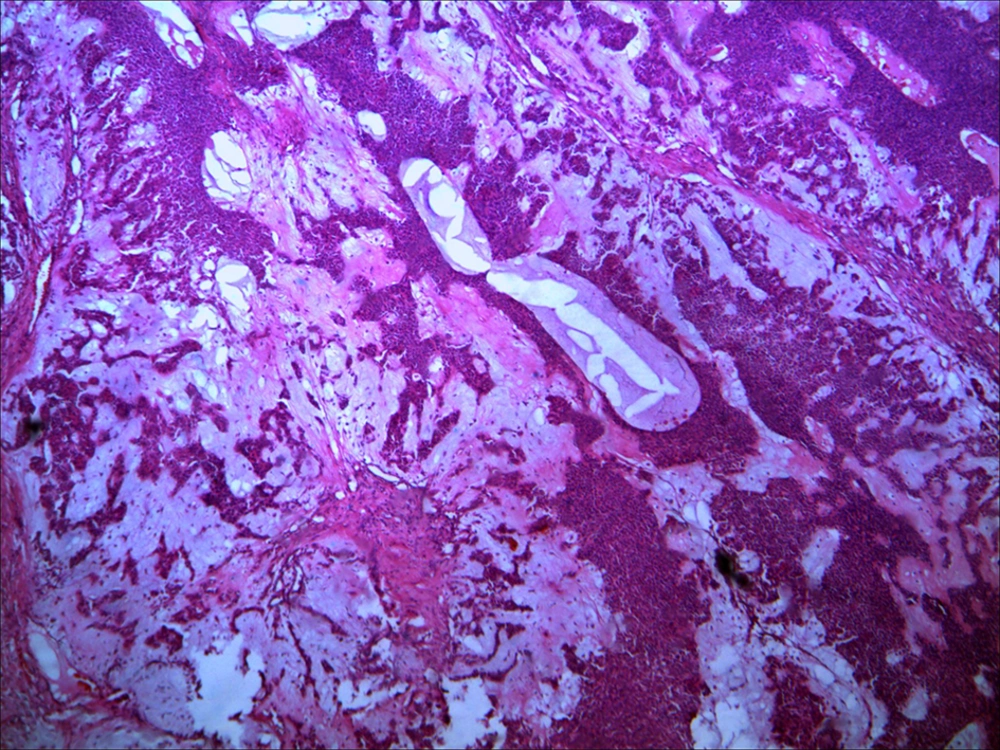
A 78-year-old male with right sided cervical lymph node and ipsilateral parotid mass from one year ago came to Imam Khomeini hospital, department of otorhinolaryngology, Ahvaz, Iran. On physical exam there is a painless firm nontender, rubbery nodule, measuring 7 × 6 × 4 cm in diameter. It was not fixed to the underlying tissues or to the overlying skin, which was normal in colour were found both within the right sided parotid and lymph node of the neck concomitantly with no pain or facial palsy was described at that time. There were no other organs abnormalities. The tumor was excised with completion parotidectomy and cervical lymphadenectomy. Histological examination of the specimen showed features of a typical benign pleomorphic. Adenoma within a lymph node and with no associated ectopic salivary gland tissue (Figure 1). Histopathologic diagnosis of the tumor of salivary gland was “pleomorphic adenoma” (Figure 2). There was no evidence of extracapsular growth, atypia or vascular-perineural involvement. Margins of the surgical specimen were free of tumour. Only scattered mitotic figures were present. No histologic characteristic of malignancy was seen in either specimen; therefore, a diagnosis of benign metastasizing mixed tumor was rendered.
3. Discussion
Pleomorphic adenoma is the most common benign salivary neoplasm (4). Although clinically and histologically it is a benign tumour, there are rare reports of metastasis to regional and distant sites, in which the metastatic foci are histologically identical to the benign primary tumour (2, 3). Benign MPA is distinguished from truly malignant pleomorphic tumors (such as carcinomas arising from pleomorphic adenomas, and carcinosarcomas) by its benign histologic features. However, there are no agreed histopathologic parameters that can differentiate a nonmetastatic pleomorphic adenoma from Mpa (4, 5, 8). It has been suggested that metastasising tumours have a higher mitotic rate than non-recurring lesions, but this theory is not universally accepted and this feature was not seen in our patient (6-9). The Patients (81%) with MPA have a history of at least one local recurrence of PA prior to the detection of distant metastasis of the tumour at the primary site is a characteristic feature of these metastasising pleomorphic adenomas; recurrence ocurring in about 90% of cases (5). There is often a long interval between the diagnosis of the primary mixed tumour and the metastasis (5, 6). Paradoxical nature of MPA, with its benign histological appearance and its metastatic spread capacity, intrigues clinicians and academic scholars. Several hypotheses have been formulated in order to explain how a histological benign tumor may produce metastasis, such as previous radiation of the primary PA or previous surgical intervention that should favor seeding and permeation of blood or lymphatic vessels by tumor cells, followed by metastatic spread (2, 7-9). However, the data in literature have shown that they are not absolute requisites for metastatic disease to occur (2, 4, 5). Tumour enucleation should never be performed as it increases local recurrence rate. Local recurrence may be the first step in the dissemination of these neoplasms and therefore radical surgery and radiotherapy should be considered in these cases (6, 7). Clinical rather than pathologic evidence seems to justify inclusion of metastasizing salivary pleomorphic adenoma in the group of low-grade malignant salivary tumors (7-9).