1. Introduction
Hydatid disease in the brain accounts for only 1% - 2% of all cases caused by Echinococcus granulosus infections. Cerebral hydatid cysts are usually located in the supratentorial region and are seldom found in the infratentorial region (1). Extracranial and spinal hydatid cysts are very rare. Hematogenous spread is the most common route of dissemination of the ova to the central nervous system and the cysts are usually located along the distribution area of the middle cerebral arteries, often in the parietal lobe (2). The majority (70% - 80%) of intracranial hydatid cysts are found in children (3). Brain hydatid cysts are usually solitary but, on rare occasions, multiple cysts might be encountered. While multiple cysts might be primary, they might also be secondary and related to the rupture of primary cyst (4). Due to slow growth of the cyst, patients usually present with a large cyst at the time of diagnosis. Typically, cysts initially manifest as focal neurologic deficits or symptoms related to increased intracranial pressure (5). The optimal management of intracranial hydatid cysts is intact surgical removal of the cyst.
2. Case Presentation
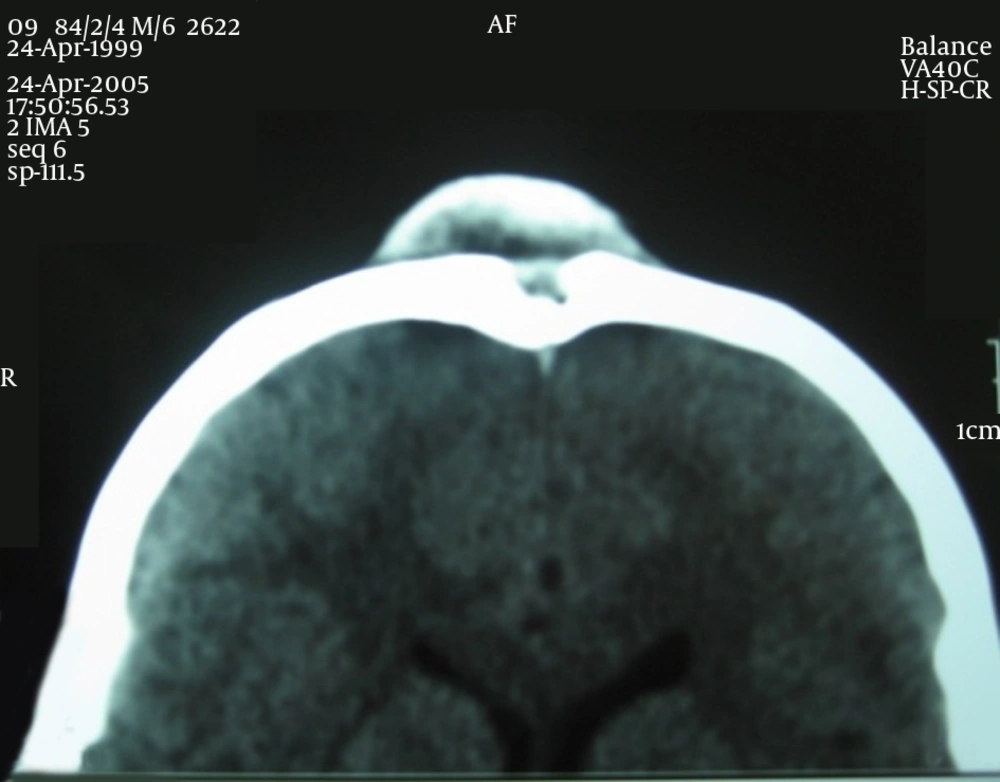
2.1. Case 1
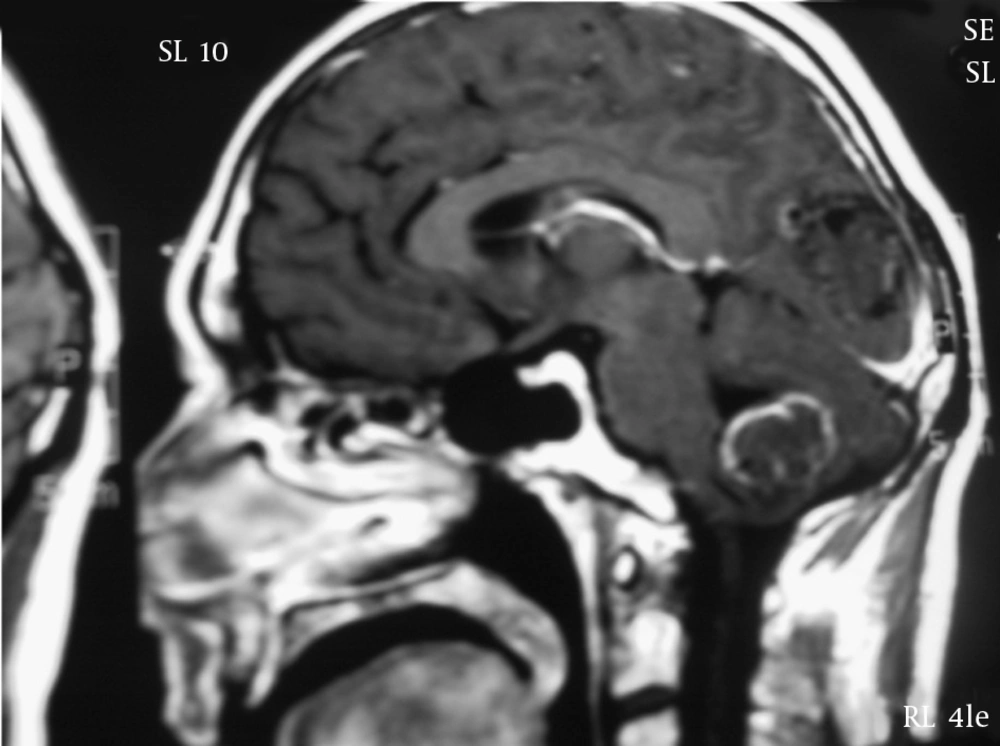
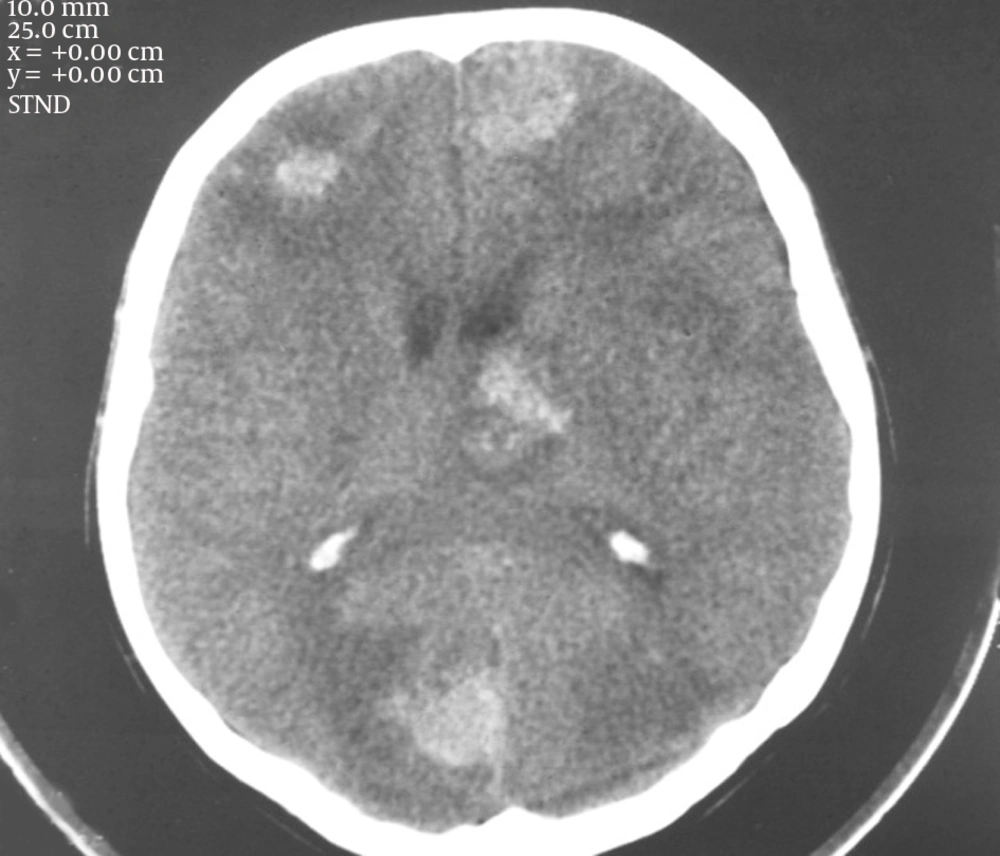
