1. Background
Polycystic Ovary Syndrome (PCOS) is a common disease in young women that is associated with infertility and other complications such as obesity, hirsutism and insulin resistance and also the disorder that mostly is specified with oligomenorrhoea or amenorrhea with clinical evidence laboratory of hyperandrogenemia (1-3). It has been recognized that a significant number of obese women that are afflicted with this disease are also suffering from the hyperinsulinemia (4). The most common cause of hirsutism and hyperandrogenism is PCOS (5). The origin of this disorder is probably poly-gene or multifactorial or both of the following (6). Criteria for diagnosis include major criteria of the chronic anovulation, hyper androgenic, clinical signs of hyper androgenic (7, 8). Also, criteria subsidiary of the insulin resistance, hirsutism and obesity begin around menarche, an increase of Luteinizing Hormone (LH) to Follicle Stimulating Hormone (FSH), lack of periodic ovulation with hyperinsulinemia and ultrasound evidence of PCOS (9, 10). For its treatment, the various drugs were used that the most effective of them is considered to induce pregnancy (11, 12). From these drugs can be pointed to the Clomiphene Citrate (CC). This agent acts as an antagonist of the estrogen receptor of the hypothalamus and causes increasing of the gonadotropin secretion and also followed by LH, FSH increases. This increase can be caused by increased gonadotropin or increased sensitivity of the pituitary to the gonadotropin (5, 6). In many studies, the reduced effect of this drug has been associated with some hormonal changes before treatment; therefore, FSH was reduced and the levels of LH and testosterone were increased and also the insulin level was decreased, which can cause to decrease the effect of this drug (13, 14). Increases or decreases in estradiol can cause inhibition of LH secretion and subsequent inhibition of ovulation and thus is expected to improve the effectiveness of CC (15).
2. Objectives
In this study, serum levels of estradiol, insulin, FSH and LH were measured in patients with PCOS before receiving CC. It was then checked whether the levels of these hormones in predose had any effect on the efficacy of this drug.
3. Materials and Methods
3.1. Study Design
This analytic case-control study was carried out on patients with PCOS admitted for undergoing superovulation due to nontubal infertility (ovulatory disorders, early-stage endometriosis, mild male factor and idiopathic infertility) to the obstetrics and gynecology ward of Imam Khomeini Teaching Hospitals in Ahvaz City, Iran, from December 2012 to December 2013. All procedures met international guidelines and the institute research ethics and animal care and use committee of Ahvaz Jundishapur University of Medical Sciences (AJUMS). The study inclusion criteria consisted of women of reproductive age with PCOS, absence of uncontrolled diabetes and lack of antidiabetic drugs and exclusion criteria included lack of patient cooperation. Patient assessment included demographic information as well as medical and gynecologic histories with physical examination and routine laboratory screening (including Body Mass Index (BMI), Complete blood count (CBC), Pap smear, Thyroid stimulating hormone (TSH), Prolactin (PRL) and viral serology). To evaluate the serum estradiol, insulin, FSH and High- Density Lipoprotein (HDL), LH and Glucose Tolerance Test (GTT), blood samples of cases were taken before taking CC (Pergonal; Serono) for controlling ovarian hyperstimulation. The parameters were measured by an Enzyme-Linked Immunosorbent Assay (ELISA) reader. The time of processing of these hormones is on the day 3 of the menstrual cycle. After that, CC was given up to 3 months and then, the percentage of people who were pregnant or had improved ovulation (which was determined by ultrasound) was calculated.
3.2. Statistical Analysis
To analyze the data, SPSS 19 statistical software (USA) was used and examined accurately by t-test, chi-square, Fisher's exact test and odds ratio for abnormal estradiol, insulin, FSH and HDL, LH and GTT in the patients with PCOS. For all other outcomes, a nominal P value of P < 0.05 was considered significant.