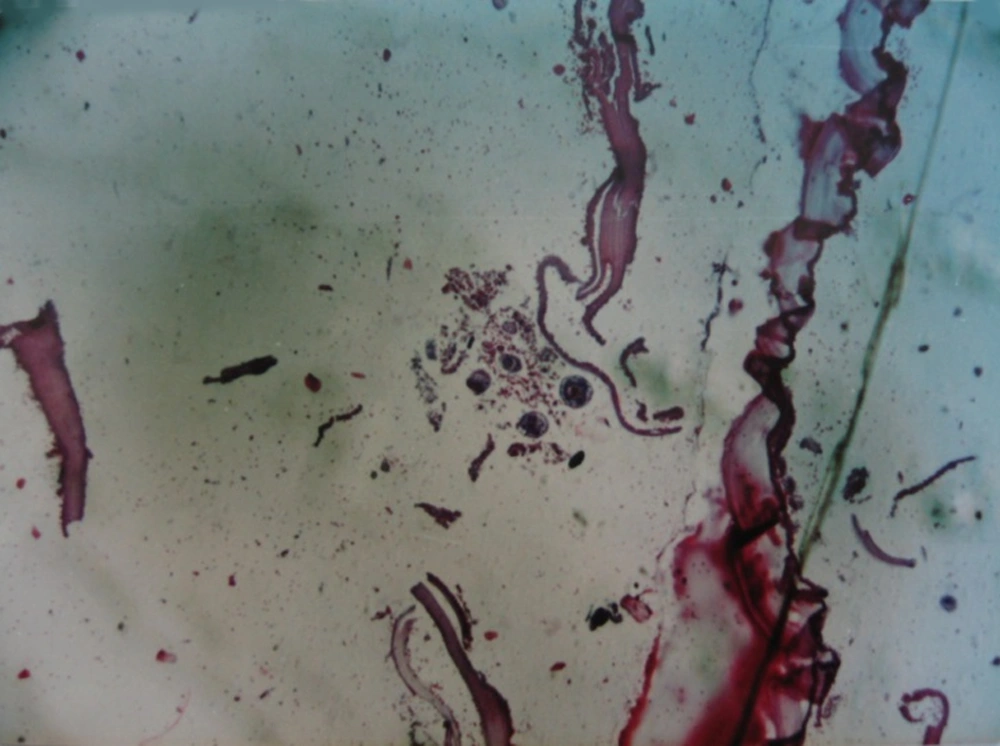
The first patient was a 45-year-old man who presented with sudden onset of severe headaches accompanied by nausea, vomiting, and weakness of the lower extremities. The patient’s Glasgow coma scale was 14/15. A brain computed tomography (CT) scan and magnetic resonance imaging (MRI) showed multiple supratentorial and infratentorial lesions similar to brain metastasis; however, no other lesions were observed in the body. The patient was taken to the operating room and multiple cysts were removed with intact capsules. Post-operative pathologic examination showed infected hydatid cysts of the brain. Patient recovery was uneventful.