4. Results
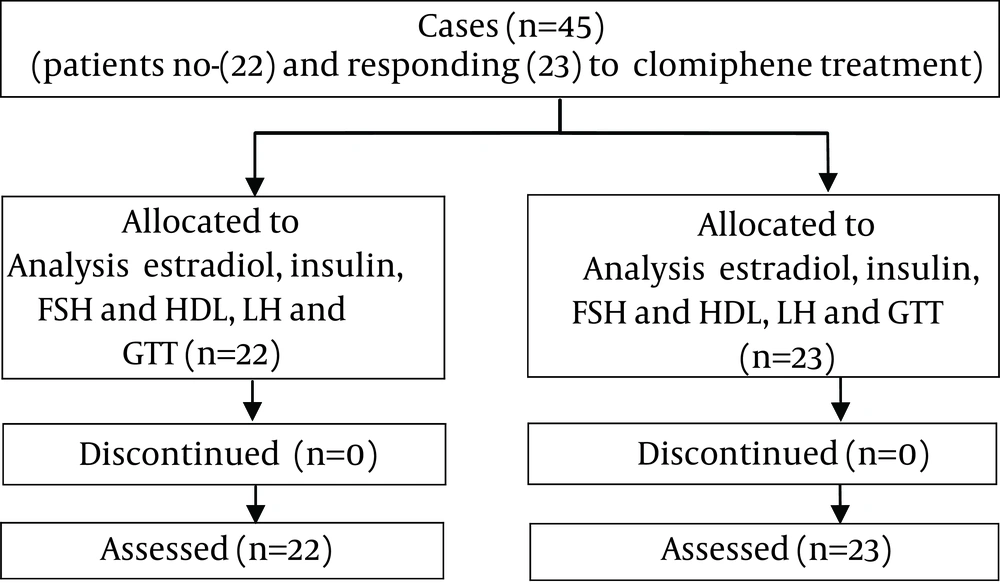
Outcome data were available for 100% of the randomized women. Forty-five PCOS cases were admitted for undergoing superovulation due to nontubal infertility (ovulatory disorders and idiopathic infertility). All forty-five PCOS cases were found to be identical in the maternal age (19 to 35 years) at admission, social and economical situation, BMI, types of infertility, duration of infertility, number of previous trial, duration of stimulation, the type of procedures used, the total dose of gonadotropin injected, number of retrieved follicles and semen analysis (Total motile sperm count (TMC), motility and morphology of sperm) (Table 1). The cases based on the responsibility of them to the CC (Pergonal; Serono) therapy were grouped into two categories. None of the patients was lost to follow-up (Figure 1). The ovulation, after taking CC, was done in 42.2% of the cases (Table 1). However, the clinical pregnancy rate was not more significant in cases responded well to CC compared to resistant cases (P ≥ 0.387). There were no subjects of severe Ovarian Hyperstimulation Syndrome (OHSS). Also, the overall clinical pregnancy rate was 17.8% (Table 1).
| Variables | Groups | ||
|---|---|---|---|
| No-Treated | Treated (Mean ± SE) | P Value | |
| Age, y | 28.5 ± 3 | 31.9 3 | 0.963 |
| BMI, kg/m2 | 27.2 ± 5 | 28.4 ± 0.69 | 0.383 |
| Kind of sterility, Primary | 19 (57.6) | 16 (48.5) | 0.97 |
| Kind of sterility, Secondary | 14 (42.4) | 17 (51.5) | 0.241 |
| Duration of infertility | 5.03 ± 4.6 | 6.94 ± 6.8 | 0.050 |
| Number of follicles | 5.5 ± 1 | 3.8 ± 0.4 | 0.069 |
| Pregnancy rate | 3 (9.9) | 4 (12.1) | 0.387 |
Maternal Demographic and Clinical Characteristics in Women Who Admitted to the Department Were Comparable in the Two Groups a
There was a significant difference in biochemical parameters such as the mean serum FSH (4.4 ± 1.2 vs. 6.6 ± 1.5, P ≥ 0.0001), LH levels (11.6 ± 2.5 vs. 8.1 ± 3.2, P ≥ 0.008) between the patients who did not respond and responded to CC treatment, respectively. Moreover, the mean serum GTT level in the group resistant to CC treatment (nonresponders) was higher than that of the group who responded to CC treatment (responders) (111 ± 11.6 vs. 96.5 ± 9.7 respectively, P ≥ 0.024) (Table 2). However, no meaningful correlation was observed among the mean serum estradiol (41.8.1 ± 7.9 vs. 46.4 ± 8.2, P ≥ 0.478), insulin (18.3 ± 3.6 vs. 14.4 ± 4.8, P ≥ 0.882) and FBS (94.4 ± 1.2 vs. 86.6 ± 1.5, P ≥ 0. 1) in the group resistant to CC treatment (nonresponders) in comparison to the group responded to the CC treatment (Table 2). Also, no significant difference was observed between the levels of mean HDL and the rate of ovulation in both groups (P ≥ 0.118) (Table 2). When all of the women were stratified according to their BMI (BMI ≤ 25 kg/m2 and BMI > 25 kg/m2), there were significant differences in the ovulation (P ≥ 0.001) and the rate of pregnancy (P ≥ 0.029) between the groups (Table 3).