2.2. Case 2
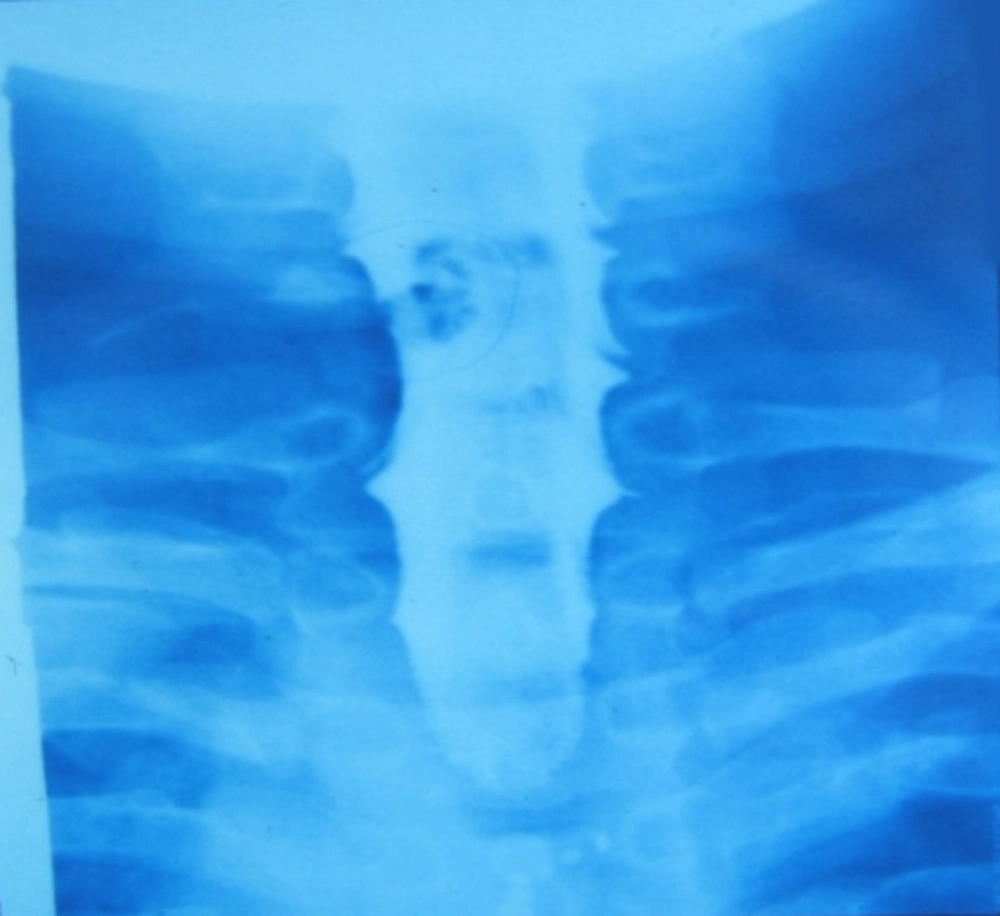
A 23-year-old man presented with right-hand C6 radiculopathy and interosseous muscle atrophy lasting six months. Cervical myelography showed extradural mass defects at the C5 - C6 foramen consistent with neurinomas. During operation, a large hydatid cyst measuring 65 × 30 mm was discovered and removed.
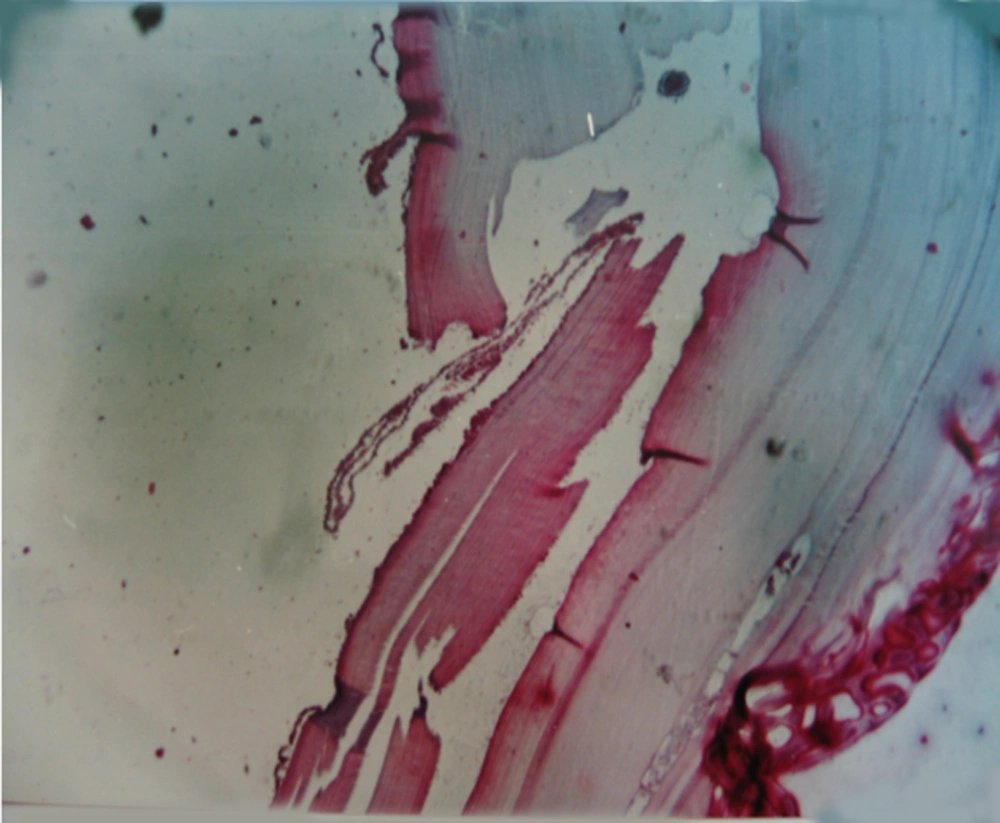
2.3. Case 3
A 6-year-old boy presented with a frontal skull mass that had been growing gradually, but had no other accompanying symptoms. Histiocytosis was suspected; however, after excision, the mass was found to be an infected hydatid cyst.
3. Discussion
The normal life cycle of Echinococcus species involves two hosts. Adult parasites live in the intestinal tract of carnivorous, definitive hosts (such as dogs) and produce eggs that contaminate vegetables and water through expelled feces. These eggs are then be ingested by herbivorous, intermediate hosts (such as sheep or humans) and become larvae that then travel through the intestinal wall of the intermediate host. The larvae then enter the blood stream, seeding organs as they travel through the blood stream. Therefore, in humans, hydatid disease mainly affects the liver and accounts for approximately 75% of the cases, followed by the lungs in 15% of cases, the brain in 2%, the vertebrae in 1%, and the orbital cavity in 0.2% - 0.8% (6, 7). It takes about 6 months from the time of initial implantation for a given cyst to become fertile. However, some cysts never produce broad capsules, while others may become sterile either through superimposed bacterial infection or through death and ensuing calcification (8). The cysts will grow at different speeds depending on tissue resistance and it is estimated that, in the brain, it takes 5–16 months for the cyst to grow 1 cm in size (6). Due to the slow growth rate, patients develop symptoms late and the cysts are usually large at the time of presentation (9).
A large published study found that headaches and motor deficits were the predominant symptoms in patients with intracranial hydatidosis, whereas back pain and spinal cord compression syndrome were the most frequently reported clinical presentations in patients with spinal hydatidosis (10).
Imaging studies, such as CT scans and MRI, are the diagnostic modalities of choice and are able to identify the intracranial or spinal cysts. CT scans usually show a round cystic lesion without per focal edema and rim enhancement (11). The cyst fluid is generally dense or slightly hyper-dense compared with cerebrospinal fluid. Cyst calcification seldom occurs. On T2-weighted MRI, the hydatid cyst appears as a cystic lesion with a hypointense halo around the cyst capsule. Accompanying cysts in other organs, especially the liver, may also provide a helpful clue for diagnosis (12).
Surgical removal is the primary method of treatment. Due to the challenges of removing a brain cyst, preoperative diagnosis can be invaluable. These cysts are usually large at the time of operation and have a thin capsule. They also might have adhesions and might be located deep in or close to the ventricular walls requiring careful dissection. In the case of successful removal of the cyst, the patient prognosis is quite good.
Hydatid cysts should be considered when a large brain cyst is encountered. Slow growth, the patient’s background, and a history of recent travel might provide helpful clues for diagnosis. Preoperative diagnosis and meticulous surgical dissection during surgery might ensure complete patient recovery.