| Parameters | Control Group | Treated Group | P Value |
|---|---|---|---|
| Estradiol | 41.8.1 ± 7.9 | 46.4 ± 8.2 | 0.478 |
| Insulin | 18.3 ± 3.6 | 14.4 ± 4 | 0.882 |
| FSH | 4.4 ± 1.2 | 6.6 ± 1.5 | 0.0001 |
| FBS | 94.4 ± 1.2 | 86.6 ± 1.5 | 0.1 |
| LH | 11.6 ± 2.5 | 8.1 ± 3.2 | 0.024 |
| GTT | 111 ± 11.6 | 96.5 ± 9.7 | 0.024 |
| Vaiables | Groups | ||
|---|---|---|---|
| BMI ≤ 25 kg/m2 | BMI > 25 kg/m2 | P Value | |
| Ovulation | 4.4 (52.5) | 3.9 (47.5) | 0.001 |
| Pregnancy rates | 4 (57.2) | 3 (42.8) | 0.029 |
The Variety of All of the Cycles (n = 66) Were Categorized by the Mean BMI into Group BMI ≤ 25 kg/m2 and Group BMI > 25 kg/m2 a
5. Discussion
The results of the present study show that CC treatment is capable of inducing follicular maturation and ovulation, followed by increasing pregnancy rate in the PCOS patients. However, whether the quality of the follicles released in these forms is optimal stays to be clarified. These findings ,with respect of studies of Adashi (4) and Bergh et al. (7), are also in accordance with other studies done by Shobokshi et al. (8), Brown et al. (16) and Moolenaar et al. (17) reported that CC plays a major role in the development of the reproductive outcome. The results of Shobokshi et al. (8) study showed that the CC treatment was effective and well-tolerated in the induction of metaphase II (MII) oocyte and ovulation in patients undergoing Intrauterine insemination (IUI) treatment. Brown et al. (16) have also found similar clinical outcomes with this drug during IUI or induction ovulation treatment in normal responder patients. Yazici et al. (18) obtained the same number of mature oocytes and similar pregnancy rates from women treated with CC. Moreover, Kelekci et al. (19) reported that low dose of CC is more efficient to achieve optimal oocyte maturation, with fewer incidences of OHSS, than a high dose of this drug. Brown et al. (16) observed that the CC at the highest dose can increase vascular permeability (VP) and expression of Vascular endothelial growth factor (VEGF) that may be running the risk of provoking OHSS or PCOS. The present study showed that the reproductive outcome i.e. ovulation and pregnancy rates in the patients with BMI < 25 kg/m2 was more pronounced than the patients with BMI > 25 kg/m2 BMI. Hull et al. (20) reported that of the 708 pairs who need infertility treatment, 21% were lack of ovulation and also more than 30% of other had other ovulation disorders. Crosignani et al. (21) reported that the weight loss was significantly reduced ovarian volume and also their micro follicles. Additionally, of the 27 patients, 18 had regular periods and 15 cases had ovulated spontaneously and also 10 patients became pregnant. In contrast, other studies have reported that cycle parameters, such as clinical pregnancy, implantation and the occurrences of moderate and severe OHSS were also found not to be significant in both higher and lower BMI, infertility duration and mean number follicles groups (22, 23). The present study also identified that the mean levels of estradiol were identical in all of the PCOS cases that were responders and nonresponders to the CC treatment; however, there was a significant difference in serum levels of FSH and LH between the patients who were responders and nonresponders to CC treatment that it could be a supplementary step towards understanding the advantages and disadvantages of the CC treatment. Although, the events initiated by the mid-phase surge of LH and FSH are presented together, certain amounts of LH and FSH may be needed in order for these events to happen (24). Also, it was shown that CC induces nuclear maturation as well as follicular maturation (17). This may also be the case in humans where a time- or dose-dependent phenomenon leads to the initial elevation in progesterone 12 hours before the LH surge, the final maturation of the oocyte 32 hours after the surge and ovulation 36 hours after the LH surge (25). Thus, it would be logical to determine the optimal CC dose to induce ovulation. Properly, the serum levels of FSH and LH act as acute phase reactants in nontubal infertility i.e. ovulatory disorders, early-stage endometriosis diseases (26). However, there was a controversy about serum estradiol in this problem that performs as an acute reactant (27, 28). It was reported that estradiol can be found in dependent phase of sex cycle level in healthy women because of it releases from follicular cells, but its level was increased in PCOS diseases, resulting to elevated FSH and LH receptors in follicular cells (29). Indeed, the serum estradiol concentration represents the amount of mature follicle storage that is in the ovary (30). Although, serum estradiol represents FSH and LH concentrations and its low level indicates maturation follicular deficiency, but increased serum estradiol doesn’t indicate that the FSH and LH levels are more than normal (31). The present study showed that there was a meaningful relation among serum insulin and FBS concentrations and GTT and its severity in PCOS cases, which confirming a role for pancreas injury and also alteration of homodynamic in PCOS. Prior researches have come to different results about whether the abnormal serum insulin and FBS concentrations and positive GTT are raised in result to PCOS (28). In conclusion, our results revealed that a cause-effect relationship between the concentration of serum FSH and LH and PCOS may in fact exist. The follow-up controls show that there is a strong relation between BMI and positive GTT and PCOS syndrome. At present we can assert that evaluating the serum levels of FSH, LH, GTT and BMI in PCOS women that are recommended to use CC for inducing maturation and ovulation of oocytes as a part of reproductive elementary routine produced a reliable way to predict maturation and ovulation status.